Types of toxic changes in neutrophils
To characterize the severity of toxic changes in neutrophils, a certain classification is used. For this, doctors have developed a system of so-called pluses. The lesion classification system evaluates the size of granules formed in diseased cells, as well as the number of diseased cells in relative percentages:
- Toxic granularity "plus" - fine, that is, "dust-like" granularity is detected.
- The diagnosis “two pluses” is stated if the granularity is of medium size, and the number of pathological cells is about half.
- Granularity +++ – large modified grains in the cells. Cells are affected by 75%.
- If the analysis shows ++++, this means that there is a severe, threatening disease of blood cells, while they contain large granules and the cytoplasm is sparse.
In addition, the following types of changes are distinguished:
- Actually graininess.
- Dele structures that have variable sizes and shapes and are colored in a light blue hue.
- Vacuolization is the formation of vacuoles in the plasma of cells. This happens with dangerous diseases (sepsis) or with leukocytosis. It can be combined with elements of Dele and other pathologies.
- Hypersegmentation is the appearance of more than five segments in the cell nucleus. This happens with megaloblastic anemia. It can rarely be observed in healthy people (a special hereditary feature).
What is toxic neutrophil granulation?
This is a series of changes in neutrophils that are not always associated with the process of toxicosis in humans. Toxigenic neutrophil granulation is so called because it was first discovered in patients with sepsis caused by gram-negative microorganisms. However, this does not mean that such organisms produce a toxic effect on these blood elements.
Speaking about this condition, we usually mean a special violation of the morphological structure of these cells under conditions of stimulation of their formation in the bone marrow and acceleration of maturation. It reflects the asynchronous processes of maturation of the nucleus and cytoplasm of blood cells.
This pathology of leukocytes is manifested by the appearance of large granules and specific inclusions in the cytoplasm. This happens because the proteins of such a part of the cell change their structure . The formation of specific Dele bodies and cytoplasmic vacuoles is possible.
Types of toxic granularity of neutrophil granulocytes
To determine the severity of morphological changes in leukocyte granulocytes, a special classification is used - the plus system. It allows you to assess the nature of degenerative changes, the number of pathological cells as a percentage of the total volume of leukocyte granulocytes. Types of pathological granularity of neutrophil granulocytes:
- Toxic granulation + is characterized by the presence of fine “dust-like” granulation.
- Two pluses mean that granulation has average values, and the number of diseased neutrophils in the blood is more than half.
- Toxic granularity with three pluses is characterized by large, modified granules. About 80% of neutrophils in the disorder have degenerative morphological changes.
- With four pluses, almost all cells are deformed. Often this disorder ends in death, and therefore requires urgent intervention from specialists.
In addition to the above changes in the blood product, five main features of toxic changes in neutrophil granulocytes are observed:
- Cytoplasmic basophilia.
- Cytoplasmic vacuolation.
- Presence of Dele bodies.
- Immaturity of nuclei in cells.
- Toxic granulation.
Toxigenic granularity
Toxogenic granularity of neutrophils differs from toxic granularity in that granularity develops in conjunction with other, more serious abnormalities. These include basophilia, Knyazkov-Dele bodies, structures, light blue colored areas. Toxogenic granularity cannot be ignored even in small volumes (unlike toxic), as it is a serious symptom of truly severe processes associated with infections and viruses. Leukocytosis, which develops against the background of toxogenicity, can ultimately even lead to death.
Diagnostics
Toxic granularity cannot always be detected with conventional staining, so special methods are used to identify it, namely the Freifeld staining method. In this case, fuchsin and a solution of methylene blue are used.
To prepare the first dye, one gram of fuchsin is placed in 96% ethyl alcohol (15 grams) and heated until dissolved. After it has cooled, add a 5% solution of carbolic acid in an amount of 100 ml. Seven drops of the first dye are added to 20 ml of water and mixed, then the second dye (1% methylene blue solution) is added in an amount of five drops and mixed again. Blood smears are painted with the prepared mixture for an hour, after which they are washed off with water and dried. If Romanovsky staining was previously performed, the Freifeld method can be used without prior bleaching.
After staining, lilac granularity can be observed in the form of dust or flakes, which depends on the severity of the disease. As a result of the analysis, the size of the granules is usually indicated, that is, the granularity can be dusty, fine, medium, large, in the form of flakes, and the number of neutrophils (per hundred cells) with toxogenic granularity as a percentage.
- If immature granulocytes are elevated, what does this mean?
Large toxic granularity of neutrophils
In addition, when diagnosing you need:
- calculate the leukocyte formula;
- identify the total number of leukocytes;
- determine whether leukocytes have pathological changes;
- determine the level of young forms of neutrophils.
Leukocyte formula (with mandatory microscopy of a blood smear)
Leukocyte formula (with mandatory microscopy of a blood smear) - counting the total number and different types of leukocytes, as well as studying their morphological features through microscopy of a peripheral blood smear.
Synonyms Russian
Leukoformula.
English synonyms
Leukocyte Differential Count, WBC Count Differential, Diff, Blood Differential, Differential Blood Count, White Blood Cell Differential.
Research method
Flow cytometry.
What biomaterial can be used for research?
Venous, capillary blood.
How to properly prepare for research?
- Eliminate alcohol from your diet for 24 hours before the test.
- Children under 1 year of age should not eat for 30-40 minutes before the test.
- Do not eat for 2-3 hours before the test; you can drink clean still water.
- Avoid physical and emotional stress for 30 minutes before the test.
- Do not smoke for 30 minutes before the test.
General information about the study
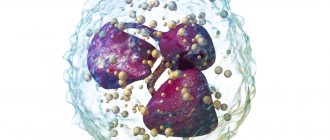
Leukocytes are a heterogeneous population of nucleated blood cells that are an essential part of the human immune system and play a role in inflammation, allergies and antitumor defense. There are five types of leukocytes, each of which performs its own specific functions: three types of granulocytes (eosinophils, basophils, neutrophils), monocytes and lymphocytes. The study of the leukocyte formula in a peripheral blood smear is a count of the number of different types of leukocytes and an assessment of their morphological properties. Both venous and capillary blood can be used for research.
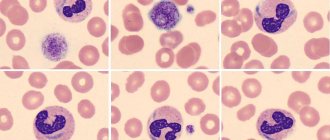
Staining a blood smear with special dyes makes it possible to distinguish cells and intracellular structures; in addition, different types of leukocytes are not equally susceptible to certain dyes and are stained differently, which, together with differences in their morphological properties (shape of the nucleus, size and presence of intracellular granules), makes it possible to differentiate the main types of leukocytes when examining a smear using a microscope. Traditionally, the count is carried out per hundred cells and the resulting numbers are recorded as percentages. Knowing the total number of leukocytes, percentages can be converted into absolute values, which much more objectively reflect the state of the leukocyte population.
Granulocytes are so called because they contain granules in their cytoplasm, which contain biologically active substances necessary for leukocytes to perform their protective functions. There are three types of granulocytes:
- Mature neutrophils have a nucleus and granules segmented into 4-5 lobules, which turn purple when stained according to Romanovsky-Giemsa. Segmented neutrophils make up the bulk of peripheral blood leukocytes. In much smaller quantities in the blood, neutrophils of the previous stage of maturation can be found - band neutrophils (with a nucleus not yet divided into lobules). Cells of earlier stages of maturation (metamyelocytes, myelocytes and others) can appear in a blood smear in exceptional cases - for example, in severe infectious diseases, when the bone marrow throws out not yet mature cells to fight the infection (this is called a shift of the leukocyte formula to the left), and also in chronic myeloid leukemia.
- Eosinophils are involved in antiparasitic immunity and the development of allergic reactions. Their granules, which are orange-pink in color, contain mediators of allergy and inflammation. Eosinophils also differ from neutrophils in the structure of their nucleus - it is bilobed.
- Basophils are granulocytes that take an active part in immediate allergic reactions. They have an S-shaped non-segmented nucleus, which is often not visible due to large granules of intense blue color containing allergy mediators.
- Lymphocytes are cells with a large nucleus, practically devoid of cytoplasm. When stained according to Romanovsky-Giemsa, their nucleus is stained in an intense purple-violet color, and the cytoplasm is blue-blue. Lymphocytes participate in more complex immune reactions associated with the recognition of their own and foreign antigens and the production of antibodies. There are three classes of lymphocytes: T lymphocytes, B lymphocytes and NK cells (natural killer cells), but standard staining does not allow them to be distinguished; more technically complex methods are used for this (for example, immunophenotyping).
- Monocytes are relatively large leukocytes containing an unsegmented bean-shaped nucleus and, unlike lymphocytes, a large amount of cytoplasm. When stained according to Romanovsky-Giemsa, the nucleus acquires a purple-red color, and the cytoplasm becomes a cloudy bluish-gray. The main function of monocytes is phagocytosis, that is, the absorption and digestion of microorganisms, their own dying cells, etc.
The above types of leukocytes are found normally in a peripheral blood smear. In some diseases, cells that normally should not be in the smear may enter the blood from the bone marrow: for example, blasts are the morphological substrate of acute leukemia. In the conclusion to the study, the number and, if possible, morphological features of atypical cells must be indicated.
In addition to counting the number of cells, a laboratory diagnostic doctor, using microscopy of a blood smear, notes changes in the morphology of leukocytes:
- Toxogenic granularity of neutrophils - dark large coarse granules are present inside the cells, which are formed as a result of coagulation (“welding”) of the cytoplasmic protein under the influence of intoxication products.
- Vacuolization of the cytoplasm is also caused by severe intoxication, under the influence of which fatty degeneration occurs in the cell, and when the smear is fixed with alcohol, droplets of fat dissolve and the cells acquire a characteristic appearance.
- Knyazkova-Dele bodies are large pale blue areas of the cytoplasm of neutrophils, free from specific granules. Also found in inflammatory diseases, sepsis.
- Hypersegmentation of neutrophil nuclei - more than five segments in the nucleus of a segmented neutrophil. It may be a congenital feature (in which case it has no clinical significance), but a consequence of a deficiency of vitamin B12 or folic acid.
- Pelger's leukocyte anomaly is a congenital disorder of neutrophil maturation, manifested by a decrease in the segmentation of their nuclei. Mature neutrophils contain an unsegmented or two-segmented nucleus. This is not accompanied by a violation of the physiological properties of neutrophils.
- Botkin-Gumprecht shadows are dilapidated nuclei of leukocytes with remnants of nucleoli, obtained in the process of preparing a smear from tumor cells in chronic lymphocytic leukemia.
What is the research used for?
- To determine the number of individual types of leukocytes and their relationship with each other, assessing the morphological characteristics of leukocytes.
When is the study scheduled?
- If an infectious disease is suspected, as well as a pathology of bone marrow hematopoiesis.
- If the number of leukocytes deviates from the reference limits according to a blood test performed on a hematology analyzer.
What do the results mean?
Reference values
Leukocytes
| Age | Reference values |
| Less than 1 year | 6 - 17.5 *10^9/l |
| 1-2 years | 6 - 17 *10^9/l |
| 2-4 years | 5.5 - 15.5 *10^9/l |
| 4-6 years | 5 - 14.5 *10^9/l |
| 6-10 years | 4.5 - 13.5 *10^9/l |
| 10-16 years | 4.5 - 13 *10^9/l |
| More than 16 years | 4 - 10 *10^9/l |
Neutrophils
| Age | Reference values |
| Less than 1 year | 1.5 - 8.5 *10^9/l |
| 1-2 years | 1.5 - 8.5 *10^9/l |
| 2-4 years | 1.5 - 8.5 *10^9/l |
| 4-6 years | 1.5 - 8 *10^9/l |
| 6-8 years | 1.5 - 8 *10^9/l |
| 8-10 years | 1.8 - 8 *10^9/l |
| 10-16 years | 1.8 - 8 *10^9/l |
| More than 16 years | 1.8 - 7.7 *10^9/l |
Lymphocytes
| Age | Reference values |
| Up to 1 year | 2 - 11 *10^9/l |
| 1-2 years | 3 - 9.5 *10^9/l |
| 2-4 years | 2 - 8 *10^9/l |
| 4-6 years | 1.5 - 7 *10^9/l |
| 6-8 years | 1.5 - 6.8 *10^9/l |
| 8-10 years | 1.5 - 6.5 *10^9/l |
| 10-16 years | 1.2 - 5.2 *10^9/l |
| More than 16 years | 1 - 4.8 *10^9/l |
Monocytes
| Age | Reference values |
| Up to 1 year | 0.05 - 1.1 *10^9/l |
| 1-2 years | 0.05 - 0.6 *10^9/l |
| 2-4 years | 0.05 - 0.5 *10^9/l |
| 4-16 years | 0.05 - 0.4 *10^9/l |
| More than 16 years | 0.05 - 0.82 *10^9/l |
Eosinophils
| Age | Reference values |
| Up to 1 year | 0.05 - 4 *10^9/l |
| 1-6 years | 0.02 - 0.3 *10^9/l |
| 2-4 years | 0.02 - 0.5 *10^9/l |
Basophils: 0 - 0.8 *10^9/l.
Blood smear microscopy
Neutrophils - rods: 0 - 5%.
Neutrophils - segment.
| Age | Reference values |
| Up to 1 year | 16 — 45 % |
| 1-2 years | 28 — 48 % |
| 2-5 years | 32 — 55 % |
| 5-7 years | 38 — 58 % |
| 7-8 years | 41 — 60 % |
| 8-12 years | 43 — 60 % |
| 12-16 years old | 45 — 60 % |
| More than 16 years | 47 — 72 % |
Lymphocytes, %
| Age | Reference values |
| Up to 1 year | 45 — 75 % |
| 1-2 years | 37 — 60 % |
| 2-4 years | 33 — 55 % |
| 4-6 years | 33 — 50 % |
| 6-8 years | 30 — 50 % |
| 8-10 years | 30 — 46 % |
| 10-16 years | 40 — 45 % |
| More than 16 years | 19 — 37 % |
Monocytes, %
| Age | Reference values |
| Up to 1 year | 4 — 10 % |
| 1-2 years | 3 — 10 % |
| More than 2 years | 3 — 12 % |
Eosinophils, %
| Age | Reference values |
| Up to 1 year | 1 — 6 % |
| 1-2 years | 1 — 7 % |
| 2-4 years | 1 — 6 % |
| More than 4 years | 1 — 5 % |
Basophils,%: 0 - 1%.
An increased level of neutrophils can be observed during acute bacterial infections, intoxications and myeloproliferative diseases.
Neutropenia can be caused by severe infection, sepsis, toxic effects on the bone marrow (cytostatics, ionizing radiation, myelotoxic drugs), aplastic anemia, as well as congenital diseases (Kostmann's neutropenia, cyclic neutropenia).
The most common causes of eosinophilia are allergic diseases, parasitic infections, and myeloproliferative diseases.
An increase in basophils may indicate allergic reactions or myeloproliferative diseases.
Absolute lymphocytosis occurs in viral infections, including infectious mononucleosis and cytomegalovirus infection, chronic lymphocytic leukemia.
to a decrease in the number of lymphocytes .
Monocytosis is possible with infections, granulomatous diseases (tuberculosis, brucellosis, sarcoidosis), blood tumors, systemic connective tissue diseases.
Important Notes
- An increase or decrease in the percentage of any type of leukocyte is called relative and does not always correspond to a change in the absolute value.
Also recommended
- Clinical blood test: general analysis, leukocyte count, ESR (with mandatory blood smear microscopy)
Who orders the study?
Hematologist, therapist, pediatrician, general practitioner, infectious disease specialist, oncologist.
Literature
- Henry's Clinical Diagnosis and Management by Laboratory Methods, 23e by Richard A. McPherson MD MSc (Author), Matthew R. Pincus MD PhD (Author). St. Louis, Missouri: Elsevier, 2021. Pages 527-531.
- A Manual of Laboratory and Diagnostic Tests, 9th Edition, by Frances Fischbach, Marshall B. Dunning III. Wolters Kluwer Health, 2015. Pages 67-82.
- Guide to laboratory diagnostic methods / Kishkun A. A. Moscow: GEOTAR-Med, 2007. P. 44-60.
Formation of degenerative changes
Toxic granularity of neutrophils, what does it mean and what is the reason. Normally, a neutrophil cell in the blood contains tiny inclusions - grains. In the presence of a strong inflammatory process, accompanied by the release of purulent exudate, changes occur in tissue cells. Under the influence of an infectious agent, physicochemical reactions occur, leading to the coagulation of protein in the blood and its attachment to the natural grains of the cell.
Thus, on the one hand, the caliber of deformed granularity and quantity increases, on the other hand, the cytoplasm becomes rarefied, i.e. the cytoplasm of the neutrophil cell loses its saturation due to protein coagulation.
Degenerative changes often appear before the nuclear shift and can serve as a warning against deterioration of the condition and the threat of developing negative consequences.
Prognostic significance
Toxic granularity of neutrophils is the body’s response to a pathological process, and determining its presence is important because such a degenerative change in cells quite often appears earlier than the leukocyte nuclear shift.
In most cases, toxogenic grain is:
- The precursor of neutrophilia is an increase in the absolute or relative quantitative content of neutrophils;
- Shift of the leukocyte formula to the left;
- The appearance in the blood of a large number of immature or band neutrophils, as well as young cellular forms - metamyelocytes and myelocytes.
In addition, an increase in the % level of degradation of neutrophil granules indicates the development of bacteremia and generalization of infection.
If the number of neutrophils with such toxogenic granularity in purulent-septic diseases, lobar pneumonia and some other inflammatory diseases exceeds 50%, and upon repeated analysis their percentage also increases, then this indicates a severe course of the infectious pathology and is a poor prognostic clinical symptom.
Toxogenic granularity of neutrophils is an important clinical symptom during the diagnosis of the following diseases:
- acute abdominal syndrome, in particular gangrenous appendicitis;
- the child has Chediak-Higashi disease.
By assessing the dynamics of toxic granules, the doctor also judges the effectiveness of the prescribed treatment, and, if necessary, decides to correct the chosen drug therapy regimen.