Complex therapy of arterial hypertension
“Arterial hypertension” (AH) refers to the syndrome of increased blood pressure (BP). A distinction is made between primary hypertension (“hypertension”—GB) and secondary (“symptomatic” hypertension).
Hypertension is usually understood as a chronic disease, the main manifestation of which is a persistent increase in blood pressure, not associated with the presence of pathological processes in which the increase in blood pressure is caused by known, often remediable causes of “symptomatic” hypertension in modern conditions. Due to the fact that hypertension is a heterogeneous disease that has quite distinct clinical and pathogenetic variants with significantly different development mechanisms at the initial stages, hypertension is often used in the scientific literature instead of designating hypertension.
It is well known that hypertension is the most common cardiovascular disease, dangerous primarily due to its complications. Data from a number of large epidemiological studies clearly indicate that the risk of developing coronary heart disease (CHD), cerebral stroke, heart failure, and peripheral arterial diseases in the population increases significantly (sometimes several times) in individuals with elevated blood pressure compared to individuals with normal blood pressure. HELL.
The prevalence of hypertension is very high in any developed country in the world. Russia, unfortunately, is no exception in this regard. A study by S. A. Shalnova and others showed that among the adult population of Russia, 39.3% of men and 41.1% of women suffer from hypertension (Table 1).
The high prevalence of hypertension in Russia is largely the reason for the extremely high mortality rates in our country. According to the information contained in the Demographic Yearbook of Russia, in 2001, 1,253,103 people died from diseases of the circulatory system, including 475,163 people from cerebrovascular diseases (for comparison: 294,063 people died from cancer in 2001) .
Hypertension plays a special role in the pathogenesis of all types of cerebral stroke. It is believed to be the underlying cause in about 70% of cases of this disease. The Framingham Study demonstrated that the age-standardized risk of stroke among patients with hypertension (systolic blood pressure above 160 mm Hg and/or diastolic blood pressure above 95 mm Hg) was 3.1 for men and 2.1 for men. 9 for women. There is a fairly clear direct and statistically significant connection between mortality from cerebral stroke and the prevalence of hypertension in a particular country (correlation coefficient 0.78).
It can be said without exaggeration that mortality from cerebrovascular diseases in our country has become catastrophic. Thus, in data on cardiovascular mortality in various countries of the world recently published in the journal Heart (in total, data are provided for 48 countries from different parts of the world), Russia consistently ranked first in the number of deaths from cerebrovascular diseases among both men and women. Moreover, the absolute mortality rates in Russia are several times higher than in other countries. So, in 1995–1998. The age-standardized mortality rate from cerebrovascular diseases in men in Russia was 203.5 cases per 100,000 people, while in the USA it was 29.3, and in Canada it was 27.8.
All modern recommendations for the treatment of hypertension clearly define the main goal of therapy as reducing cardiovascular and renal morbidity and mortality. To achieve this goal, first of all, it is necessary to reduce blood pressure to a normal level, as well as correct all modifiable risk factors: smoking, dyslipidemia, hyperglycemia, obesity - and treatment of concomitant diseases: diabetes mellitus, etc.
Reduction of systolic and diastolic blood pressure to <140/90 mm Hg. Art. helps reduce the likelihood of developing cardiovascular complications. This has been clearly demonstrated by some studies, in particular MRFIT (Fig. 1). That is why the target blood pressure level for the treatment of hypertension is considered <140/90 mmHg. Art. Data from a number of recent studies indicate that if therapy is well tolerated, it is advisable to achieve a reduction in blood pressure to certain values, but not lower than 110/70 mm Hg. Art. In patients with hypertension and diabetes mellitus or kidney disease, the target blood pressure is <130/80 mmHg. Art.
The need to lower blood pressure can be convincingly illustrated by the fact that over the past 20 years, the implementation of a set of measures to combat hypertension in the United States has led to the disappearance of malignant hypertension, a reduction in mortality from cerebral stroke by 60%, and a 2-fold reduction in cardiovascular mortality.
Ways to achieve target blood pressure levels
Non-medicinal. Lifestyle changes are recommended for all patients with hypertension, including those receiving drug therapy, especially in the presence of risk factors. These measures include: quitting smoking, normalizing body weight (body mass index < 25 kg/m2), reducing alcohol consumption < 30 g/day in men and < 20 g/day in women, regular dynamic physical activity of 30– 40 minutes at least 4 times a week, reducing the consumption of table salt to 5 g/day, changing the diet with increasing the consumption of plant foods, reducing the consumption of animal fats, including foods rich in potassium, calcium (vegetables, fruits, grains) and magnesium (dairy products).
The recently completed Oxford Fruit and Vegetable Study and TOHP-II further clearly demonstrated the effect of a diet high in fruits and vegetables on blood pressure levels. The Oxford Fruit and Vegetable Study included 670 individuals with normal blood pressure. Everyone in the study group was required to follow a diet enriched with vegetables and fruits, while the control group was not given any dietary recommendations. The observation period was 6 months. Daily consumption of vegetables and fruits in the main group increased by 112 g, in the control group - by 8 g. Compliance with the diet was associated with a decrease in systolic blood pressure by an average of 2.0 mm Hg. Art., and diastolic - by 1.6 mm Hg. Art. (p < 0.05), while in the control group the first indicator increased by 1.4 mm Hg. Art., and the decrease in diastolic blood pressure was only 0.3 mm Hg. Art. However, no dynamics associated with cholesterol levels were noted in any of the groups.
Drug therapy. The main indication for prescribing antihypertensive therapy is the degree of cardiovascular risk (Table 2).
For grade I and II hypertension in patients with a high or very high risk of developing cardiovascular complications, antihypertensive drugs should be prescribed immediately. With a moderate risk, observation for 3 months with regular blood pressure monitoring is acceptable before deciding to start therapy. Treatment is prescribed for a sustained increase in blood pressure > 140/90 mmHg. Art.
In the low-risk group, a 3- to 12-month observation period and non-pharmacologic therapy are recommended before initiating drug treatment. The indication for starting such treatment is a stable blood pressure level in the range of 140–159/90–99 mmHg. Art.
In case of grade III hypertension, antihypertensive drug therapy should be immediately prescribed.
In addition to therapy with antihypertensive drugs, patients at high risk of cardiovascular complications are prescribed therapy aimed at preventing other risk factors, primarily impaired lipid metabolism. Reducing the risk of complications is achieved by prescribing anticoagulants, primarily acetylsalicylic acid.
Main groups of antihypertensive drugs
In the Russian recommendations for the treatment of hypertension, the second revision, presented at the Russian National Congress of Cardiologists in 2005, the group of drugs recommended for the treatment of hypertension, in addition to diuretics, β-blockers, calcium antagonists (CA), angiotensin-converting enzyme inhibitors (ACE inhibitors), receptor blockers angiotensin I (ARB), α-blockers, I1-imidazoline receptor agonists (AIR) are included. The latter play a certain role in the treatment of patients with metabolic syndrome and diabetes mellitus; it is noted that they can be prescribed as monotherapy or in combination with other antihypertensive drugs if other drugs are ineffective.
Monotherapy or combination therapy
When choosing between monotherapy and combination therapy, the doctor should focus primarily on the initial level of blood pressure, the presence of complications or their absence. Based on the results of multicenter international studies, it can be assumed that monotherapy will be effective mainly in patients with stage I hypertension. Thus, according to the ALLHAT study, monotherapy was effective in only 60% of patients with stage I and II hypertension; in the HOT study, only 25–50% of patients with stage I and III hypertension remained on monotherapy: in studies that included patients with diabetes, the vast majority of patients received at least two drugs, whereas in diabetic nephropathy, to achieve the target blood pressure level on average, two to three drugs were required in addition to basic therapy.
In accordance with the initial blood pressure level, the presence of complications and risk factors, it is advisable to start therapy with either a low dose of one drug or a low-dose combination.
The advantage of monotherapy is that if treatment is ineffective at the initial stage, the doctor can either change the class of the drug or increase the dose of the previously taken drug, this will make it possible to select the drug individually for each patient. However, in most cases, such a procedure is labor-intensive, in addition, it often leads to a loss of trust not only in the therapy being performed, but also in the attending physician, which, in turn, does not contribute to increasing compliance.
An obvious disadvantage of a treatment regimen that involves starting treatment with two drugs at once, even in low doses, is the danger of prescribing an “unnecessary” drug to the patient. However, combination therapy still has more advantages: firstly, the use of drugs with different mechanisms of action makes it possible to more effectively control hypertension and its complications; secondly, when using combination therapy, it becomes possible to prescribe drugs in low doses, while reducing the likelihood of developing undesirable effects; thirdly, fixed drug combinations have now become available, allowing two drugs to be prescribed in one tablet, which significantly increases compliance.
Currently, the following combinations of drugs are considered effective and safe: ACE inhibitors + diuretics; diuretics + β-blockers; diuretics + ARBs; calcium antagonists (CA) (dihydropyridine) + β-blockers; AA (dihydropyridine) + ARB; AA + ACEI; AA (dihydropyridine) + diuretics; α-blockers + β-blocker (Fig. 2).
| Figure 2. Possible combinations of different classes of antihypertensive drugs. (From European guidelines for the treatment of hypertension) |
Guided by numerous studies demonstrating the positive effects of individual drug combinations on endpoints, leading pharmaceutical companies began to offer combination antihypertensive drugs. Thus, in recent years, combinations of long-acting drugs with fixed dosages have appeared on the pharmacological market: diuretic + ARB (co-diovan, gizaar); ACE inhibitor + diuretic (co-renitec, noliprel, renipril GT); AK (dihydropyridine) + β-blocker (Lomax); diuretic + β-blocker (atehexal compositum); today the only combination of AK + ACEI (Tarka).
The question of the benefits of using one or another group of antihypertensive drugs, one or another combination is quite complex and ambiguous, however, the results of multicenter randomized studies generally prove that the appointment of any of the existing treatment regimens for hypertension reduces the overall risk of cardiovascular events, and the lower the blood pressure , the lower the above-mentioned risk.
In all cases, it is recommended to use long-acting drugs that provide an effect throughout the day; this reduces blood pressure variability and, possibly, provides better organ protection and a reduction in the number of cardiovascular complications. In addition, due to the convenience of a single dose of drugs, patient adherence to treatment increases.
Modern international recommendations for the treatment of hypertension clearly define when and which drugs the doctor should give preference to. The main argument in favor of prescribing a specific group of drugs are the so-called additional indications. Thus, additional indications for the prescription of dihydropyridine ACs are old age, isolated systolic hypertension, the presence of angina pectoris, atherosclerosis of the peripheral arteries, in particular atherosclerosis of the carotid arteries. Pulse-lowering non-dihydropyridine AKs, diltiazem and verapamil-SR, are advisable to use in patients with supraventricular tachycardia. It has been proven that ARBs slow down the progression of chronic renal failure in hypertension in combination with diabetes mellitus, and also ensure the reverse development of left ventricular hypertrophy. An aldosterone receptor blocker (spironolactone) has been effective in patients with chronic heart failure and patients who have had myocardial infarction.
All these additional indications arise from the results of specific controlled studies that have demonstrated the benefits of dihydropyridine AKs in these categories of patients. It should be remembered that dihydropyridine AKs are one of the few groups of drugs that a doctor can prescribe to pregnant women with hypertension.
When selecting therapy for hypertension, practicing physicians do not always follow international recommendations and often determine treatment priorities themselves. Interestingly, AKs are the most commonly prescribed drugs worldwide: the AK market accounts for about 35%, which is significantly larger than that of other groups of antihypertensive drugs; Thus, the market for ACEIs and ARBs combined accounts for only 39% of the global market (16 and 23%, respectively). In Russia, the situation is fundamentally different: in terms of frequency of use, ACEIs and ARBs confidently lead, occupying 47% of the market, while ACs account for only 13.9%, which practically coincides with the frequency of use of diuretics. However, what is even more alarming is the fact that we are still mainly prescribing first-generation AKs, regular treatment of which, as noted in a number of studies, cannot be considered either sufficiently effective or safe. A striking example of this is the analysis of the sales structure of AKs in one of the pharmacies in the center of Moscow, carried out in the second quarter of 2003, which showed that 48% of sales of all dihydropyridine AKs still account for short-acting first-generation drugs.
Speaking about the effectiveness and safety of long-term use of antihypertensive drugs used for the treatment of hypertension, it is necessary to recall that all large studies examining the effect on “endpoints” have been and are being conducted only with original drugs. The only drawback of original drugs is their high cost, which often limits the possibilities of complex therapy. The creation of generics - copies of original drugs - significantly reduces the cost of treatment, but raises the problem of assessing the equivalence of generics to original drugs. Today, about 60 generics of enalapril, about 30 generics of amlodipine, more than 10 generics of indapamide are registered in Russia, and recently the first generic fosinopril, bioequivalent to the original drug, has appeared
It is clear that it is difficult for a practicing physician to understand such a variety of drugs, especially since manufacturing companies in most cases do not provide data on pharmaceutical and pharmacokinetic equivalence to the original drug. Familiarization of doctors with such data could significantly ease the problem of choosing a drug. In the absence of such information, specialists can only rely on personal experience, as well as the results of a few clinical studies comparing original drugs and generics or different generics with each other.
Literature
- Shalnova S. A., Deev A. D., Vikhireva O. V. et al. Prevalence of arterial hypertension in Russia. Awareness, treatment, control // Disease prevention and health promotion. 2001. No. 2. P. 3–7.
- Demographic Yearbook of Russia - 2002. M., 2002.
- D'Agostinio RB, Wolf PA, Belanger AJ, Kannel WB Stroke risk profile: adjustment for antihypertensive medication: the Framingham Study//Stroke. 1994; 25:40–43.
- Mancia G. Prevention and treatment of stroke in patients with hypertension//Clin. Therapeutics. 2004; 26:631–648.
- Levi F., Lucchini F., Negri E., La Vecchia C. Trends in mortality from cardiovascular and cerebrovascular diseases in Europe and other areas of the world//Heart. 2002; 88: 119–124.
- Opie LH, Schall R. Evidence-based evaluation of calcium channel blockers for hypertension: equality of mortality and cardiovascular risk relative to conventional therapy//J. Am. Coll. Cardiol. 2002; 16: 39 (2): 315-22. Erratum in: J. Am. Coll. Cardiol. 2002; 17:39(8):1409–1410.
- Staesssen J., Ji-Guang Wang, Thijs L. Calcium-channel blockade and cardiovascular prognosis: recent evidence from clinical outcome trials // Am. J. Hypertens. 2002; 15:85–93.
- Poole-Wilson P., Lubsen J., Kirwan B. et al. Effect of long-acting nifedipine on mortality and cardiovascular morbidity in patients with stable angina requiring treatment (ACTION trial): a randomized controlled trial//Lancet. 2004; 364:849–857.
- Guidelines Committee. 2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension//J. Hypertension. 2003; 21: 1011–1053.
- Martsevich S. Yu., Kutishenko N. P., Dmitrieva N. A. The problem of choosing a drug in the treatment of arterial hypertension // Cardiovascular therapy and prevention. 2004. No. 3.
- VNOK Expert Committee. Prevention, diagnosis and treatment of arterial hypertension. Russian recommendations (second revision) // appendix to the railway. "Cardiovascular therapy and prevention." 2004.
- Schrader J., Luders S., Kulschewski A. et al. MOSES Study Group. Morbidity and Mortality After Stroke, Eprosartan Compared with Nitrendipine for Secondary Prevention: principal results of a prospective randomized controlled study (MOSES)//Stroke. 2005; 36(6):1218–1226.
V. A. Egorov Yu. E. Semenova, Candidate of Medical Sciences Yu. V. Lukina, Candidate of Medical Sciences State Research Center for Preventive Medicine, Moscow
Classification
Drugs that reduce the stimulating effect of adrenergic innervation on the cardiovascular system: 1. Agonists of imidazoline I1 receptors 2. Central a2-adrenergic agonists 3. Receptor blockers: • a-adrenergic blockers; • b-adrenergic blockers; • a, b-adrenergic blockers.
Vasodilators: 1. Calcium channel blockers 2. Potassium channel activators 3. Arteriolar vasodilators 4. Arteriolar and venous vasodilators.
Diuretics (diuretics).
Drugs that affect the functions of angiotensin II: 1. Angiotensin-converting enzyme inhibitors (ACEIs) 2. Angiotensin II AT1 receptor blockers 3. Vasopeptidase inhibitors.
The vasomotor center of the medulla oblongata regulates blood pressure with the participation of presynaptic receptors - imidazoline I1 receptors and a2 adrenergic receptors. These receptors, stabilizing the presynaptic membrane, prevent the release of norepinephrine to pressor neurons, which is accompanied by a decrease in central sympathetic tone and an increase in vagal tone. I1 receptors localized in the ventrolateral nuclei of the medulla oblongata are of primary importance in maintaining normal blood pressure; a2 receptors in the nucleus of the solitary tract play a lesser role. A probable endogenous ligand of imidazoline receptors is the decarboxylated metabolite of arginine, agmantine.
Tolerability of ACE inhibitors
The subject of special attention of pervostolniks, as specialists dispensing the drug, is the side effects of ACE inhibitors. Despite the generally favorable safety profile, adverse reactions are the weak link of drugs in this group.
What should I warn the client about?
- While taking ACE inhibitors, a dry cough develops in 1–10% of cases [6]. Different members of the group practically do not differ from each other in their ability to cause it, and replacing one ACE inhibitor with another does not improve tolerability in this regard [11].
- When taking single-agent ACEIs, Quincke's edema can extremely rarely occur (but more often than when taking other antihypertensive drugs) [2]. It is believed that drugs in this group do not cause this complication, but alleviate its occurrence in predisposed patients. When releasing ACE inhibitors, it is appropriate to emphasize that if difficulty breathing and shortness of breath occur, you should immediately contact your doctor [11].
The cause of cough while taking ACE inhibitors has not been fully determined. It is assumed that the leading role is played by the accumulation of bradykinin in the bronchial mucosa, which is activated by blockade of angiotensin II [11].
Vasopeptidase inhibitors
Omapatrilat has the properties of an ACE inhibitor and a vasopeptidase inhibitor (neutral endothelial endopeptidase2). Blockade of vasopeptidase prevents the proteolysis of natriuretic peptides, bradykinin and adrenomedullin. This provides a pronounced hypotensive effect, improves renal blood flow, increases the excretion of sodium and water ions, and also inhibits the production of collagen by fibroblasts of the heart and blood vessels. The clinical effectiveness of omapatrilat in angina pectoris and CHF was revealed (decreased mortality, increased exercise tolerance, improved functional class).
Diuretics
The mechanism of the antihypertensive action of diuretics is associated with the ability of the drugs to reduce the volume of circulating fluid, primarily by reducing the reabsorption of sodium ions in the renal tubules. As a result of a decrease in fluid load, the total peripheral vascular resistance and blood pressure levels decrease. The hypotensive effect of diuretics is complemented by the ability of these drugs to reduce the sensitivity of the vascular wall to natural vasopressors (including adrenaline), in the maintenance of which sodium ions participate.
The most widely used antihypertensive drugs are thiazide and thiazide-like diuretics: hydrochlorothiazide, chlorthalidone, indapamide, etc. Loop diuretics are used only to relieve hypertensive crises. Long-term use of any diuretics is dangerous for the development of electrolyte imbalance, therefore, when prescribing them, it is recommended to monitor the content of electrolytes in the blood plasma. When using thiazide and thiazide-like diuretics daily in small doses, the risk of complications of therapy is minimized without a significant loss of the necessary hypotensive effect.
Thiazide and thiazide-like diuretics may be preferred for isolated systolic hypertension in older people, with concomitant CHF, and in women with hypertension in the perimenopausal period. Diuretics are convenient to supplement already prescribed treatment regimens to achieve the target blood pressure level.
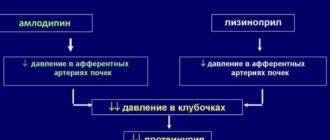
Calcium antagonists (slow calcium channel blockers)
According to the classification according to B. Nauler, all calcium antagonists (CA) are divided into 3 groups: derivatives of dihydropyridines (nifedipine, isradipine, amlodipine, etc.), benzothiazepines (diltiazem), phenylalkylamines (verapamil). AA limit the flow of Ca2+ ions into the cell, reducing the ability of the muscle fiber to develop contraction. Due to the limitation of the entry of Ca2+ ions into the cell, 3 main effects develop, to one degree or another characteristic of all AKs: a decrease in myocardial contractility (negative inotropic effect), a decrease in the tone of smooth muscles of the arteries (vasodilating effect), a change in the excitation threshold of cardiomyocytes of the conduction system (characteristic of pulse – reducing AKs – verapamil and diltiazem). It is known that dihydropyridine AKs can increase heart rate, especially at the initial stage of treatment.
AKs reduce the tone of arterioles, which is mainly responsible for their antihypertensive effect. Due to this, renal blood flow increases in parallel, which provides a small natriuretic effect, complemented by a decrease in aldosterone formation under the influence of AA. Blocking Ca2+ ions at the level of platelets leads to a decrease in their aggregation readiness.
Being highly active agents, AKs have a number of advantages, which are often called “metabolic neutrality”: the drugs of the group do not affect lipid, carbohydrate, mineral and purine metabolism. Since AKs improve coronary and cerebral blood flow, their use is justified in hypertension with concomitant coronary artery disease or cerebrovascular insufficiency.
Imidazoline I1 receptor agonists
Drugs belonging to this group - moxonidine, rilmenidine - stimulate imidazoline receptors, which leads to inhibition of the activity of the vasomotor center and the sympatho-adrenal system. Peripheral vascular resistance, cardiac output and, as a result, blood pressure decrease.
It should be remembered that imidazoline receptor agonists can increase bradycardia and inhibition of atrioventricular conduction when used together with beta-blockers.
Despite the fact that imidazoline receptor agonists effectively control blood pressure, the therapeutic potential of this group of drugs (impact on the prognosis of patients with hypertension, rational combination with other drugs) requires further study.
a1-blockers
The mechanism of antihypertensive action of α1-adrenergic blockers (prazosin, doxazosin) is the competitive blockade of α1-adrenergic receptors of vascular smooth muscle cells, which prevents excessive stimulation of these receptors by catecholamines. There is a decrease in peripheral vascular resistance and a drop in blood pressure.
An important property of a1-blockers is their beneficial effect on the lipid profile (increasing the content of anti-atherogenic high-density lipoproteins, reducing atherogenic low-density lipoproteins and triglycerides). When using a1-adrenergic blockers, there is a high risk of developing hypotension of the first dose, compensatory tachycardia, and increased urination (a1-adrenergic receptors of subtype A are located in the prostatic part of the urethra).
Angiotensin-converting enzyme inhibitors
ACE inhibitors are a group of drugs that affect numerous pathological links, leading to functional and structural changes that underlie various diseases of the cardiovascular system. The mechanism of action of ACE inhibitors is the binding of zinc ions in the active center of the angiotensin-converting enzyme, the key enzyme of the RAAS, and blocking the reaction of the transition of angiotensin I to angiotensin II, which reduces the activity of the RAAS both in the systemic circulation and at the tissue level (kidneys, myocardium, brain). In parallel, due to ACE inhibition, the degradation of bradykinin is inhibited, which also promotes vasodilation. As a result, systemic arterio- and venodilation occurs, pre- and afterload on the heart decreases, and in the presence of left ventricular myocardial hypertrophy, the process of its reverse development begins (cardioprotection). A similar process is observed in the muscle layer of arterial vessels (angioprotection). ACE inhibitors inhibit the proliferation of mesangial cells in the kidneys, which is used in nephrology (nephroprotection). Decreased aldosterone production leads to decreased reabsorption of sodium and water in the proximal and distal tubules of the nephrons.
ACE inhibitors are preferred if a patient with hypertension has concomitant CHF, post-infarction cardiosclerosis, diabetes mellitus and its complications (including nephropathy). The ability of ACE inhibitors to restore endothelial function is used when the patient has dyslipidemia and diffuse atherosclerotic lesions. When prescribing ACE inhibitors, the dose of other antihypertensive drugs (especially thiazide diuretics) should be adjusted if the patient is taking them. The decrease in blood pressure due to ACE inhibitors in most cases occurs smoothly over several weeks. Despite the fact that ACE inhibitors are quite well tolerated in most cases, you should always remember the possibility of developing the following adverse reactions characteristic of this group of drugs: dry cough, hyperkalemia and impaired renal function, angioedema (at any time of treatment).
ACE inhibitors are contraindicated during pregnancy due to the risk of teratogenies, unilateral or bilateral renal artery stenosis, aortic stenosis, mitral stenosis, and obstructive hypertrophic cardiomyopathy.
Medicines affecting the renin–angiotensin system
The renin–angiotensin–aldosterone system (RAAS) plays an important role in the regulation of blood pressure, cardiac activity, and water and electrolyte balance. Its activity increases with arterial hypertension, chronic heart failure and diabetic nephropathy. In acute myocardial infarction, the activity of the RAAS increases already on the first day; in complicated myocardial infarction, excessive activation of the RAAS persists long after the patient is discharged from the hospital. High renin activity and increased levels of angiotensin II in the blood are indicators of an unfavorable prognosis in patients with cardiovascular diseases.
For pharmacological blockade of the RAAS, ACE inhibitors and non-peptide angiotensin II receptor antagonists are used.