Treatment of arterial hypertension: combination of drugs and combination drugs
About the article
28514
0
Regular issues of "RMZh" No. 10 dated 05/05/2010 p. 708
Category: Cardiology
Authors: Vertkin A.L. 1, Topolyansky A.V. 2 1 FSBEI HE MGMSU im. A.I. Evdokimov Ministry of Health of Russia, Moscow, Russia 2 State Budgetary Educational Institution of Higher Professional Education “MGMSU named after. A.I. Evdokimov" Ministry of Health of the Russian Federation, Moscow
For quotation:
Vertkin A.L., Topolyansky A.V. Treatment of arterial hypertension: combination of drugs and combination drugs. RMJ. 2010;10:708.
When selecting antihypertensive therapy, from the very first steps the doctor has to decide the problem: is it possible in this case to get by with one drug (monotherapy) or the use of the most effective drug will be insufficient. It is possible to achieve the target blood pressure level using monotherapy with any antihypertensive drug in less than half of the patients; Combination therapy was required in 45% of patients in the SHEP (Systolic Hypertension in the Elderly Program) trial, 62% in the ALLHAT (Antihypertensive and Lipid–Lowering treatment to prevent Heart Attack Trial), 63% in the HOT (Hypertension Optimal Treatment) trial, 80 % in the INVEST study (Verapamil SR/Trandolapril Study), in the LIFE study (Losartan Intervention For reduction in hypertension study) – 92%.
According to the Recommendations of the Russian Medical Society on Arterial Hypertension (RMSHA) and the All-Russian Scientific Society of Cardiology (VNOK) in 2008, treatment of arterial hypertension can begin with low-dose combination therapy, followed by increasing the amount and/or doses of the drug if necessary, and full-dose combination therapy can be prescribed at the start of treatment for patients with blood pressure ≥ 160/100 mmHg. with a high and very high risk of cardiovascular complications. At the same time, excessive therapeutic activity often results in so-called polypharmacy, when several (sometimes many!) drugs are simultaneously prescribed without sufficient justification for the use of each of them; Therefore, when prescribing combination therapy, drug interactions should be assessed from the standpoint of effectiveness and safety, as well as patient comfort and cost of course treatment. According to domestic recommendations, drugs used in combination must meet a number of requirements: – have a complementary effect; – achieve improved results when used together; – drugs must have similar pharmacodynamic and pharmacokinetic parameters, which is especially important for fixed combinations. All the advantages of combination therapy are manifested in the case of a rational combination of antihypertensive drugs; if the combination is not absolutely recommended, but is not prohibited, then it is considered possible; if, when used together, drugs do not potentiate their hypotensive effect or side effects increase, the combination is considered irrational (Table 1). It should be noted that, in contrast to the European recommendations (EOAG/EOC, 2007), the Russian recommendations do not exclude the use of low doses of thiazide diuretics (6.25 mg) in combination with highly selective beta-blockers or those with vasodilating properties (in such a combination there are negative metabolic effects drugs should be minimal), as well as a combination of b- and a-blockers (in particular, in men with arterial hypertension and benign prostatic hyperplasia). The combination of a diuretic and a calcium antagonist raises certain doubts: according to Boger-Megiddo I., et al. (2010), it is associated with an increased risk of myocardial infarction compared to combinations of a diuretic and a beta-blocker and a diuretic and an ACE inhibitor. In recent years, the combination of ACE inhibitors and calcium antagonists has attracted increasing interest. This was greatly facilitated by the publication of the results of the Anglo-Scandinavian Cardiac Outcomes Trial-Blood PressureLowering Arm (ASCOT-BPLA) study on the comparative use of a combination of amlodipine and perindopril, on the one hand, and a combination of atenolol and bendroflumethiazide, on the other. The severity of the decrease in blood pressure, the incidence of non-fatal myocardial infarction, including painless forms, as well as death from coronary artery disease in the two groups of patients did not differ significantly, however, in the amlodipine ± perindopril group compared with the atenolol ± bendroflumethiazide group, a decrease in the risk of developing non-fatal myocardial infarction was found by 13 %, all coronary events and procedures by 16%, overall mortality by 11%, cardiovascular mortality by 24%, fatal and non-fatal strokes by 23%. Efficacy of fixed combinations of a calcium antagonist with an ACE inhibitor (amlodipine at a dose of 5–10 mg + benazepril at a dose of 10–20 mg) and an ACE inhibitor with a thiazide diuretic (benazepril at a dose of 10–20 mg + hydrochlorothiazide at a dose of 12.5–25 mg) was compared in The Avoiding Cardiovascular Events through Combination Therapy in Patients Living with Systolic Hypertension (ACCOPLISH) study, which lasted 5 years and included 11,400 hypertensive patients with systolic blood pressure >160 mmHg. over the age of 55 years, obese, with cardiovascular or renal disease or target organ damage; 60% of them suffered from type 2 diabetes. When taking a combination of a calcium antagonist with an ACE inhibitor, a slightly more pronounced hypotensive effect was noted, and cardiovascular morbidity and mortality were significantly lower by 20%. The efficacy and safety of a fixed combination of amlodipine and lisinopril compared with the isolated use of each component was assessed in the Hungarian multicenter study (HAMLET), conducted in Hungary. The randomized, placebo-controlled (at baseline), double-blind study included 195 patients with untreated or poorly controlled hypertension (BP 140–179/90–99 mmHg). It has been shown that a fixed combination of amlodipine with lisinopril can more significantly reduce the levels of systolic and diastolic blood pressure with a lower incidence of side effects. The number of patients who achieved target blood pressure (below 140/90 mmHg) was 90% in the combination therapy group, 79% in the amlodipine group and 75% in the lisinopril group. From the point of view of ensuring the comfort of treatment, instead of several individual drugs, it is sometimes advisable to use combination drugs - dosage forms containing two or more active pharmacological substances. The advantage of combination drugs compared to combination therapy with several drugs is psychological and social comfort (it is much more convenient to take one tablet or take one inhalation than several). Sometimes this turns out to be more cost-effective, since the cost of combination drugs is usually less than the cost of components prescribed separately. The disadvantages of combined drugs are due to the “fixed” ratio of the drugs included in them and often the non-synchronism of the maximums of their effects (for example, in Korenitek, the diuretic effect is ahead of the vasodilator). Features of the use of combined agents: – indicated for patients who really need combination therapy; – should be used only during the “typical” course of the disease (since the pharmacologically active substances are included in the combination drug in the most common ratio, calculated for the “typical” course of the disease); – are more often used at the stage of maintenance therapy (rather than at the stage of selecting drug treatment), since the fixed nature of the ingredients excludes the possibility of promptly changing doses and correcting their ratio; – are the drugs of choice for “undisciplined” patients who require lifelong treatment. Examples of combined antihypertensive drugs are presented in Table 2. In recent years, a new combination drug Equator (Gedeon Richter, Hungary), which is a combination of 10 mg of lisinopril and 5 mg of amlodipine, has entered clinical practice. The prolonged action of the drugs included in its composition ensures 24-hour blood pressure control with a single dose of the drug. The pronounced hypotensive effect of Equator is due to the potentiation of the effect of its components: lisinopril reduces the activity of the renin-angiotensin and sympatho-adrenal systems, the activation of which reduces the effectiveness of amlodipine, and the negative sodium balance caused by amlodipine enhances the hypotensive effect of lisinopril. The likelihood of developing side effects is reduced, namely: - swelling of the legs, which occurs while taking dihydropyridines due to dilatation of precapillary arterioles and an increase in intracapillary hydrostatic pressure (ACE inhibitors, causing dilatation of postcapillary venules, reduce hydrostatic pressure in the capillaries); – tachycardia, developing as a reaction to vasodilation (ACE inhibitors, by suppressing the formation of angiotensin II, reduce the release of norepinephrine and reduce central sympathetic activity). The combined use of an ACE inhibitor and a calcium antagonist leads to a decrease in glomerular pressure and albumin excretion; the renoprotective effect may be beneficial in patients with diabetic nephropathy. The metabolically neutral components of the drug allow us to recommend its use in metabolic syndrome. All this allows us to consider the use of the combined drug Equator promising for arterial hypertension, including in patients with left ventricular myocardial hypertrophy, coronary artery disease, atherosclerosis of the carotid and peripheral arteries, metabolic syndrome and diabetes mellitus, chronic renal failure, etc.
References 1. Boger–Megiddo I., Heckbert SR, Weiss NS et al. Myocardial infarction and stroke associated with diuretic based two drug antihypertensive regimens: population based case–control study. BMJ. 2010, 25; 340:c103. 2. Dahlof B., Sever PS, Poulter NR et al. Prevention of cardiovascular events with an attihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo–Scandinavian Cardiac Outcomes Trial–Blood Pressure Lowering Arm (ASCOT–BPLA): A multicentre randomized controlled trial. Lancet. 2005; 366:895–906. 3. Jamerson K, Weber MA, Bakris GL et al.; ACCOMPLISH Trial Investigators. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med. 2008; 359(23): 2417–2428. 4. Farsang C. A HAMLET Vizsgalok neveben. A lisinopril es az amlodipin kombinaciojanak elonyei az antihypertensiv terapiaban. A Hypertoniaban adott AMlodipin 5 mg es Lisinopril 10mg tablettak hatekonysaganak es toleralhatosaganak osszehasonlito vizsgalata kulon es Egyutt alkalmazott Terapiakent (HAMLET). Multicentrikus vizsgalat eredmenyei. Hypertonia es nephrologia, 2004; 8(2):72–8.
Content is licensed under a Creative Commons Attribution 4.0 International License.
Share the article on social networks
Recommend the article to your colleagues
Arterial hypertension (AH) is one of the most pressing health problems both in Russia and throughout the world. This is due to the high prevalence and high risk of its complications - coronary heart disease (CHD), cerebral strokes, heart and kidney failure. The prevalence of hypertension in economically developed countries reaches 25% [1].
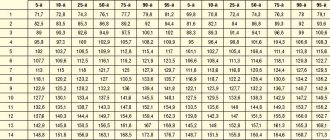
In Russia, 40% of men and women over 18 years of age have elevated blood pressure (BP) [2]. According to Russian recommendations for the diagnosis and treatment of hypertension, the strategic goal of therapy for this disease is to reduce the risk of cardiovascular complications (CVC) as much as possible. The most important condition for effective antihypertensive therapy is adequate blood pressure control, i.e. achieving its target level, which is taken as blood pressure
However, in Russia, only 5.7% of men and 17.5% of women with hypertension achieve target blood pressure levels. If you do not increase the effectiveness of therapy, i.e., do not increase the proportion of adequately treated patients with hypertension, you cannot count on a turning point in reducing cardiovascular risk.
Currently, it is possible to use two strategies for treating hypertension to achieve target blood pressure: monotherapy and combination treatment (see figure). Monotherapy is based on finding the optimal drug for a particular patient, and switching to combination therapy is advisable only if the latter has no effect. Combination therapy already at the start of treatment involves the selection of an effective combination of drugs with different mechanisms of action.
Each of these approaches has its own advantages and disadvantages. The advantage of monotherapy is that if the drug is successfully selected, the patient will not need to additionally take another drug. However, as a rule, with monotherapy it is possible to achieve target blood pressure on average only in 30–40% of patients with hypertension. This is quite natural, since one class of drugs is not able to control all pathogenetic mechanisms of increased blood pressure: the activity of the sympathetic nervous system and the renin-angiotensin-aldosterone system, volume-dependent mechanisms. In addition, monotherapy requires the doctor to painstakingly search for the most optimal antihypertensive drug for the patient with frequent changes in drugs and their dosages, which often deprives the doctor and the patient of confidence in success and ultimately reduces adherence to treatment. This is especially true for patients with mild and moderate hypertension, most of whom do not experience discomfort from increased blood pressure and are not motivated to treatment.
The disadvantage of combination therapy is the inconvenience associated with the fact that the patient has to additionally take one more, and sometimes several, drugs. However, in most cases, the prescription of antihypertensive drugs with different mechanisms of action allows, on the one hand, to achieve target blood pressure, and on the other hand, to minimize the number of side effects. Combination therapy also makes it possible to suppress counterregulatory mechanisms of increased blood pressure. Thus, the transition to combination therapy, which allows effective control of various mechanisms of increased blood pressure, gives hope for increasing the effectiveness of antihypertensive therapy.
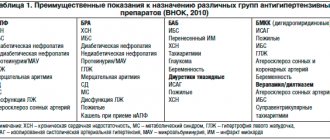
There are various combinations of antihypertensive drugs. Among the combinations of two drugs, the following are considered effective and safe: diuretic + beta-blocker; diuretic + ACE inhibitor (ACE inhibitor); diuretic + angiotensin II receptor antagonist (ARA); dihydropyridine calcium antagonist + beta-blocker; calcium antagonist + ACE inhibitor; calcium antagonist + diuretic; alpha-blocker + beta-blocker; centrally acting drug + diuretic. In addition, combinations of an ACE inhibitor, a calcium antagonist, an ARA and a diuretic with an I1 imidazoline receptor agonist are possible. The most popular in Russia is the combination of an ACE inhibitor and a diuretic. As the results of the Pythagoras study show, almost a third of doctors in Russia prefer a combination of these drugs [4].
The most important step towards improving the strategy of combination therapy was the creation of fixed combinations of antihypertensive drugs (two components in one tablet), which significantly improve patient adherence to therapy. However, along with the advantages (the ability to take one tablet containing two drugs), this approach also has serious disadvantages. Thus, the doctor cannot vary the doses of each of the drugs included in the combination, which complicates treatment, especially when adverse reactions occur that are clearly related to one of the components included in the combination. To avoid such difficulties, it was necessary to create several different dosage forms, which may partially alleviate the problem (for example, the drugs Enap-H and Enap-HL, containing different doses of the diuretic), but does not solve it completely.
In this regard, it is of interest to create non-fixed combinations containing two drugs in one blister, which will allow, if necessary, to vary the doses of each of them. The first drug of this type in Russia was Enzix - a combination of enalapril with indapamide.
The creation of this form of the drug was largely facilitated by the results of the multicenter study EPIGRAF, in which doctors from 38 clinics from 17 cities of Russia took part [5]. In total, the study included 550 patients with grades II–III hypertension (initial systolic blood pressure > 160 mm Hg), and among them there were patients not only with essential, but also with symptomatic hypertension. A feature of this study was that already at the beginning of treatment, patients were prescribed a combination of enalapril and indapamide. Moreover, if the dose of indapamide was constant - 2.5 mg, then the dose of enalapril varied depending on the initial blood pressure level. However, doctors had the opportunity to adjust doses depending on the achievement of the target blood pressure level within 14 weeks. The average dose of enalapril in the study was 15.2 mg. As a result of treating patients with hypertension with differentiated doses of enalapril and indapamide, it was possible to achieve a significant reduction in both systolic and diastolic blood pressure. Moreover, in 70% of patients it was possible to achieve the target blood pressure level, despite its very high initial level. Adverse reactions were noted in only 8.1% of patients, and in 5.4% they were due to an excessive decrease in blood pressure, which can be eliminated with more careful selection of drug dosages.
The main conclusion of the study is that the effectiveness and safety of the combination of enalapril with indapamide in the treatment of hypertension does not depend on gender, age and the cause of the increase in blood pressure (primary hypertension or secondary hypertension of renal origin). Particular attention should be paid to the latter circumstance in connection with the entrenched opinion that the effectiveness of antihypertensive therapy is lower in patients with symptomatic hypertension. The combination of enalapril with indapamide was especially preferred in women in whom ACE inhibitor monotherapy may be less effective.
The results of the EPIGRAF study made it possible to work out the most effective doses of enalapril and indapamide for patients with hypertension of varying degrees, which became the basis for the creation of three types of the drug Enzix: ENZIX - 10 mg of enalapril and 2.5 mg of indapamide (single dose in the morning) for patients with stage I hypertension; ENZIX DUO – 10 mg enalapril and 2.5 mg indapamide (morning) + 10 mg enalapril (evening) for patients with stage II hypertension; ENZIX DUO FORTE – 20 mg enalapril and 2.5 mg indapamide (morning) + 20 mg enalapril (evening).
The effectiveness and safety of Enzix were assessed in the EPIGRAPH-2 study, which was a comparative randomized multicenter study that included nine centers in Russia and one in Serbia [6]. A total of 313 patients were included in the study and randomized into two groups. The Enzix group included 211 patients, and the control group included 102 patients. The control group was treated with other classes of antihypertensive drugs (except ACE inhibitors and diuretics). After 2, 4 and 6 weeks of treatment in cases where it was not possible to achieve target blood pressure (
All patients randomized to the Enzix group were divided into two subgroups depending on the initial blood pressure level.
In the first subgroup, 118 patients with stage I hypertension and initial systolic blood pressure of 140–160 mm Hg. Art. a combination of 10 mg enalapril and 2.5 mg indapamide (corresponding to the ENZIX form) was prescribed. During treatment, 88 (74.6%) of them continued to take the original dose, and in 26 (22.1%) patients the dose of enalapril was doubled (10 mg in the morning + 10 mg in the evening) while maintaining the dose of indapamide (2.5 mg in the morning ), which corresponded to the ENZIX DUO form. Only one patient with stage I hypertension required a combination of 40 mg of enalapril (20 mg in the morning + 20 mg in the evening) and 2.5 mg of indapamide, which corresponded to the ENZIX DUO FORTE form. Three patients did not complete the study.
In the second subgroup, 93 patients with stage II hypertension and systolic blood pressure 160–180 mm Hg. Art. Therapy began with 20 mg of enalapril (10 mg each morning and evening) and 2.5 mg of indapamide (corresponding to the ENZIX DUO form). During treatment in 46 patients, this dosage was maintained, and in 45 patients, the dose of enalapril was increased to 40 mg/day (20 mg in the morning + 20 mg in the evening) with a constant dose of indapamide 2.5 mg, which corresponded to the form of ENZIX DUO FORTE. For two more patients, the initial dose of enalapril was reduced to 10 mg while maintaining the original dose of 2.5 mg of indapamide, which corresponded to the ENZICS form.
When analyzing the number of patients whose blood pressure levels normalized as a result of treatment, the group of patients receiving Enzix (72.5%) had some advantages compared to the control group (66.7%). And this, despite the fact that systolic blood pressure in the “experimental” group was initially 2.7 mm Hg. Art. higher than in the control. If we sum up the total number of patients who responded positively to treatment (the number of patients with normalization of blood pressure or a decrease in systolic blood pressure by more than 20 mm Hg from the initial level), then by the end of treatment it reached 82.4% on average for the group, taking Enzix, and among patients with stage I hypertension this value was 89.8%, and in patients with stage II hypertension – 77.2%.
Thus, early treatment of patients with grades I–II hypertension with a non-fixed combination of enalapril and indapamide (Enzix) in comparison with routine antihypertensive therapy makes it possible to achieve normalization of blood pressure levels more often. In addition, the Enzix group was able to significantly reduce the number of patients with left ventricular hypertrophy and proteinuria, improve quality of life, and reduce the number of hospitalizations and additional visits to the doctor. Among other things, Enzix therapy is cost-effective.
Very important importance is currently attached to the metabolic effects of antihypertensive therapy. The essence of the metabolic theory is that a number of antihypertensive drugs, such as diuretics and beta-blockers (especially non-selective ones), tend to worsen the lipid profile and worsen insulin resistance, which can in the long term increase the risk of developing diabetes mellitus and reduce the effectiveness of therapy in preventing the development of cardiovascular disease [7].
Recently completed large-scale studies have confirmed the validity of the metabolic theory. In groups of patients taking diuretics and beta-blockers, the incidence of diabetes was significantly higher than when treated with calcium antagonists, ACE inhibitors and ARBs [8–10]. In this regard, the effectiveness of antihypertensive therapy must be assessed not only from the point of view of achieving target blood pressure, but also from the standpoint of the likelihood of metabolic effects. This fully applies to combination therapy. It is appropriate to emphasize that the components of Enzix do not cause concern in this regard. Enalapril, as studies show, is metabolically neutral, and indapamide occupies a special place among diuretics. At recommended doses (1.5–2.5 mg per day), it not only provides adequate antihypertensive effects, but is also metabolically neutral. It has been proven that indapamide does not cause hypokalemia or changes in carbohydrate [11] and lipid profiles [12]. Particularly compelling evidence for the metabolic indifference of indapamide comes from a meta-analysis of three studies involving a total of 1195 patients. Based on the results of treatment with the retard form of indapamide for 9–12 months, no effect on carbohydrate and lipid profiles, as well as uric acid levels, was detected [13].
In addition to the diuretic effect, indapamide has a vasodilating effect by reducing the sodium content in the arterial wall, regulating the entry of calcium into vascular smooth muscle cells, as well as increasing the synthesis of prostaglandin E2 in the kidneys and prostacyclin in the endothelium [14]. Thus, indapamide, having a more pronounced direct effect on blood vessels compared to other diuretics, affects endothelial function. It has an antioxidant effect, increasing the bioavailability of NO and reducing its destruction [15]. The LIVE study demonstrated the ability of indapamide therapy to cause regression of left ventricular myocardial hypertrophy [16].