Renin is a specific enzyme that is produced in the kidneys. Its functions include monitoring fluid balance and sodium levels. Violations of this balance lead to a sharp increase in blood pressure. Therefore, if hypertension occurs, the patient is prescribed a blood test for renin.
Despite the fact that this enzyme compound is produced by a parenchymal organ, it cannot be considered a true hormone. This is due to the area of influence of this enzyme. It contains only one type of protein. Thanks to this diagnostic test, many serious diseases can be identified.
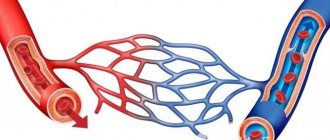
Renin levels depend on blood pressure. The mechanism of influence of this enzyme is complex. Immediately after production, renin enters the blood, resulting in the transition of angiotensinogen to angiotensin I. The latter is then converted into the same substance of the second type. At the same time, the following processes occur: narrowing of blood vessels and activation of the process of aldosterone production. At the last stage, the balance of potassium and sodium is stabilized and blood pressure is normalized.
Aldosterone and renin are related to each other, so doctors often order specific tests to determine their levels at the same time. Data on the obtained ratio are necessary to identify the exact cause of the patient’s ailment.
Active renin results from the synthesis of prorenin. This element is formed in juxtaglomerular cells. The diagnostic scheme must include OAM, liver and kidney tests, ionogram, and biochemical blood test.
general characteristics
Renin is a proteolytic enzyme, one of the components of the body's renin-angiotensin system. Under the influence of renin, angiotensinogen is converted into angiotensin-I, which, under the action of angiotensin-converting enzyme, becomes angiotensin-II (a powerful vasoconstrictor), the latter promotes the synthesis and release of aldosterone (a hormone that regulates the exchange of sodium and potassium). The most important factor enhancing renin formation is a decrease in renal blood flow. The content of renin in the blood has a daily rhythm and depends on the volume of blood volume, sodium level and body position (vertical or horizontal). In practice, it is preferable to determine the direct renin concentration. The advantage of direct determination of renin is that it does not depend on the level of renin substrates in plasma, as in determining activity (maximum plasma renin activity is measured only at the saturating plasma concentration of angiotensinogen). Also see Aldosterone-Renin ratio.
Indications for use
An analysis of renin levels in the blood is necessary to determine pathologies accompanied by disruptions in the production of this hormone. Significant reasons for prescribing a laboratory test are:
- potassium deficiency;
- lack of a positive effect when using the usual treatment regimen;
- presence of hypertension in the patient's medical history;
- partial dysfunction of the kidneys and (or) adrenal glands;
- malignant neoplasm in the area of parenchymal organs;
- narrowing of the renal artery.
Patient preparation rules
Standard conditions, unless otherwise determined by the doctor. 2 weeks in advance, agree with your doctor on the intake of: drugs from licorice root, diuretics, antihypertensive drugs, oral contraceptives. For 3 days - food without salt restriction. 8 hours in advance - fast, eliminate fatty foods. You can drink water. 2 hours before - be in an upright position (standing, sitting). In 5 minutes, sit at the manipulation table. If directed by a doctor, blood may be taken after the patient has been in a horizontal position for 1-2 hours.
You can add this study to your cart on this page
Collection process
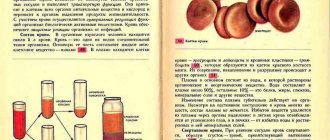
The level of renin depends on the state of the central nervous system and the drinking regime. A patient referred for this procedure should limit salt intake. The biological material required for the renin test is taken from the renal or peripheral vein. An X-ray machine may be required during collection. The collected blood is first placed in a tube with EDTA, after which laboratory assistants separate the plasma and freeze the biomaterial (temperature is -20 degrees Celsius).
A negative result does not guarantee the absence of pathology. Therefore, the doctor prescribes additional tests. The need for this is due to the fact that the exact cause of the ailment cannot be determined based on only one diagnostic test. The general scheme includes comprehensive studies, ultrasound, MRI, computed tomography and stress tests.
Diagnosis of primary type hyperaldosteronism is carried out by determining the ratio between aldosterone and renin in a direct way. The required indicator is detected by chemiluminescence immunoassay. It is based on the immunological reaction of blood plasma, the occurrence of which is achieved through the use of phosphors. This is the name given to components that produce light when exposed to ultraviolet light. The result is determined by the level of luminescence.
Interpretation:
- Increased with subsequent secondary aldosteronism: 1. Hypertensive conditions: malignant or severe hypertension, unilateral kidney damage with severe or malignant hypertension, parenchymal renal lesions, renin-secreting tumors, hypertension caused by oral contraceptives, pheochromocytoma.2. Edema normotensive conditions: liver cirrhosis, hepatitis, nephrosis, congestive heart failure.3. Hypokalemic normotensive conditions: juxtaglomerular cell hyperplasia (Barter's syndrome), other nephropathies with loss of sodium or potassium, nutritional disorders with loss of electrolytes. Increase without subsequent secondary aldosteronism: adrenocortical insufficiency, decreased potassium content in the body.
- Decreased without diseases of the adrenal cortex: hypertensive states, essential hypertension with low renin activity; Liddle syndrome-pseudohyperaldosteronism; normotensive conditions - parenchymal kidney diseases, autonomic disorders with hypotension.
Sample result (PDF)
Publications in the media
Regarding the treatment of this disease, you can contact the Surgical Department No. 2 of the Clinic of Faculty Surgery named after. N.N. Burdenko
Hyperaldosteronism (aldosteronism) is a condition resulting from hypersecretion of aldosterone or a violation of its metabolism. Frequency. 0.5–2% of all cases of arterial hypertension. The predominant age is over 40 years. The predominant gender is female. There are primary and secondary hyperaldosteronism • Primary is a clinical syndrome that occurs with lesions of the adrenal glands and is manifested by arterial hypertension, hypokalemia and low renin levels in the blood serum • Secondary (symptomatic) is caused by causes localized outside the adrenal glands. Renin content is significantly increased.
Etiology • Primary hyperaldosteronism •• Unilateral aldosterone-secreting adenoma (Conn's syndrome) is the most common cause (60%) •• Bilateral zona glomerular hyperplasia of the adrenal cortex (idiopathic aldosteronism) is the second most common cause (34%) •• Bilateral aldosterone-secreting adenoma •• Unilateral aldosterone-secreting carcinoma of the adrenal cortex • Secondary hyperaldosteronism •• Renal artery stenosis •• Malignant hypertension •• Renin-secreting tumors •• Ectopic foci of ACTH secretion •• Bartter's syndrome •• Taking oral contraceptives •• Various conditions accompanied edema (heart failure, liver cirrhosis, nephrotic syndrome), cause ischemia of the cells of the juxtaglomerular apparatus of the kidneys, which leads to the release of renin, which increases the content of angiotensins and aldosterone.
Pathogenesis. Aldosterone increases sodium reabsorption and excretion of potassium and hydrogen ions in the distal renal tubules • Sodium retention causes an increase in blood pressure • Potassium loss leads to muscle weakness, paresthesia, tetany •• Hypokalemia reduces insulin secretion by the pancreas, which reduces carbohydrate tolerance •• Hypokalemia reduces sensitivity of renal tubular receptors to ADH, which leads to polyuria.
Clinical picture • Mild to severe arterial hypertension with a predominant increase in diastolic blood pressure is the dominant sign of the disease • Severe hypokalemia in most cases is accompanied by muscle hypotonicity and cramps, headaches, tachycardia, polydipsia, polyuria and nocturia • Edema is not typical.
Laboratory tests • Hypokalemia in combination with increased excretion of potassium in the urine • Hypernatremia • Hypochloremia (hypochloremic alkalosis) • High concentration of aldosterone in the blood serum and urine, not corrected by drugs. Aldosterone content is determined under standard conditions, because it is influenced by sodium balance, use of diuretics and other factors •• Diuretics and vasodilators are stopped 2 weeks before determination of aldosterone and renin levels •• Sodium loading is carried out to differentiate primary aldosteronism (no suppression with sodium load) from increased aldosterone levels in healthy individuals (suppression with sodium load) • Low renin activity in the blood plasma with primary aldosteronism; in secondary – high • Influence of drugs. Diuretics, estrogens, ACE inhibitors, vasodilators, calcium channel blockers and adrenergic blockers can alter renin secretion • Effect of diseases. Malignant arterial hypertension can lead to hyperreninemia, secondary hyperaldosteronism and hypokalemia.
Special studies • Postural test: record the dynamics of aldosterone secretion caused by a 4-hour stay in an upright position (aldosterone concentration is determined at 8 am and at 12 noon in the afternoon) •• In healthy people and patients with bilateral hyperplasia, the concentrations of renin and angiotensin increase with subsequent increased aldosterone levels •• In patients with unilateral adrenal adenomas, a decrease in aldosterone levels is noted • Trial treatment with spironolactone • CT and MRI can detect adrenal adenomas in 80% of cases. Tomographic sections of the adrenal glands should be made every 3 mm • Angiography of the adrenal vessels • The concentration of aldosterone in blood samples from the adrenal veins obtained by selective catheterization allows us to differentiate the causes of aldosteronism. A unilateral increase in aldosterone levels indicates an adenoma; high concentrations on both sides are characteristic of bilateral hyperplasia.
Differential diagnosis • Diuretic use • Renovascular hypertension • Pheochromocytoma • Renin-secreting tumor • Malignant hypertension • Congenital adrenal hyperplasia • Aldosterone-secreting tumor • Use of GCs in high doses • Excessive consumption of mineralocorticoids or consumption of licorice (licorice root) • Pseudoaldosteronism (Liddle's syndrome).
TREATMENT
Management tactics • Sodium-restricted diet, regular dosed physical activity (set of exercises), optimization of body weight, smoking cessation • Conn's syndrome - unilateral adrenalectomy (correction of hypokalemia with spironolactone is required before surgery) • Idiopathic hyperaldosteronism - long-term drug therapy - potassium-sparing diuretics (spironolactone 25–50 mg 3 times / day) and other antihypertensive drugs (for example, calcium channel blockers, ACE inhibitors, small doses of thiazide diuretics).
Observation • Determination of blood pressure • Determination of serum potassium levels • Determination of urinary aldosterone concentrations within 24 hours after adrenalectomy • All patients with arterial hypertension and hypokalemia of unknown etiology should be examined for aldosteronism.
Drug therapy
Drugs of choice • Spironolactone 75–150 mg/day (to compensate for hypokalemia) • Antihypertensive drugs: calcium channel blockers, ACE inhibitors or thiazide diuretics in small doses • For Bartter's syndrome - potassium-rich foods, nutritional supplements in combination with spironolactone, triamterene, amiloride or propranolol usually reduce the clinical manifestations of the disease, but do not completely prevent potassium loss.
Complications. Cardiac arrhythmias (possibly fatal) associated with severe hypokalemia.
Course and prognosis. Surgical removal of an aldosterone-secreting adenoma leads to the disappearance of arterial hypertension in approximately 70% of cases. Arterial hypertension usually disappears gradually over 1–4 months.
ICD-10 • E26 Hyperaldosteronism
Note. Sodium loading, methods of implementation • Measure the level of aldosterone excretion in 24-hour urine after the patient has taken more than 150 mEq of sodium for at least 3 days (sodium chloride tablets are usually prescribed). Sodium loading may further reduce serum potassium levels, so use caution in case of hypokalemia. Elevated aldosterone levels in 24-hour urine containing more than 150 mEq of sodium indicate primary aldosteronism • Plasma aldosterone levels are measured after infusion of 2,000 ml of 0.9% sodium chloride solution over 4 hours. Normal values are below 8–10 ng%. Contraindications: severe arterial hypertension and congestive heart failure.
Pathogenesis
Aldosterone helps to increase the concentration of sodium in the blood plasma by increasing the reabsorption of this ion from primary urine and reducing the potassium content due to the acceleration of its secretion. As a result of sodium retention, the osmotic pressure of the blood increases and the volume of circulating fluid increases. High sodium content leads to sensitization of the vascular wall and the effects of endogenous pressor substances (catecholamines). The result of these pathophysiological changes is an increase in blood pressure.
An increase in the concentration of aldosterone in the blood causes damage to the myocardium, blood vessels and kidneys. In patients suffering from primary hyperaldosteronism for a long time, aldosterone-dependent myocardial hypertrophy is noted. Although left ventricular hypertrophy is considered a nonspecific manifestation of hypertension of any origin, it has been proven that an increase in myocardial mass in PHA develops earlier and is more pronounced.
With PHA, diastolic myocardial function is impaired to a greater extent than with hypertension of other etiologies. Diastolic overload causes left atrium dilatation. With a prolonged increase in aldosterone concentration, fibrotic changes develop in the myocardium. It has been established that after surgical treatment of aldosteroma and normalization of blood pressure, despite a decrease in myocardial hypertrophy, diastolic myocardial dysfunction may persist.
In patients with PHA, along with nonspecific changes observed in any hypertension (like arteriolosclerotic nephrosclerosis), a specific morphological manifestation of the disease is described - the so-called hypokalemic kidney. The morphological substrate of these changes is interstitial inflammation and sclerosis of the interstitium as a result of damage to the tubular epithelium during hypokalemia and metabolic alkalosis. A hypokalemic kidney can cause renoprival hypertension, that is, the formation of secondary hyperaldosteronism.
Treatment
Drug treatment
To reduce the risk of surgery and anesthesia, preoperative correction of hypertension and water-electrolyte imbalance is necessary. For this purpose, spironolactone, slow calcium channel blockers, and α1-blockers are used. In case of idiopathic aldosteronism or refusal of surgical treatment, the main drug for effective therapy is spironolactone. The remaining groups of antihypertensive drugs do not have any advantage over each other for the correction of arterial hypertension in hyperaldosteronism. It is not always possible to relieve hypertension and hypokalemia with idiopathic aldosteronism using drug therapy. Indications for unilateral adrenalectomy in such cases include resistance of hypertension to combination antihypertensive therapy, the presence of complications during treatment with high doses of drugs or contraindications to therapy (intolerance, allergies, etc.).
Clinical picture
Hypertension is one of the most persistent symptoms of PHA. Hypertension is manifested by headache, dizziness, the appearance of spots before the eyes, etc. The nature of hypertension varies from malignant, resistant to traditional antihypertensive therapy, to moderate and mild, amenable to correction with small doses of antihypertensive drugs (the higher the concentration of aldosterone in the blood, the higher the blood pressure values) . Hypertension can have either a crisis or persistent course. Disorders of neuromuscular conduction and excitability (muscle weakness, paresthesia, convulsions, bradycardia, rarely tetany) are mainly associated with hypokalemia. Due to electrolyte disturbances, the function of the renal tubules changes (thirst, polyuria, nocturia). At the same time, all of the indicated signs of PHA may not be present, and cases of oligosymptomatic or even asymptomatic progression are often observed. The absence of neuromuscular and renal disorders should not be considered as a criterion for excluding PHA.