Authors:
Currie KD, Floras JS, La Gerche A, Goodman JM.
Translation
- Sergei Strukov.
Current guidelines defining indicators for exercise testing and the prognostic importance of excessive blood pressure response to exercise lack contextual references and require updating.
- The magnitude and rate of change in blood pressure varies depending on age, gender, baseline values, training level, heart rate, comorbidities, and exercise protocol.
- The clinical utility of blood pressure measurement during exercise may increase with the establishment of normative ranges that integrate similar variables and defining models with better prediction of cardiovascular events.
Introduction
Blood pressure (BP) measurement during clinical exercise testing (CST) is a necessary adjunct to electrocardiography (ECG) and heart rate (HR) assessment, as abnormal responses may reveal underlying pathology. Given the difficulty of measuring BP during exercise, accurate measurement techniques are required to ensure optimal clinical interpretation (1). Widely accepted contraindications to continued CST for safety include upper blood pressure limits (2,3). However, definitions of “normal” BP during exercise and a safe “upper limit” are based on a limited number of studies dating back to the early 1970s (4, 5). Since then, our knowledge of phenotypic variations and possible links to pathology of abnormal BP responses has evolved significantly. Despite this, BP responses in CST that exceed the recommended norms often pose a dilemma due to unclear clinical consequences, especially when other tests are normal. There is compelling evidence that excessive increases in systolic blood pressure (SBP) or diastolic blood pressure (DBP) during CST, called the hypertensive response (2, 3), are associated with a 36% increased risk of cardiovascular events and mortality (6), masked hypertension, despite clinically normal blood pressure (7), and an increased risk of latent hypertension in normotensive people (8 – 18). These observations highlight the potential clinical diagnostic and prognostic utility of exercise BP measurements, but they are not yet widely used in clinical practice due to limitations of previous studies (19), lack of standardized methodology, and limited empirical data in the general population.
The purpose of this review is to critically analyze the evidence contained in current guidelines for CST AD. We will show that the criteria used to define “normal” and “abnormal” responses are largely arbitrary and based on insufficient empirical data. We will also identify key factors influencing BP responses during exercise and how to increase their explanatory value in individual responses to CST. Finally, we will provide recommendations for future studies on exercise BP measurement to expand the evidence base and facilitate its adoption into clinical practice.
Norms of pressure indicators in the load field
The maximum permissible pressure after physical activity is 140/90 mmHg. It should not rise higher to supply the muscles with blood. Within an hour after exercise, the pressure drops to normal levels; otherwise, other organs experience a lack of blood.
When measuring a person's blood pressure, it is necessary to take into account the conditions of physical education. Figures greater than the above are justified when:
- The workout started without warming up, the body is not prepared.
- Improper breathing during exercise.
- High air temperature.
- Diseases of the circulatory system.
Neglecting to warm up is a common mistake that can lead to surges in blood pressure and injuries to the muscular-ligamentous system.
“Normal” blood pressure reactions to CST
With increasing physical activity, SBP increases linearly, mainly due to an increase in cardiac output to satisfy the demand from working muscles. Sympathetically mediated vasoconstriction reduces splanchnic, hepatic and renal blood flow (this increases vascular resistance), the local vasodilatory effect suppresses vasoconstriction (“functional sympatholysis”), allows the redistribution of cardiac output to working skeletal muscles and reduces overall peripheral vascular resistance. These opposite reactions contribute to the maintenance or slight decrease in DBP during CST. A detailed discussion of the regulatory mechanisms of these reactions is beyond the scope of our review; they are widely discussed elsewhere (20). The American College of Sports Medicine (ACSM) and the American Heart Association (AHA) define a “normal” response as an increase in SBP of approximately 8 to 12 mmHg. Art. (2) or 10 mm Hg. Art. (3) per metabolic equivalent (MET – 3.5 ml/kg/min). The source of these values is a 1973 textbook study where healthy men (with unknown sample size and age) showed mean and peak SBP increases of 7.5 and 12 mmHg. st./MET, respectively. An abnormally elevated (“hypertensive”) response to exercise was defined as exceeding these values (12 mmHg/MET) (5). Thus, widespread and long-standing recommendations defining a “normal” response to CST are limited by data from a single study of men with a poorly characterized phenotype. Below we will present information about the significant impact of the blood pressure response to CST depending on gender, level of training, concomitant diseases and associated medications.
Influence of age and gender
In a study of 213 healthy men (4), changes in SBP in response to increasing exercise intensity increased with each decade of life. The largest increase in SBP per MET was observed in the oldest group (50–59 years; 8.3 ± 2.3 mmHg/MET), compared with an average increase of 5.7 ± 2.3 mmHg. Art./MET in the youngest group (20 – 29 years old). With age, the slope of the response graph increased (p <0.001) (Fig. 1a).
Data on the effect of gender on BP response during CST are limited. A group of healthy women aged 20–42 years responded with an average increase in SBP of 5.0±1.1 mmHg. st./MET (21). The slope of the graph should be less than that of men of the same age (Fig. 1b, p <0.001). It is noteworthy that the average increase in the groups of men and women was much lower than the “normal” response range of 8 – 12 mm Hg. st./MET. In contrast, current studies of the effects of age and sex suggest that in older women, the hypertensive response to exercise occurs due to a limited ability to reduce systemic vascular resistance (22). Unfortunately, there are no data on the BP response to exercise in older adults (>65 years), which limits our clinical interpretation of the BP response to CST.
Impact of health status and medications
The level of training during CST behaves as an independent factor influencing blood pressure. According to Fick's rule, maximum oxygen consumption (VO2max) depends on cardiac output and the arteriovenous oxygen difference. A higher VO2max value corresponds to a higher cardiac output, which means a greater increase in SBP. Therefore, when interpreting the maximum SBP obtained during CST, it is necessary to take into account the level of training (VO2max). The rate of change in SBP can also change with the level of training. In a study of young men, 16 weeks of endurance training increased VO2max and peak SBP (Fig. 2a) during CST (23). When we plotted the increase in SBP during CST versus VO2max, the slope of the curve after training was steeper (Fig. 2b; p=0.019). In women, differences in SBP during CST are also observed depending on training. With increasing training, SBP with CST is lower than that of sedentary peers. Young, exercised women achieve higher SBP at the end of the test compared to their sedentary counterparts (24).
Rice. 1. Response of systolic blood pressure (SBP) to a progressive exercise test in healthy people.
Values are presented as changes (Δ) in SBP compared to baseline values with increasing exercise intensity, expressed in metabolic equivalents (METs):
- a) data from healthy men, divided by decades of life;
- b) data from healthy men (20 – 39 years old) and women (20 – 42 years old).
The figure is based on previously published values (4, 21). Regression equations are presented for each gender.
* p < 0.001 for between-group differences in the slope of the SBP response curve.
Rice. 2. Systolic blood pressure (SBP) response before and after 16 weeks of endurance training in healthy men:
- a) the maximum SBP was obtained in a test with a gradual increase in load;
- b) the increase in SBP during the test is shown as a percentage of maximum oxygen uptake (VO2max).
The figure is based on previously published values (23). Before/after regression equations are shown.
* p < 0.05 for differences in the slope of the SBP response curve.
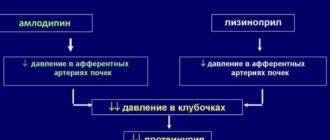
Comorbidities, especially those affecting BP and its regulation, or other indicators of cardiovascular disease also influence BP response to exercise. In people with normal and untreated hypertension (without known baroreflex sensitivity impairments), there is a similar increase in SBP and mean BP with increasing exercise intensity, but the higher baseline BP in people with hypertension results in greater values at maximal effort (25, 26). Conversely, people with hypertension and impaired arterial baroreflex sensitivity experience a greater absolute increase in BP during bicycle ergometry (27). Individuals with changes in autonomic nervous system function also differ in their BP response to exercise, as cervical spinal cord injuries (eg, tetraplegia) are typically associated with altered cardiovascular activity due to absent or reduced sympathetic tone below injury levels (28). Some studies have shown a decrease in SBP with exercise in people with tetraplegia, compared with healthy controls and people with paraplegia (partial or complete preserved sympathetic tone below the level of injury) (29, 30). Similarly, people with diabetes and autonomic neuropathy experienced less of a rise in SBP from baseline and reached lower peak values (37 ± 6 mmHg and 158 ± 7 mmHg, respectively) compared with people without autonomic neuropathy ( 55±8 mmHg and 176 mmHg) (31). In addition, in patients with coronary artery disease, dyslipidemia, and diabetes, aerobic exercise may increase DBP (32, 33). All of these responses are distinct from the pathological conditions associated with exercise hypotension (10 mmHg decrease in SBP with increased exercise) (2, 3), including coronary heart disease and left ventricular dysfunction (34 – 36). Medications prescribed in this clinical population also lower exercise BP: nitrates, calcium channel blockers, diuretics, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and β-blockers (37). Regarding β-blockers, by recording SBP directly from the brachial artery during bicycle ergometry, Floras et al (38) showed a significant attenuation of the SBP response by chronic blockade of cardioselective β1-adrenergic receptors; but nonselective blockade of β1 and β2 adrenergic receptors did not alter this BP response.
Impact of the CST protocol
The type of CST also influences the blood pressure response. In healthy men, four progressive treadmill protocols resulted in similar maximum SBP (39), whereas in women the slope of the SBP response curve and maximum SBP observed in the Bruce and Balke treadmill protocols were significantly different (21). Treadmill and cycle ergometer exercises, with stepwise and continuous increases in exercise, produced similar maximum SBP in men (40). However, bicycle ergometry results in greater maximum SBP in the clinic (41) and in trained individuals (42), possibly due to the addition of isometric work (hand grip) or increased quadriceps activation (and thus sympathetic afferent activity). Therefore, when interpreting the BP response to CST, the type of exercise must be taken into account.
Upper limits of blood pressure during CST
As mentioned above, characteristics of an individual's phenotype influence the maximum SBP obtained in CST. In a large group of healthy individuals, maximum SBP was higher in men than in women, and higher in older adults than in younger adults (Figure 3) (43). Also, maximum SBP is higher in trained individuals than in their sedentary counterparts (23, 44), in hypertensive individuals than in normotensive individuals (25, 26), and in individuals with reduced baroreflex sensitivity (27). The ACSM and AHA recommend discontinuing CST for SBP and DBP levels greater than 250 and 115 mmHg. Art., respectively (3, 45). This criterion has not changed for decades (46), since the study presented in Fig. 1 (4), where the authors recommended without justification: “... Stress testing should be completed if SBP exceeds 250 mm Hg. Art." Similarly, the basis for the DBP criterion and the relationship of these upper BP values with an increase in negative events during physical activity are unknown (19).
Rice. 3. Maximum values of systolic blood pressure (SBP; a) and diastolic blood pressure (DBP; b) obtained in the Bruce treadmill test in men (black circles) and women (gray squares).
Mean ± SD are presented for each decade of life. The corresponding black and gray lines below and above represent the 10th and 90th percentiles for men and women, respectively. Figures use data from Daida et al (43).
Widely accepted upper values for stopping CST are based on data from a small sample of men of unknown age. Therefore, applicability across different populations is limited. Extreme increase in SBP and DBP, exceeding 320 and 250 mm Hg. Art. accordingly, was observed in healthy men during double leg presses (47). In contrast to aerobic exercise, resistance exercise secondarily increases intra-aortic pressure from straining while the glottis is closed, and this slightly reduces the increase in transmural pressure (48). There is no direct evidence that exercise increases the risk of adverse outcomes in people with hypertension (49), but this does not exclude the possibility of an adverse event from increased BP during exercise (eg, coronary or aortic dissection, cerebral hemorrhagic events). However, increased BP with exercise is transient and returns to baseline values or less after cessation of exercise (50, 51). Adherence to current CST discontinuation criteria based solely on maximal BP is a cautionary rather than an evidence-based recommendation.
When is the best time to stop training?
The load is not dangerous and natural if a person does not feel increased pressure.
The following symptoms indicate a pathological increase in blood pressure:
- breathing complications;
- blurred vision, the appearance of black spots;
- dizziness;
- retrosternal pain;
- headache in the back of the head.
If they occur, the training must be stopped. Symptoms should stop within half an hour. Otherwise, you need to call an ambulance, take nitroglycerin, and then consult a cardiologist and undergo diagnostics for the presence of pathologies.
The appearance of black floaters in the eyes
Excessive blood pressure response to CST
In addition to establishing an upper BP threshold for exercise cessation, the AHA established an excessive BP response to exercise >210 mmHg. Art. for men and >190 mm Hg. Art. for women, as well as an increase in DBP >10 mm Hg. Art. compared to the resting value or above the value of 90 mmHg. Art., regardless of gender (3). Validation of the systolic criterion appears to be based on data described in a review (52), whereas the criteria for abnormal DBP response arose from a series of studies predicting an increase in resting DBP (53). ACSM currently defines excessively elevated BP as an absolute SBP >250 mmHg. Art. or relative increase >140 mm Hg. Art. (2), however, the source of these values is unknown and the criteria have changed over time. For example, the AHA confirmed the clinical need for excessive BP values but refrained from proposing threshold values (54), whereas previous ACSM recommendations cited systolic and DBP >225 and >90 mmHg as response criteria. Art., respectively (55).
Many studies linking exaggerated BP responses to exercise with latent hypertension have not used recommended thresholds but have used arbitrary thresholds (8, 14, 15, 53, 56 – 59), values >90th or 95th percentile (11 – 59). 13) or the values of people from the top tertile (10, 60). Figure 4 provides a summary of BP thresholds used in previous hypertension-related studies of individuals with excessive BP. To date, the lowest threshold has been established by Jae et al (17) - 181 mmHg. Art. – as the most selective SBP threshold for predicting hypertension in men during a five-year follow-up. Several studies have used magnitude of change rather than absolute value to define excessive BP. Matthews et al (9) used a change in SBP >60 mmHg. Art. at 6.3 MET or >70 mm Hg. Art. at 8.1 MET; Lima et al (61) used an increase in SBP >7.5 mmHg. st./MET. For DBP, several studies have used increases >10 mmHg. Art. (9, 53, 56) or 15 mm Hg. Art. (61) with CST. Not surprisingly, the lack of consensus on the definition of excessive BP has led to discrepancies in incidence estimates ranging from 1 to 61% (59, 62).
Rice. 4. Generalized thresholds for systolic blood pressure (SBP; a) and diastolic blood pressure (DBP; b), which are used to identify excessive blood pressure responses.
Dashed lines are sex-specific thresholds recommended by the American Heart Association (AHA) (3) and the American College of Sports Medicine (ACSM) (2). Source studies are listed at the bottom of each column.
Most studies assessing excessive BP during exercise have included a narrow age group of men (middle-aged), which limits the applicability of the results to all people. A single study of young adults (25 ± 10 years), involving 76–77% of competitive male athletes, concluded that exercise BP was the best predictor of future BP (53). Several studies have assessed men and women, and similar thresholds have been applied to both sexes (8, 13, 59). Only one study examined age- and sex-specific criteria for excessive BP based on values above the age/sex 95th percentile (12). The values used were obtained from the second stage of the Bruce protocol, for both sexes, only excessive BP was associated with an increased risk of hypertension.
In addition to emphasizing the importance of DBP in predicting future events, this study poses two key questions: is the best criterion for BP, and how to obtain BP values during exercise? Limited evidence suggests that the excessive increase in blood pressure seen early in CST may be more clinically significant. Holmqvist et al (16) observed people who reached their maximum BP late in the CST without having the same risk of hypertension as people who reached that BP early in the test. To date, studies have performed manual auscultation with various sphygmomanometers or used automatic oscillometric devices. Auscultation is complicated by motion artifacts and ambient noise, and oscillometric devices assessed DBP through measurement of mean arterial pressure (63). In all cases, numerous errors and assumptions are possible, including the validity and reliability of data from each device, which are typically obtained in a homogeneous population and are not valid in others (64), and the use of DBP estimates to attribute risk.
Although there is sufficient evidence to support the association between exaggerated BP responses to exercise and the risk of latent hypertension, more rigorous methodology for identifying “abnormal” responses is required for additional factors of age, sex, fitness and comorbidities, particularly the use of a single value at peak exercise. The rate of change in BP, plotted as the slope of the curve in Figure 5, provides the most reliable approach to classifying individuals as normal or overresponsive. However, the hypertensive response to exercise will help uncover pathologies (eg, coarctation of the aorta), improve risk stratification, increase the sensitivity of exercise imaging studies, and improve the identification of strategies in cases of borderline hypertension.
Rice. 5. Changes in systolic blood pressure (SBP) relative to metabolic equivalent (MET) - shown as different colored lines for three hypothetical respondents.
Dashed lines indicate sex-specific thresholds recommended by the American Heart Association (AHA) (3) and the American College of Sports Medicine (ACSM) (2). Red and green reactions are stopped at similar levels determined by the AHA. However, the theoretical response shown in green appears to be more clinically significant. Likewise, although the red and blue lines reach similar MET (training) levels, there are clear differences in response patterns.
Generalization and directions for further research
Many clinicians express concern when the SBP response exceeds the “normal” range, but in such cases there is insufficient empirical evidence to make clinical recommendations. Moreover, arbitrarily set upper blood pressure values for stopping CST have the same drawback. We argue that the clinical utility of BP measurements can be improved under the following conditions:
In addition to the maximum/peak values obtained with CST, consider the rate of change of BP (slope of the curve), and establish the level of agreement between these two measurements.
Possibility of influence of age, gender, health status, medications and CST protocol on blood pressure values obtained in the test.
Standardize BP measurements as recommended by Sharman and LaGerche (1):
- Measure at the end of each CST step.
- Measure before ending the test, and if not possible, immediately after stopping the test.
- Use an automated device that can measure on the move (65). This limits interobserver variability. Prefer DBP data from auscultatory devices over oscillometric devices. However, caution is needed as there is little reliable data on these devices, mostly from small studies of healthy people.
- Manual measurements are suitable for experienced assessors. There are no empirical data to inform the threshold effects of training, but regular BP measurement during exercise is likely to be more beneficial than sporadic BP measurement.
Future studies should record and report BP values at which acute cardiovascular events occur during CST to properly assess risk and establish evidence-based upper limits.
Improved medical advice on the role of exercise is needed
So why are we talking about an “epidemic” of hypertension? Are our doctors letting us down? Obviously, doctors can easily identify this condition: survey results from 2000 show that hypertension is the most common diagnosis during an in-person doctor's visit (total number of visits examined in the United States was 35 million).
However, we are talking about practical advice regarding exercise; doctors are clearly not doing everything in their power. What is meant here is the recommendation “You need to exercise more. I instruct you to walk 30-45 minutes a day, 5 days a week, and please start today.”
It’s sad to realize that such a conversation is a rare occurrence in medical practice. Doctors simply don't have the knowledge to give advice about exercise. It’s much easier to write out the required prescription and give a piece of paper with recommendations for yourself to review.
conclusions
Hypertension is a leading cause of cardiovascular mortality and morbidity, but clinical BP measurements alone underestimate its prevalence in healthy individuals considered normotensive at these levels (66). We argue that CST BP measurements serve as a complementary assessment for clinical and outpatient assessment of hypertension and CVD risk, diagnosis, and prognosis. However, this approach is still hampered by the unreasonableness of previously proposed values and the lack of empirical diagnostic indicators of BP. To facilitate accurate classification of normal and excessive BP responses, existing guidelines need to be reinterpreted. Clinically significant abnormalities in BP response should be defined in terms of the rate of change in BP relative to workload or cardiac output in addition to peak values obtained during exercise. It is important to note the modulating influence of age, gender, level of training, health status and medications taken, which may be a consequence of an adaptive state (higher level of training), and not a connection with pathology. Finally, without positive clinical results, there is no need to stop CNT at high blood pressure thresholds, since there is no scientific evidence that such a reaction is associated with adverse events.
Source:
https://link.springer.com/