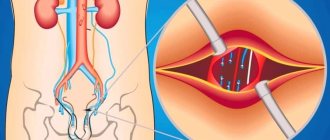
Varicocele is a varicose dilation of the vessels of the testicle or spermatic cord. The pathology impairs the functioning of blood vessels, increases venous pressure in the genital area, and often causes infertility in men.
The course is often asymptomatic or symptoms are not clearly expressed. In this case, varicocele can be diagnosed during a routine examination or when determining the causes of infertility.
Causes:
- genetic predisposition to varicose veins;
- inflammatory processes in the body;
- regular physical activity, namely lifting heavy objects;
- the presence of tumors in the groin;
- excess body weight.
Varicocele causes
Varicocele does not cause pain, and only occasionally can be manifested by aching or pulling sensations in the testicle . This is the insidiousness of this disease, because it can be difficult to convince a patient who is not in pain to go under a knife (although today it is, of course, not a knife, but a microsurgical instrument ). But it is necessary to undergo surgery, because due to varicose veins of the spermatic cord, blood stagnation occurs in the testicle , its blood supply suffers and the local temperature rises. All these factors, acting gradually and imperceptibly, lead to disruption of the process of formation and maturation of sperm, and in advanced cases - to a decrease in the size and atrophy of the testicle . The sooner varicocele , the greater the chance of preventing negative consequences for the man’s body.
In patients with varicocele, pathological changes in the spermogram are often detected. The most common are oligozoospermia (a decrease in the concentration of sperm to less than 15 million per ml), asthenozoospermia (a decrease in the concentration of progressively motile sperm to 32% or less), teratozoospermia (a large number of pathological forms of sperm, exceeding 96%). Varicocele is characterized by damage and fragmentation of sperm DNA .
Several studies in recent years have confirmed the relationship between varicocele and decreased testosterone levels and erectile dysfunction .
Thus, in 2011, a group of Indian scientists led by Sathya Srini V. published the results of treatment of 200 patients with hypogonadism and erectile dysfunction in combination with varicocele. Some of these patients received hormone replacement therapy, while others underwent surgical treatment of varicocele. In 78% of patients who underwent surgery to eliminate varicocele, normalization of testosterone levels was achieved with improvement in erectile function. Similar results were demonstrated by the Polish urologist D. Paduch. In his study of infertile men with varicocele and hypogonadism, 76% achieved normalization of testosterone and improvement in sexual function after surgical treatment of varicocele.
Complications
The main thing that patients suffering from testicular varicose veins need to understand is the serious situation with the appearance of offspring. Infertility can become a sad complication of varicocele, so you should not delay going to the clinic for diagnosis and treatment. Doctors from the Global Clinic Center can provide qualified assistance. Statistics show that patients diagnosed with varicocele in 60 cases out of a hundred are faced with the problem of sperm dysfunction. 40% of men with testicular varicose veins become infertile.
Degrees of varicocele
Varicocele grades (according to the criteria of the European Association of Urology):
| STAGE | CHARACTERISTIC |
| Subclinical varicocele (0) | non-palpable (even with the Valsalva maneuver) dilation of veins, determined only using Doppler ultrasound |
| First stage varicocele | expansion palpable during the Valsalva maneuver, disappearing with rest |
| Second stage varicocele | expansion palpable at rest and during the Valsalva maneuver, but not visually detectable |
| Third stage varicocele | visually detectable dilatation, determined both at rest and during the Valsalva maneuver |
The second and third stages may be accompanied by a decrease in size (hypotrophy) of the corresponding testicle.
History of the disease
Varicocele is a disease with deep historical roots. The first mention of the problem dates back to the 16th century and is associated with the name of Paré, a famous surgeon of the Renaissance. He drew attention to the pathology of the venous vessels near the male testicle. Many medical historians speak of the involvement of Hippocrates and Celsius in establishing the facts about this problem. The topic of varicocele is very closely related to infertility. In the 19th and 20th centuries, scientists confirmed the possibility of curing male infertility in direct proportion to the elimination of testicular varicose veins.
TREATMENT OF VARICOCELE
Varicocele surgery
Varicocele in men treatment
As I already mentioned, conservative methods of treating varicocele are ineffective . A weak and stretched vein wall cannot be strengthened with medications. Therefore, the only effective treatment for varicocele is surgery. There are various options for operations for varicocele . Dilated veins can be ligated in the inguinal canal, above or below it. An endovascular approach is possible - embolization and sclerosis of dilated veins. However, the “gold standard” is microsurgical infrainguinal (subinguinal) ligation - the Marmara operation. Let's consider the features of each of these operations used to treat varicocele .
Preventive measures
An annual visit to the urologist, even in the absence of any complaints or symptoms, in combination with a healthy lifestyle, decisive and unconditional cessation of bad habits (primarily smoking) and active sports is the best set of preventive measures at any age. You should also pay attention to the functioning of the gastrointestinal tract, and take care to exclude fatty, fried and spicy foods from your diet. Clothing should be comfortable and not constrict the genitals. It is important to remember that hypothermia of the body is an additional provoking factor for the occurrence of varicocele or its progression.
How to treat varicocele
Operation Palomo
In this operation, a 5-6 cm long incision is made in the lower lateral part of the abdomen, above the inguinal canal. In this place, the testicular vein is usually a single trunk, running along with the testicular artery and lymphatic vessels. The surgeon isolates, ligates and cuts the vascular bundle as a single block. General or spinal anesthesia is most often used. The disadvantage of the Palomo operation is the intersection of the testicular artery that supplies the corresponding testicle, which can worsen its functional state. The intersection of lymphatic vessels can lead to the formation of hydrocele (hydrocele). Recovery and rehabilitation after Palomo surgery takes about 2 weeks.
Operation Ivanissevich
The length of the incision is approximately the same as during the Palomo operation, but the incision itself is made lower, directly in the area of the inguinal canal. The spermatic cord (containing dilated veins) lies quite superficially in this place, which makes it possible to isolate it. Typically, the operation is performed under general or spinal anesthesia, although local anesthesia is also possible.
During the Ivanissevich operation, the surgeon tries to preserve the testicular artery and lymphatic vessels, but the lack of optical magnification makes this task difficult. In case of ligation of the artery and lymphatic vessels, the complications described above may occur (testicular atrophy, hydrocele formation). The recovery period after Ivanissevich's surgery lasts about 2 weeks .
Operation Marmara
Marmara operation (subinguinal microsurgical ligation of the veins of the spermatic cord). This technique was first described by American urologist Joel Marmar in 1985. Through a small (about 2 cm) skin incision in the groin area (below the inguinal canal), the spermatic cord is isolated. Using optical magnification (operating microscope or binoculars) and microsurgical techniques, the elements of the spermatic cord (vas deferens, testicular artery, tributaries of the internal spermatic vein and lymphatic vessels) are separated. Venous vessels with a diameter of more than 2 mm are ligated (ligated) and divided. All other elements remain intact. The operation ends with the application of a cosmetic suture.
In 1992, another American urologist-andrologist Mark Goldstein modified the Marmara operation, proposing to cross not only the branches of the internal spermatic vein, but also the veins of the scrotum (branches of the external spermatic vein and gubernacular veins), for which it is necessary to remove the testicle into the surgical wound. The Goldstein modification is still actively used by urologists around the world, especially for recurrent forms of varicocele.
The Marmara operation can be performed under general or spinal or local anesthesia. The minimal incision length and microsurgical technique make it possible to perform this operation on an outpatient basis, without hospitalization.
In most cases, the patient can leave the clinic within 1-2 hours after surgery. Complications during the Marmara operation are much less common than with other types of operations used for varicocele. The functional and cosmetic results of Marmara surgery are also significantly better than other techniques. The number and motility of sperm increases to a greater extent. It is natural that the Marmara operation is currently considered as the “gold standard” for the surgical treatment of varicocele.
Scrotal access
Varicose testicular veins can also be divided at the level of the scrotum. Through a small incision of about 1-2 cm, the spermatic cord is isolated, followed by the intersection of varicose veins. The main stages of the operation correspond to the Marmara technique . The main difficulty with scrotal access is that the internal spermatic vein at the level of the scrotum is represented by a network of veins of different sizes, forming a pampiniform (or pampiniform) venous plexus. To achieve a good effect, it is necessary to cross each of these branches, which, of course, increases the operation time. The scrotal approach is currently rarely used for the treatment of varicocele.
Laparoscopic ligation of the testicular vein
Like any other laparoscopic surgery, ligation of the testicular vein is performed through punctures in the anterior abdominal wall. The operation is performed only under general anesthesia. Instruments and an optical system are introduced through punctures into the abdominal cavity. The testicular vein is isolated near the internal opening of the inguinal canal, metal clips are applied to it, and the vein is divided. The functional results of laparoscopic surgery for varicocele are generally close to the results of the Ivanissevich operation.
The postoperative period is easier than during the operations of Palomo and Ivanissevich , punctures in the abdomen heal quite quickly. Typically, the patient is discharged home the next day after laparoscopic ligation. The only advantage of laparoscopic surgery for varicocele, in my opinion, is the ability to cross the testicular veins on both sides (for bilateral varicocele) through the same access. The disadvantages of the laparoscopic approach are the need for general anesthesia, as well as the risk of complications associated with the introduction of instruments into the abdominal cavity.
Testicular vein embolization for varicocele
This technique is the least invasive among all those used to treat varicocele . The absence of an incision allows embolization to be performed under local anesthesia (or without anesthesia at all!). Naturally, there is no need for seams. A thin catheter with a flexible guide is inserted through a needle into the femoral vein. Contrast is injected through the catheter into the vasculature, and the location and movement of the guidewire and catheter are monitored using fluoroscopy. The catheter is passed retrogradely (from the renal vein towards the testicle) into the internal spermatic (testicular) vein. The structure and features of the testicular vein are assessed, and possible additional branches and tributaries are identified. After this, a coiled spiral is inserted through the catheter into the lumen of the vein. In the lumen of the vein, the spiral expands, firmly pressing against the walls of the vein and fixing itself inside. Then an embolic substance is injected into the lumen of the vein, completely closing the lumen of the vein. A control study of blood flow through the vein is performed. If there is no blood flow, the operation is completed.
The patient can leave the clinic within two hours after the operation . Recurrence of varicocele after embolization is very rare. Another advantage of embolization for varicocele is that during the procedure, fluoroscopy of the veins is performed, which makes it possible to diagnose various anatomical anomalies, additional branches connecting the testicular vein with the vein of the same name on the opposite side, and other vascular features leading to relapses of varicocele. In this regard, embolization may be particularly effective in cases of recurrent varicocele. Like any method, testicular vein embolization is not without its drawbacks.
One of the significant ones is the need to administer a contrast agent (usually the same as is administered during computed tomography). Some people have an allergic reaction to contrast and cannot undergo embolization. In addition, the administration of contrast is contraindicated in renal failure. Therefore, before this operation, the blood creatinine level must be checked.
Another limitation for embolization is right-sided varicocele. Right-sided localization is uncommon with varicocele. But, due to anatomical features, inserting a catheter and guide into the right testicular vein is often very difficult. Therefore, for right-sided (or bilateral) varicocele, it is better to resort to surgical treatment methods rather than embolization.
The high cost and relatively low availability of embolization are also of particular importance. The cost of embolization for varicocele, as a rule, is several times higher than the cost of surgical treatment (including the Marmara operation). This is due to the use of expensive disposable consumables and the need to work in an endovascular operating room equipped with high-resolution fluoroscopic equipment (angiograph). Embolization is a highly operator-dependent technique, the effectiveness and safety of which largely depends on the surgeon (human factors).
Complications from testicular vein embolization are rare . These include an allergic reaction to contrast, impaired renal function, bleeding from the puncture site, and perforation of the vein wall. A rare specific complication is migration (displacement) of the installed coil and its movement along the vascular bed with the occurrence of embolism in various organs.
Comparison of different operations for the treatment of varicocele :
| Cut length | Anesthesia | Rehabilitation period | Relapse rate | |
| Operation Palomo | 5-6 cm | spinal | 2 weeks | 29 % |
| Operation Ivanissevich | 5-6 cm | spinal | 2 weeks | 13,3 % |
| Operation Marmara | 2 cm | local/general | 7-10 days | up to 4% |
| Laparoscopy | 3 punctures | anesthesia | 5-7 days | 3-7 % |
| Embolization | No incision | local | 1 day | to 10 % |
, in accordance with the recommendations of the European Association of Urology , I perform on my patients the most modern operation for varicocele - microsurgical subinguinal ligation of varicose veins according to Marmar, and I have extensive experience in this operation.
Treatment of varicocele without surgery
Many of my patients, who are faced with such a problem as varicocele for the first time, are primarily interested in whether it is possible to treat varicocele without surgery. Of course, it would be very tempting to do without surgery, or even better to cure varicocele with folk remedies. Unfortunately, I have to disappoint them. There are currently no effective methods for treating varicocele without surgery. A temporary positive effect can be provided by some herbal remedies that increase the tone of the veins (horse chestnut tincture, grape leaves), as well as medications (for example, Aescusan, Detralex, Phlebodia, etc.). Varicoceles, of course, will not go away with these medications, but the symptoms may decrease. To reduce the symptoms of varicocele, adherents of traditional medicine recommend limiting physical activity and wearing tight-fitting underwear (so that the scrotum does not sag, but is pressed against the perineum). Temporary relief can be expected from these measures, but the varicocele itself will not disappear. Therefore, I must state that attempts to cure varicocele without surgery only waste precious time.
Treatment of varicocele - operations
As I already mentioned, conservative methods of treating varicocele are ineffective.
Prevention
It is easier to prevent any disease than to treat it, so it is necessary to carry out preventive measures.
Measures aimed at reducing the risk of developing pathological dilation of veins in the scrotum:
- healthy eating has a beneficial effect on the intestines;
- taking vitamins;
- use contraception during sexual intercourse;
- reasonable physical activity;
- Regular visits to the doctor from adolescence.
Reasonable adherence to preventive measures not only minimizes the risk of developing the disease and its relapse, but also contributes to the choice of an effective and less invasive treatment method.
Advantages of Marmara microsurgery:
- A small cosmetic incision in the groin area, in the hair growth area (the scar is almost invisible)
- The greatest efficiency of the operation is achieved through the use of operating binoculars and microsurgical instruments
- Lowest percentage of relapses and complications (less than 5 percent)
- Can be performed on an outpatient basis, without hospitalization
- Short and easy postoperative and recovery period
I am aware of my responsibility for preserving the main thing that my patient trusts me, and I will do everything to justify the trust!
Diagnostics
To effectively treat the disease, you need to use all diagnostic methods. To detect varicocele, experienced specialists only need to visually examine the patient and palpate the plexus of testicular venous vessels in the form of a cluster. The man is examined in a standing position, in a calm state. To clarify the results of palpation, the patient is asked to tense the abdominal muscles (Valsalva maneuver) to improve the filling of testicular vessels with blood. In this case, the study of the enlarged area will be more complete. This will help in diagnosing grade 2-3 varicocele; if the problem is not expressed, you will need the help of modern equipment. Ultrasound and doplegraphic examination of the scrotum is necessary to clarify the diagnosis. The patient must be examined in two positions - standing and sitting. To rule out infertility, a man needs to have a spermogram. One semen examination is not enough; examination in the interval from 4 to 12 weeks will make the diagnosis more accurate. This diagnosis is very informative; it can be used to determine the type of varicocele, obtain data on the size of the testicle, the location of diseased veins, and thickening of the spermatic cord.
Questions about the article
Arthur
October 5, 2021 at 12:49 pm
Hello! Please tell me, is it necessary to undergo surgery for grade 1 varicocele? Or is it just observation? One urologist doctor says do it, and the other two say just observe, healthy lifestyle, medications, that supposedly even at the second stage they don’t perform surgery, they just look at the situation. That's not the task. Please advise as a doctor. Is it still necessary to have this operation? Doctors have so many opinions that it’s unclear what to do. 29 years old, male.
Anton Evgenievich Rotov
October 5, 2021 at 04:26 pm
Indications for surgery for varicocele are pain in the left testicle or pathological changes in the spermogram (impaired fertility). If you do not have these signs, then there is no need to rush into surgery.
Novel
September 21, 2021 at 07:36
Hello, I had a varicocele operation using a puncture in the thigh. Now it’s pulling a little in the scrotum area and where the stomach is on the left. 4 days have passed since the operation, is this normal? And what things I can’t do, please tell me
Anton Evgenievich Rotov
September 21, 2021 at 09:36
The method is called testicular vein embolization. At first, there may be a pulling sensation in the testicle, as with other methods of treating varicocele. Limitations: Avoid heavy lifting and strenuous physical activity.
Elena
September 3, 2021 at 08:53
A 17-year-old child was diagnosed with grade 3 varicocele. How necessary is surgery at this age? They offer laproscopy...
Anton Evgenievich Rotov
September 3, 2021 at 08:58
It's a must do. The way they use it in your hospital. There is no other way to cure varicocele
Dmitriy
August 17, 2021 at 22:00
We carried out embolization due to varicocele, after 2 weeks we did an ultrasound, there is no reverse blood flow, but the veins are dilated at rest by 3 mm and with a tension of 5 mm, can the operation be considered successful and start playing sports, at least running
Anton Evgenievich Rotov
August 19, 2021 at 09:28 pm
2 weeks is too short a period to evaluate the result of the operation. The fact that there is no retrograde blood flow is a good indicator. The veins may collapse later. As for running, there are no objections. I would wait with the load (weight lifting) for at least a month
Vladislav
May 21, 2021 at 09:38 pm
Hello. In December 2021, I had varicocele embolization. After 1 and 3 months after two ultrasounds, which I did after the operation, there was no improvement (The conclusion indicated the dilatation of the veins was 0.39 mm). But after 7-8 months, positive dynamics appeared, the veins became smaller (0.35 mm). After another 5 months, I did an ultrasound in another place where the result confirmed that there was improvement (0.3 mm). The current recommendation was to take Detralex for 3 months. I would like to clarify whether these changes are the result of embolization? and if so, is there any hope that after some time the varicocele will be able to go away? Or is there still a relapse? My concern is that after embolization they promise improvement in 1.5 months, but in my case more than a year has already passed and there is a varicocele, but positive dynamics are observed over a long period, in connection with this there is a misunderstanding!) Thanks in advance!
Anton Evgenievich Rotov
May 22, 2021 at 08:06
The effect of surgery for varicocele (including embolization) develops within 3 months. In your case, there is probably an incomplete effect (persistent varicocele)
Statistics
According to WHO (World Health Organization), varicocele occurs among men in 15-17% of cases. At the same time, a wide range of frequency of occurrence is revealed depending on the region and age of the subjects. However, when examined using ultrasound methods, varicocele is found in 35% of men of reproductive age.
During conscription, varicocele is detected in 5-7% of young people, and the highest incidence occurs at the age of 14-15 years - 19.3%. As a rule, varicocele occurs only on one side - on the left (80–98%). This is explained by the different drainage of the testicular veins on the right and left.
Bilateral varicocele occurs in 2-12% of cases, while right-sided varicocele occurs in only 3-8% of cases.
Traditional methods
Many people ask the question of how to cure varicocele at home, so the following set of measures has already become traditional:
- tinctures and decoctions for oral use;
- compresses for external use;
- medicinal baths;
- massage;
- aromatherapy;
- physiotherapy.
You can choose 3-4 suitable methods. The main thing is that there is a regular and comprehensive impact on the problem.
Herbs that help get rid of varicocele:
- horse chestnut;
- yarrow;
- Oak bark;
- St. John's wort;
- calendula.
These plants have analgesic, venotonic and anticoagulant effects.
It is also worth remembering herbs that are strictly contraindicated for varicocele:
- valerian;
- motherwort;
- hawthorn.
Home treatment can be carried out for unilateral varicocele. The bilateral process is usually abrupt and complicated. In this case, urgent surgery is required.
Tinctures and decoctions
Infusions, tinctures and decoctions are widely used as folk remedies for testicular varicocele. The most popular of them.
Chestnut flower tincture
Pour 100 grams of chestnut flowers into a bottle of vodka. Infuse for two weeks in a cool place. Take ten drops three times a day. Contraindication: kidney disease.
Oak bark decoction
Pour 100 grams of dry oak bark extract into a liter of water and boil. After this, simmer in a water bath. Then strain the mixture and take it, diluting 50 ml of decoction in 200 ml of water. Use in courses of one month. This is one of the most effective remedies for the treatment of varicocele.
Infusion of a mixture of herbs for varicocele
Pour 1 teaspoon of yarrow, chamomile flowers, chestnut, string, raspberry leaves, dried wort, St. John's wort into a liter of boiling water. Infuse for one day. Take 150 g twice a day for three weeks in a row.
Compresses and lotions
Applying compresses for testicular varicocele is a more complicated procedure than taking a decoction, but the effect is worth the effort.
Compresses and lotions help:
- relieve pain
- improve blood circulation;
- reduce swelling.
It is important to do the compress correctly - apply gauze soaked in the medicine, then a plastic bag or cling film. Cotton wool is placed on top and everything is bandaged with a bandage.
Common and effective compress recipes for the treatment of varicocele.
Oatmeal compress
Mix one tablespoon each of strawberry leaves, birch leaves, dandelion roots, sweet clover, and chopped oat straw. Take a tablespoon of the resulting mixture and pour 600 ml of boiling water. Leave for half an hour. The compress is made daily before bedtime according to the above scheme for three weeks.
Alcohol compress on acacia flowers
5 tbsp. l. acacia flowers pour 100 ml of vodka. Leave for 2 weeks in a cool, dark place. The recommended frequency of use of this compress is 3 times a week. Apply a compress before going to bed.
Oil lotion with St. John's wort
Pour one tablespoon of St. John's wort into 100 ml of vegetable oil. Simmer in a water bath for three hours. Make lotions with the resulting mixture four times a day. The product gives good results in a relatively short period of time.
Therapeutic baths
Hot baths for vein pathology are contraindicated. Therefore, we will talk about sitz baths only for the genitals. A deep basin is suitable for these purposes.
You can consider the following herbal bath recipes for varicocele.
- From a decoction of calendula. Pour boiling water (1 liter) over a handful of dry calendula and leave in a warm place for 2 hours. Strain and mix in a bowl of cold water. Take this bath for 15 minutes.
- From angelica. Pour 100 g of herb into a liter of boiling water. Leave for 14 hours. Pour into a bowl, dilute with cool water. The procedure time is 30 minutes.
- With oak leaves, wormwood, calendula and chamomile. Take the herbs in equal proportions, pour boiling water over them and let it brew. Then dilute with cold water. Bath duration is 20 minutes.
If you have varicocele, you should avoid saunas, steam baths and hot baths. The temperature of the therapeutic baths is not higher than 40°C.
Effect on male infertility
Reproductive dysfunction occurs due to the development of varicocele. Due to impaired blood supply, the following problems occur:
- The temperature of the testicles increases. Hyperthermia has a detrimental effect on the activity and viability of sperm;
- Hypoplasia, atrophy, testicular hypoxia. Tissues die, the function of producing sex hormones and cells decreases;
- Oxidation. The body's waste products (free radicals) accumulate in the testicles, poisoning them;
- Biological substances produced by the adrenal glands are released into the testicles.
Scientists have proven that due to these consequences, varicocele can provoke the development of male infertility. However, this does not mean that reproductive function is necessarily impaired in pathology. In some cases, high-quality spermogenesis remains, but in order to prevent the condition from worsening, it is important to consult a doctor.
Stages of development
The most important classification of the disease according to stages of development:
- First . There are no symptoms of pathology, the expansion is not visually visible or palpable. The problem can only be determined by ultrasound.
- Second . The disease cannot be visualized. When palpated in a vertical position, the expansion is palpable, especially after exercise. When lying down, the varicocele does not appear.
- Third . The patient independently feels the dilated venous nodes in any position: lying or standing.
- Fourth . The expansion is strong, noticeable to the naked eye. The nodes do not “hide” due to changes in body position, sometimes they even hang down, increasing the size of the scrotum by 1.5-2 times.
Some doctors combine the third and fourth stages.