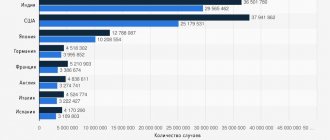
In patients with type 2 diabetes mellitus (T2DM), arterial hypertension (AH) develops in 80% of cases [1,2]. At the same time, the prevalence of hypertension among the urban population of Russia is 40%, and among the rural population - 30% [3].
In 80% of patients with T2DM, the causes of hypertension are metabolic syndrome and diabetic nephropathy. Triggering factors for the development of hypertension in metabolic syndrome are insulin resistance and hyperinsulinemia [4]. Under conditions of insulin resistance, the sympathetic nervous system is activated and the activity of sodium-potassium ATPase decreases, which ultimately leads to an increased flow of calcium ions into the smooth muscle vascular cells and their contraction. Both sympathotonia and contraction of vascular smooth muscle cells lead to an increase in blood pressure (BP). Hyperinsulinemia stimulates the proliferation of vascular smooth muscle cells, leading to an increase in the thickness of the vascular wall, a decrease in the lumen of the arteries and an increase in blood pressure. In addition, hyperinsulinemia is associated with increased reabsorption of sodium and water ions in the distal convoluted tubules of the nephron with a subsequent increase in circulating blood volume, which also contributes to hypertension. The main role in the development of hypertension in patients with diabetic nephropathy is played by increased synthesis of angiotensin II in tissues due to the activation of tissue renin-angiotensin systems, as well as as a result of the non-renin pathway of angiotensin II formation in the kidneys, vascular wall, myocardium and other organs [5].
Other causes of hypertension in patients with type 2 diabetes are stenosis of the lumen of the renal arteries or a combination of diabetes with hypertension, parenchymal kidney diseases, and hormonally active adrenal tumors.
The presence of renovascular hypertension or hypertension caused by an adrenal tumor in patients with T2DM requires appropriate surgical intervention, which, as a rule, leads to normalization of blood pressure levels or mitigation of the course of hypertension. In other cases, non-drug and drug treatment of hypertension is prescribed, the tactics of which do not depend on the specific cause of its occurrence.
The basic principles of hypertension therapy in patients with type 2 diabetes have some differences from that in patients without diabetes. It must be emphasized that the very fact of having diabetes increases the likelihood of life-threatening complications of hypertension to a high or very high risk level [6]. This means that over the next 10 years, more than 20% of such patients will develop a stroke or acute myocardial infarction due to hypertension. For this reason, the presence of grade 1 hypertension in T2DM is an indication for immediate prescription of drug treatment, even in the absence of additional risk factors and concomitant diseases. Moreover, if diabetes is detected, antihypertensive drug therapy should be started even in patients with so-called high normal blood pressure (i130/85 mm Hg) [7].
In patients with hypertension without diabetes, it is recommended to strive to reduce blood pressure to a level below 140/90 mmHg. Art. When hypertension and diabetes are combined, the recommended target blood pressure level depends on the severity of proteinuria. If it is absent or the loss of protein in the urine does not exceed 1 g per day, it is advisable to reduce blood pressure below 130/85 mm Hg. Art. If more than 1 g of protein is lost in the urine, blood pressure should be maintained below 125/75 mmHg. Art. [7].
Pharmacotherapy must be combined with non-drug treatment of hypertension, including reducing excess body weight, rational nutrition, limiting the consumption of table salt and alcohol, combating smoking, a sedentary lifestyle and stress [6]. This makes it possible to increase the sensitivity of patients to the effects of antihypertensive drugs, reduces the severity of side effects of medications, has a beneficial effect on the regulation of carbohydrate metabolism and improves the quality of life. Complex treatment of hypertension in patients with diabetes is effective only if, along with antihypertensive therapy, therapy is carried out aimed at achieving compensation for diabetes.
In the normal state of carbohydrate metabolism, drug treatment of hypertension can begin with either monotherapy or a combination of antihypertensive drugs [2,6,7]. In case of hypertension against the background of T2DM, it is recommended to carry out combination antihypertensive therapy from the very beginning [8-10]. This allows for better protection of vital organs and faster achievement of the target blood pressure level. A rationally selected combination of drugs with different mechanisms of action can provide potentiation of the hypotensive effect and mutual neutralization of the side effects of the medications used [11]. Another feature of pharmacotherapy for hypertension in T2DM is that in this case it is not recommended to start it with a combination of a diuretic and a beta-blocker, whereas in patients without diabetes this method of correcting hypertension can be considered completely justified and is often used. It should be noted, however, that research in recent years makes it necessary to reconsider existing ideas about the inappropriateness of the combined use of diuretics and beta-blockers in diabetes, which will be discussed in more detail below.
Regardless of the presence of diabetes, drug treatment of hypertension should be long-term (most often lifelong). Course prescription of antihypertensive drugs is unacceptable. The drugs used must comply with the following modern requirements of clinical pharmacology:
- the half-life of the antihypertensive drug and its active metabolite should be at least 12 hours;
- adequate control of blood pressure levels should be achieved when the drug is prescribed no more than 2 times a day;
- the residual effect of the drug (24 hours after a single dose) should be at least 50% of the maximum effect.
It is also desirable that an antihypertensive drug have 2 elimination routes from the body.
If there are appropriate indications, antihypertensive therapy should be supplemented by the prescription of lipid-lowering drugs and/or drugs containing aspirin [6,7].
Experts from WHO and the International Society for the Study of Hypertension recommend the use of diuretics, beta-blockers, calcium antagonists, angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor antagonists and alpha-blockers as first-line drugs for the treatment of hypertension. Centrally acting drugs, in particular imidazoline receptor agonists, are recommended as adjuvant agents [6].
Over the past 8-10 years, the attitude of clinicians towards the use of many antihypertensive drugs in diabetes has undergone significant changes. Back in the early 90s. last century, it was believed that the drugs of choice for the treatment of hypertension in T2DM were ACE inhibitors and alpha-blockers. The use of calcium antagonists was also allowed. In addition, even then it was believed that it was undesirable to use beta-blockers and diuretics in T2DM due to their adverse effects on lipid and carbohydrate metabolism [12].
Currently, ACE inhibitors retain their leading position as a treatment for hypertension in diabetes [2,3,11], but the use of angiotensin II receptor antagonists (for example, losartan - Cozaar) in this category of patients is considered equally effective and appropriate [13]. In the absence of contraindications, ACE inhibitors or angiotensin receptor antagonists should be prescribed to all patients in whom hypertension develops against the background of diabetes. These drugs are more effective than all other antihypertensive drugs in reducing the severity of microalbuminuria and proteinuria (by 40%). Only they, in multicenter studies, have proven their ability to slow down the rate of decline in glomerular filtration rate by 5-6 times and prevent the development of chronic renal failure in patients with diabetic nephropathy [13-16]. In addition, ACE inhibitors and angiotensin II receptor antagonists effectively prevent the development of stroke and acute myocardial infarction in hypertension [3,13,16], prevent the development of arteriolenecrosis and arteriolohyalinosis, are superior to other drugs in their ability to reduce the severity of myocardial hypertrophy, and are the drug of choice for the treatment of concomitant insufficiency blood circulation [3,11]. In multicenter studies, ACE inhibitors reduced the severity of atherosclerotic lesions of the coronary arteries [2,16], reduced mortality in acute myocardial infarction among patients with low left ventricular ejection fraction [3], and had an anticarcinogenic effect. ACE inhibitors can be used in patients with moderate chronic renal failure if the plasma creatinine level is less than 300 μmol/L. When creatinine levels are below 200 µmol/l, average therapeutic doses of ACE inhibitors are used. If plasma creatinine levels range from 200 to 300 µmol/l, the daily dose of ACE inhibitors should be reduced by 2-4 times, and the use of these drugs should be carried out under careful dynamic monitoring of plasma creatinine levels. The most common side effect of ACEIs is a dry cough, due to which 5-10% of patients are forced to stop using them. Unlike ACE inhibitors, antigen receptor antagonists do not provoke coughing.
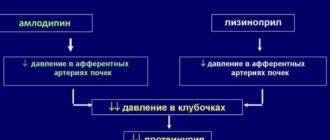
The use of calcium antagonists in patients with a combination of T2DM and hypertension is also considered completely justified, although in terms of the nephroprotective effect, these drugs are inferior to ACE inhibitors or angiotensin II receptor antagonists [2,3,13]. Multicenter studies FACET and STOP Hypertension-2 indicate that in patients with T2DM with hypertension, calcium antagonists are somewhat inferior to ACE inhibitors in terms of preventing stroke and acute myocardial infarction [17,18]. At the same time, the undoubted advantages of calcium antagonists are the ability to prevent attacks of variant (vasospastic) angina [2] and high efficiency in elderly patients, including the ability to halve the risk of developing dementia in the presence of a history of cerebral circulatory disorders [11,19]. In addition, verapamil and diltiazem reduce the severity of supraventricular arrhythmias, and diltiazem also increases the survival of patients with acute myocardial infarction without a Q wave and a decrease in left ventricular ejection fraction. In a situation where a patient with T2DM, in addition to hypertension, has concomitant circulatory failure, the choice among calcium antagonists should be amlodipine and felodipine, the safety of which in case of circulatory failure (as part of combination antihypertensive therapy) can now be considered proven [2,3].
For long-term treatment of hypertension in patients with type 2 diabetes, short-acting nifedipine should not be used, which can increase proteinuria, aggravate the manifestations of circulatory failure, and in large doses (160-200 mg per day) worsen the prognosis in patients with coronary artery disease with post-infarction cardiosclerosis [3].
In 2000, preliminary results from the multicenter ALLHAT study were published, which showed that, in terms of safety, alpha-blockers are inferior to other antihypertensive drugs. In particular, it was found that in patients with hypertension and previous cardiovascular complications who took the alpha-blocker doxazosin in combination with the diuretic chlorthalidone, the risk of stroke and circulatory failure was 19% and 100% higher, respectively, than in patients receiving one chlorthalidone and chlorthalidone in combination with the ACE inhibitor lisinopril or the calcium antagonist amlodipine [20]. Thus, the preliminary results of the ALLHAT study cast doubt on the advisability of using alpha-blockers as drugs of choice for the treatment of hypertension (including in patients with a combination of hypertension and diabetes).
In recent years, attitudes towards the use of beta-blockers and diuretics in T2DM have changed. First of all, it should be noted that modern highly selective prolonged beta-blockers (metoprolol, bisoprolol, nebivolol, atenolol, etc.), the diuretic indapamide and small doses of hydrochlorothiazide do not affect lipid and carbohydrate metabolism, without changing, in particular, the level of glycated hemoglobin and glucose content in venous blood [7,11,21]. Therefore, the use of these drugs for diabetes can be considered completely safe. In addition, the results of the multicenter SHEP study indicate that in patients with T2DM and hypertension, diuretics and beta-blockers prevented the development of stroke and acute myocardial infarction even more effectively than in patients with hypertension without diabetes [22]. Finally, multicenter studies (UKPDS 39, STOP Hypertension-2, IPPSH, CAPPP) found that in patients with diabetes and hypertension, modern cardioselective beta-blockers reduce the risk of stroke, acute myocardial infarction and cardiovascular death no less effectively than ACEI. Taken together, all these data suggest the feasibility of using cardioselective beta-blockers and diuretics for the treatment of hypertension in T2DM. Experts from the International Society for the Study of Hypertension even consider the presence of T2DM in a patient with hypertension as an additional indication for the prescription of beta-blockers.
Beta blockers have a number of advantages that other antihypertensive drugs lack. For example, only they reduce the number and duration of episodes of silent myocardial ischemia. Among antihypertensive drugs, lipophilic beta-blockers (metoprolol, nebivolol, betaxolol, bisoprolol) prevent the development of ventricular fibrillation. Only beta-blockers and ACE inhibitors prevent the development of recurrent myocardial infarction in hypertension [2,11]. Along with calcium antagonists, beta-blockers reduce angina attacks; like verapamil and diltiazem, they have a beneficial effect on supraventricular arrhythmias. ACEIs, beta-blockers and diuretics are the drugs of choice for the treatment of concomitant circulatory failure [11]. Beta-blockers such as atenolol, metoprolol and nebivolol have demonstrated the ability to reduce proteinuria regardless of the degree of blood pressure reduction.
Important advantages of diuretics include their ability to potentiate the hypotensive effect of most known antihypertensive drugs, reduce the sensitivity of the vascular wall to the action of vasopressor hormones, as well as high efficiency in elderly patients [2,11].
Of the diuretics, preference should be given to indapamide, prescribed in an average daily dose. If the patient for some reason cannot use indapamide, small doses of hydrochlorothiazide can be used instead - from 6.25 to 12.5 mg per day [21]. In diabetes, it is not advisable to use triamterene and amiloride, since these potassium-sparing diuretics have nephrotoxic properties [2].
In patients with T2DM with hypertension, the use of the imidazoline receptor agonist moxonidine may be very promising; in this category of patients, the unique spectrum of pharmacological effects of this drug can provide a number of additional advantages. Clinical studies have shown that moxonidine reduces the severity of proteinuria and slows down the rate of decline in glomerular filtration rate in diabetic nephropathy [23]. A unique property of moxonidine among other antihypertensive drugs is its ability to reduce insulin resistance in patients with T2DM. After completion of multicenter clinical trials, moxonidine has every chance to be included in the list of first-line drugs used to treat hypertension in patients with type 2 diabetes.
Since it is preferable to use combination antihypertensive therapy in patients with a combination of diabetes and hypertension, it is necessary to give a comparative description of this kind of combinations. The best organoprotective effect in T2DM in combination with hypertension has a combination of an ACE inhibitor (or an angiotensin II receptor antagonist) with a beta-blocker, which can most effectively prevent damage to the kidneys, heart and brain [2,11]. However, this combination does not always achieve the desired hypotensive effect. Therefore, in some cases, to achieve the target blood pressure level, it is advisable to add a diuretic to this combination. Combination treatment with the use of an ACE inhibitor and a calcium antagonist (sometimes with the addition of a diuretic) usually also achieves an adequate reduction in blood pressure in patients with type 2 diabetes and has a clear organoprotective effect [11,15,24]. Currently, the multicenter clinical trial VALUE-2 is being conducted, in which the effectiveness of combined treatment with an angiotensin receptor antagonist and calcium antagonist is assessed in 15,300 patients with hypertension (30% of them with T2DM). Finally, the combination of an ACE inhibitor and a diuretic allows effective control of blood pressure levels [2,7]. However, in the presence of diabetes, the use of this combination seems less rational than the combination treatment regimens discussed above, since it has a less pronounced nephro- and cardioprotective effect.
If there are contraindications to ACE inhibitors and angiotensin II receptor antagonists, combination antihypertensive therapy can be carried out using a calcium antagonist and a beta-blocker. Combinations of a calcium antagonist and a diuretic or an alpha and beta blocker seem less rational.
To increase the effectiveness of any combination antihypertensive therapy regimen in patients with T2DM, it can additionally include moxonidine as a 3rd or 4th component.
Currently, the 5-year multicenter ABCD-2 study is evaluating the effectiveness and safety of combination treatment of patients with T2DM with diabetic nephropathy and hypertension, an angiotensin receptor antagonist (valsartan) and an ACE inhibitor (captopril).
Thus, hypertension in patients with T2DM may be due to several reasons, but the principles of its treatment remain common to all patients and have some differences from the treatment tactics for patients with hypertension, which develops against the background of normal carbohydrate metabolism.
Hypertension in type 2 diabetes mellitus
One of the factors that provokes the development of type 2 diabetes mellitus is insulin resistance, i.e. decreased sensitivity of tissues to the action of insulin.
To compensate for insulin resistance, excessive amounts of insulin circulate in the blood, which itself causes an increase in blood pressure. Over time, a narrowing of the lumen of blood vessels occurs, caused by atherosclerosis, which also contributes to the occurrence of hypertension. In parallel, patients experience the development of abdominal obesity, and, as is known, it is from adipose tissue that substances that increase blood pressure are released into the blood.
This complex is called metabolic syndrome. The development of hypertension occurs much earlier than type 2 diabetes itself.
Literature
1. Thorin E., Thorin-Trescases N. Vascular endothelial aging, heartbeat after heartbeat. Cardiovasc Res. 2009 Oct 1; 84(1):24–32. 2. Makrilakis K., Bakris G. Diabetic hypertensive patients: improving their prognosis. J Cardiovasc Pharmacol. 1998; 31: Suppl. 2: S34–S40. 3. Izzo R., de Simone G., Trimarco V. at al. Hypertensive target organ damage predicts incident diabetes mellitus. Eur Heart J. epub 27 June 2013. 4. Ferrannini E. Insulin resistance versus insulin deficiency in non-insulin-dependent diabetes mellitus: problems and prospects. Endocr Rev. 1998; 19: 477–490. 5. Balletshofer BM, Rittig K., Enderle MD, Volk A., Maerker E., Jacob S., Matthaei S., Rett K., Haring HU Endothelial dysfunction is detectable in young normotensive first degree relatives of subjects with type 2 diabetes in association with insulin resistance. Circulation. 2000; 101:1780–1784. 6. Mancia G., Fagard R., Narkiewicz K. et al. 2013 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension. J Hypertens. Oct 2013; 31(10): 1925–1938. 7. Hansson L., Zanchetti A., Carruthers SG et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomized trial. HOT Study Group. Lancet. 1998 Jun 13; 351(9118):1755–1762. 8. Gradman AH, Parisé H., Lefebvre P. et al. Initial combination therapy reduces the risk of cardiovascular events in hypertensive patients: a matched cohort study. Hypertension. Feb 2013; 61(2):309–318. 9. Egan BM, Bandyopadhyay D, Shaftman SR et al. Initial monotherapy and combination therapy and hypertension control the first year. Hypertension. 2012 Jun; 59(6):1124–1131. 10. Cooper-DeHoff RM, Bird ST, Nichols GA et al. Antihypertensive drug class interactions and risk for incident diabetes: a nested case-control study. J Am Heart Assoc. 2013 Jun 10; 2 (3): e000125. 11. Borchard U. Pharmacokinetics of beta-adrenoceptor blocking agents: clinical significance of hepatic and/or renal clearance. Clin Physiol Biochem. 1990; 8 Suppl 2: 28–34. 12. Haasis R., Bethge H.. Exercise blood pressure and heart rate reduction 24 and 3 hours after drug intake in hypertensive patients following 4 weeks of treatment with bisoprolol and metoprolol: a randomized multicentre double-blind study (BISOMET). Eur Heart J. 1987 Dec; 8 Suppl M: 103–113. 13. Fogari R., Zoppi A., Pasotti C. et al. Effects of different beta-blockers on lipid metabolism in chronic therapy of hypertension. Int J Clin Pharmacol Ther Toxicol. 1988 Dec; 26 (12): 597–604. 14. Parrinello G., Paterna S., Torres D. et al. One-year renal and cardiac effects of bisoprolol versus losartan in recently diagnosed hypertensive patients: a randomized, double-blind study. Clin Drug Investig. 2009; 29(9):591–600. 15. Paterna S., Parrinello G., Di Pasquale P. et al. Medium-term effects of bisoprolol administration on renal hemodynamics and function in mild to moderate essential hypertension. Adv Ther. 2007 Nov–Dec; 24 (6): 1260–1270. 16. Zhou WJ, Wang RY, Li Y. et al. A randomized controlled study on the effects of bisoprolol and atenolol on sympathetic nervous activity and central aortic pressure in patients with essential hypertension. PLoS One. 2013 Sep 10; 8(9):e72102. 17. Haneda T., Ido A., Fujikane T. et al. Effect of bisoprolol, a beta 1-selective beta-blocker, on lipid and glucose metabolism and quality of life in elderly patients with essential hypertension Nippon Ronen Igakkai Zasshi. 1998 Jan; 35 (1): 33–38. 18. Wai B., Kearney LG, Hare DL Beta blocker use in subjects with type 2 diabetes mellitus and systolic heart failure does not worsen glycemic control. Cardiovasc Diabetol. 2012 Feb 14; 11: 14. 19. Wang B., Song WH, Liu GZ; Multi-center Cooperation Group of Bisoprolol. The effect long-term administration of a selective beta1 blocker bisoprolol on glucose metabolism in patients with essential hypertensive and type 2 diabetes mellitus Zhonghua Nei Ke Za Zhi. July 2005; 44 (7): 503–5. 20. Janka HU, Ziegler AG, Disselhoff G., Mehnert H. Influence of bisoprolol on blood glucose, glucosuria, and haemoglobin A1 in noninsulin-dependent diabetics. J Cardiovasc Pharmacol. 1986; 8 Suppl 11:S96–99. 21. Zamorano J., Rodriguez Padial L., Cosin J. et al. Amlodipine reduces predicted risk of coronary heart disease in high-risk patients with hypertension in Spain (The CORONARIA Study). J Int Med Res. 2008 Nov–Dec; 36(6):1399–1417. 22. Levine CB, Fahrbach KR, Frame D. et al. Effect of amlodipine on systolic blood pressure. Clin Ther. 2003 Jan; 25 (1): 35–57. 23. Kloner RA, Neutel J, Roth EM et al. Blood pressure control with amlodipine add-on therapy in patients with hypertension and diabetes: results of the Amlodipine Diabetic Hypertension Efficacy Response Evaluation Trial. Ann Pharmacother. 2008 Nov; 42(11):1552–1562. 24. Ersoy C., Imamoğlu S., Budak F. et al. Effect of amlodipine on insulin resistance & tumor necrosis factor-alpha levels in hypertensive obese type 2 diabetic patients. Indian J Med Res. 2004 Nov; 120(5):481–488. 25. Zanetti-Elshater F., Pingitore R., Beretta-Piccoli C. et al. Calcium antagonists for treatment of diabetes-associated hypertension. Metabolic and renal effects of amlodipine. Am J Hypertens. 1994 Jan; 7 (1): 36–45. 26. Shirure PA, Tadvi NA, Bajait CS et al. Comparative effect of fixed dose combination of Amlodipine + Bisoprolol versus Amlodipine and Bisoprolol alone on blood pressure in stage-2 essential hypertensive patients. Int J Med Res Health Sci. 2012; 1 (1): 13–19. 27. Rana R., Patil A. Efficacy and safety of bisoprolol plus amlodipine fixed dose combination in essential hypertension. Indian Pract. 2008; 61:225–234.
L.O. Minushkina
Federal State Budgetary Institution "Educational and Scientific Medical Center" of the Administration of the President of the Russian Federation, Moscow
The article discusses the role of sympathetic activation and features of the treatment of arterial hypertension (AH) in patients with diabetes mellitus (DM). The pharmacological features of amlodipine and bisoprolol are presented, emphasizing the effectiveness of using a combination of these drugs in the treatment of patients with hypertension and diabetes. Keywords:
arterial hypertension, diabetes mellitus, amlodipine, bisoprolol, fixed combination.
About the author:
Minushkina Larisa Olegovna – Doctor of Medical Sciences, Professor of the Department of Therapy, Cardiology and Functional Diagnostics of the Federal State Budgetary Institution "Universal Scientific Medical Center" of the Department of the President of the Russian Federation