Facial swelling is not only a cosmetic defect; if it appears frequently or is accompanied by redness and pain, it is a sign of quite serious health problems that need to be identified and treated.
ALENA PARETSKAYA
Pathophysiologist, immunologist, member of the St. Petersburg Society of Pathophysiologists ANDREY GRACHEV Leading cardiologist of the SM-Clinic holding, MD, academician of the Russian Academy of Medical Sciences
Facial edema is not a separate disease, but only a reflection of an imbalance between retention and excretion of fluid in the body. But what problems in the body can cause the face to swell and how serious is it?
Diuretics: what are they?
Diuretics are medications that speed up the formation of urine and its elimination from the body.
Such drugs are prescribed primarily to combat tissue swelling due to diseases of the cardiovascular system, kidneys and liver, as well as to treat severe pathological conditions that require rapid fluid reduction.
All diuretics differ in the mechanism of their diuretic effect. The pharmacological property of the drugs is their effect on the epithelium of the renal tubules, where urine formation occurs.
In addition, some medications affect certain enzymes and hormonal substances that are responsible for normal kidney function.
How to relieve leg swelling caused by heat
The best medicine in this case is gravity. Arriving home and throwing away the shoes that have become a vice, it is enough to lie down and place your feet higher (at a minimum - on several pillows, at a maximum - against the wall).
When it becomes easier to move, you need to take a shower. Ideally, a contrasting one that trains blood vessels, but you can limit yourself to just cool. In this case, you should direct the pressure to the feet: such a hydromassage will restore blood circulation.
You can disperse the fluid with light exercises: pulling the toe towards you and away from you, rotating your feet, squatting. But if you don’t have the strength to do this, and your legs hurt, it’s better not to torture them.
Foot baths are also useful. Even plain water will provide relief, but you can enhance the effects with additives. This could be sea salt or herbal infusions. Compresses made from cabbage leaves or bandages soaked in a decoction of birch leaves improve the condition of the limbs.
Indications for diuretics
The main indications for taking diuretics are the following conditions:
- Elimination of swelling of cells and tissues as a result of varying degrees of heart failure and vascular diseases.
- Kidney pathologies.
- Normalization of high blood pressure.
- Removal of toxic and other harmful substances from the body due to poisoning.
- Ascites.
- Liver cirrhosis.
- Glaucoma.
- Osteoporosis.
Edema is the main symptom of pathological conditions of the heart, blood vessels and dysfunction of the excretory system. Fluid accumulation is associated with retention of high amounts of sodium. The mechanism of action of diuretics is precisely that it removes sodium from the body, thereby eliminating swelling.
At high blood pressure levels, increased sodium content negatively affects the tone of blood vessels, leading to their narrowing. Therefore, taking diuretics removes this element from the body, increasing the lumen of blood vessels and normalizing blood pressure.
Due to poisoning, a certain amount of toxins and harmful compounds is reduced during kidney function. However, in order to speed up their elimination, patients are necessarily prescribed diuretics. First, patients are given an intravenous infusion of medicinal solutions, and then diuretics are administered, which, together with the liquid, eliminate toxic substances from the body.
University
→ Home → University → University in the media → Algorithm for the use of diuretics in outpatient practice
To date, few studies have examined the effect of diuretic therapy on the prognosis of patients with fluid retention syndrome (FRS).
When prescribing diuretics, specialists rely primarily on their own clinical experience. It is known that the use of diuretics in those with signs of fluid retention is fraught with side effects (dehydration, hypokalemia, cardiac arrhythmias). It is especially difficult for doctors in outpatient practice to control the results of treatment: they are forced to delegate a significant part of the responsibility for taking medications to patients and their relatives.
The proposed algorithm for prescribing diuretic therapy for CVD was created on the basis of research, recommendations, and clinical experience and is intended to optimize the management of this complex category of patients in an outpatient setting.
Basic rules for prescribing diuretics for CVD Diuretic therapy should begin only if there are symptoms and signs of fluid retention, which include:
• appearance or worsening of inspiratory shortness of breath, tachypnea (RR >16 per minute);
• paroxysmal nocturnal suffocation;
• paroxysmal night cough (in the absence of COPD);
• need to raise the head of the bed to sleep (possibly orthopnea);
• appearance of peripheral edema;
• accumulation of fluid in cavities (ascites, hydrothorax, hydropericardium);
• weight gain by 2 kg in 1 week;
• swelling and pulsation of the neck veins (venous pulse);
• moist rales in the lungs;
• increase in the direct size of the liver;
• X-ray signs of stagnation in the pulmonary circulation (venous hypertension);
• increased left ventricular filling pressure.
If the listed signs and symptoms develop within 1–3 days and are accompanied by tachycardia and hypotension, then such a condition should be regarded as acute decompensation of cardiac activity.
In this case, the proposed algorithm is not applicable and, as a rule, rational management of the patient in an outpatient setting is not possible.
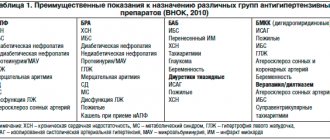
If HF appears as a result of chronic heart failure, then diuretics should be prescribed in combination with ACE inhibitor therapy (if they are intolerant to angiotensin II receptor antagonists, beta-blockers and mineralocorticoid receptor antagonists (MCRA)).
Diuretics for CVS should be used continuously, diuretic therapy should be carried out daily. Intermittent courses of diuretics provoke hyperactivation of neurohormonal systems and may contribute to the progression of CVD.
Weighing yourself daily is important. The maximum permissible weight loss is 1 kg/day, in an outpatient setting - no more than 0.5 kg/day. Dehydration and excessive diuresis are more dangerous than the edema syndrome itself.
Prescribing and titrating the dose of diuretics to increase requires mandatory monitoring of the level of blood electrolytes, glomerular filtration rate (GFR), and the duration of the QT interval at least once a week. Once the condition has stabilized, potassium and creatinine/GFR levels can be determined once every 3–6 months.
When a clinical effect is achieved (reduction in the manifestations of life-threatening symptoms, increase in tolerance to physical activity), it is necessary to begin titrating the dose of the diuretic “downward” with daily weight monitoring. If the patient's condition stabilizes, it is even possible to discontinue the diuretic (the patient should be monitored regularly). When prescribing active diuretic therapy, it is important to remember the peculiarities of the water-salt regime. Optimal diuresis is achieved if treatment is carried out on a diet with the usual amount of sodium with a slight decrease in the volume of fluid drunk (1–1.2 l/day). That is, it is advisable not to sharply reduce salt intake, but only to limit liquids.
Algorithm for prescribing diuretics
If RLS leads to a slight limitation of the patient’s physical activity, which corresponds to class II CHF, in order to make a decision on the choice of diuretics, it is necessary to evaluate renal function and the basic therapy taken (Fig.).
It is preferable to begin diuretic therapy with starting doses of loop diuretics (LDs). Thiazide diuretics (TD), if previously prescribed, can be continued if HF develops in patients with arterial hypertension (AH) and preserved renal function. TDs are safe only in combination with ACE inhibitors or ARBs. Particular attention is paid to the dose. For the treatment of CHF, doses of hydrochlorothiazide (HCTZ) of 25 mg and higher are recommended. In this range, it can lead to severe metabolic disorders, in particular hypokalemia, hyponatremia, and the emergence of new cases of diabetes mellitus. A dose of hydrochlorothiazide of 12.5 mg/day, which is usually prescribed in combination with ACE inhibitors/ARBs as an antihypertensive agent, has a weak diuretic effect.
Achieving positive diuresis using TD is associated with a higher likelihood of hypotension than using PD. A decrease in blood pressure is an independent factor of negative prognosis in patients with CHF, the main cause of HF.
It should be especially noted that even with moderate chronic kidney disease (CKD), the effectiveness of TDs decreases, and a decrease in GFR of less than 30 ml/min/1.73 m2 is an absolute contraindication to their use.
All of the above significantly narrows the role of TD in modern treatment regimens for gastrointestinal tract diseases. They can be included in combination diuretic therapy if large doses of PD are ineffective.
If a clinically significant HF is detected, it is possible to continue taking TDs if they were prescribed as part of combination antihypertensive therapy in a patient with hypertension while maintaining SBP > 140 mm Hg. Art. and GFR > 60 ml/min/1.73 m2. However, in this situation, to eliminate signs of fluid retention, it is necessary to add PD in starting doses. GFR is calculated using the MDRD formula. GFR = 186 (creatinine (in µmol/l) / 88) – 1.154 (age (in years) – 0.203) (for women the result is multiplied by 0.742). Calculation of endogenous creatinine clearance (CC) can be carried out using the Cockcroft–Gault formula: CC = (140 – age) weight (in kg) / creatinine 1.22 (for men); CC = (140 – age) weight / creatinine 1.03 (for women).
TD therapy requires daily monitoring of electrolytes in the first stages due to the high risk of hypokalemia, which is difficult to organize in an outpatient setting.
If the patient has significant limitations in physical activity or the clinical picture of the life-saving lifestyle manifests itself at rest (FC III–IV), then it is necessary to begin diuretic therapy with starting doses of PD (Table).
Advantage should be given to PDs with a long half-life and predictable absorption from the gastrointestinal tract. Extending the release interval of diuretic drug molecules, achieved through the use of a special matrix, reduces the peak concentration of the drug in the blood and increases the time of maximum drug concentration. In this regard, when using such drugs (sustained-release torasemide), a milder and more predictable diuretic effect develops, which worsens the quality of life to a lesser extent. In addition, sustained-release torasemide reduces the patient's risk of developing peak natriuresis, which can lead to renal tubular damage, as well as compensatory activation of the SAS and RAAS, which reduces the result of diuretic therapy.
If the starting doses of PD are ineffective, they should be doubled, but the maximum allowable doses cannot be exceeded. If furosemide is chosen as the starting drug, it is preferable to switch to torsemide due to higher bioavailability in patients with edema syndrome (the dose ratio of torasemide to furosemide is approximately 1:4). If high doses of PD do not lead to relief of the manifestations of CVD, it is recommended to add a carbonic anhydrase inhibitor - acetazolamide. This drug, in addition to its diuretic effect, has the ability to change the pH of urine to the acidic side and can lead to the restoration of sensitivity to PD. The following regimen is usually followed: acetazolamide 250 mg 2-3 times a day for 3-4 days (once every 2-3 weeks). If therapy has not led to a significant improvement in the patient’s condition and he remains limited in physical activity at the level of FC II–IV, it is necessary to prescribe or increase doses of AMCR up to the maximum.
• Increasing doses of AMKR for life-saving lifestyle is allowed up to 200 mg/day for veroshpiron. The dose of the drug should be divided into 2 doses: in the morning and at lunch.
• Increasing AMKR doses is allowed only in situations where CKD is not more severe than stage 3 and potassium levels are normal or low.
• Laboratory monitoring of potassium and creatinine (GFR) is strictly required. When the potassium level is more than 5.0–5.5 mmol/l, the AMKR dose is halved. If GFR decreases < 10 ml/min/1.73 m2, discontinuation of AMCR is required.
• If the potassium level differs more significantly from the norm—more than 5.5 mmol/l—the dose is adjusted until the drug is discontinued, and a low-potassium diet is prescribed.
• After reducing the dose by 50%, a repeated increase in the AMKR dose is possible after 1 month, provided that normokalemia is persistent.
• If the condition is stable and there are no fluctuations in creatinine levels, potassium levels should be monitored once every 3 months.
• It must be remembered that the combination of an ACE inhibitor and a MAKR should always be considered as potentially leading to hyperkalemia. The ineffectiveness of all of these measures requires an assessment of the possible causes of refractoriness to diuretic therapy. The causes of edematous syndrome refractory to combined diuretic therapy may be:
• slowing down the absorption of diuretics (mainly furosemide) in the gastrointestinal tract in patients with ascites and anasarca;
• uncontrolled polydipsia;
• uncontrolled intake of NaCl;
• severe hypotension;
• current NSAID therapy;
• progression of renal failure;
• hypoalbuminemia.
The next stage of treatment for SGI should include intravenous bolus or drip administration of diuretics (furosemide), and, if necessary, a combination of PD and HCTZ.
It is likely that in this situation low systemic blood pressure comes to the fore. In this case, it is important not to further increase diuretic therapy, but to increase plasma flow through the kidney, which is achieved by introducing pressor amines.
There is also a high probability of need for non-drug methods of combating CVD - hemodialysis, ultrafiltration, etc. At this stage, it is unrealistic to continue outpatient management of the patient; the tactics of his further treatment are beyond the scope of this algorithm.
Obviously, the presented algorithm does not consider all possible clinical situations. It does not replace the need for an individual approach, taking into account the underlying and concomitant diseases, the patient’s living conditions and the experience of the attending physician. However, it indicates the main directions for finding rational solutions in the management of patients with fluid retention syndrome in outpatient practice.
Alexander Bova , doctor of medicine. Sciences, Professor, Honored Doctor of the Republic of Belarus,
Sergey Tregubov , assistant at the Department of Military Field Therapy, BSMU Medical Bulletin , August 6, 2014
Share
Contraindications of drugs
The use of diuretics is not always advisable. There are certain conditions that prohibit the use of this type of medicine. These include:
- Low potassium levels in the blood.
- Individual intolerance to sulfonamide substances.
- Severe form of respiratory failure.
- Acute kidney diseases.
- Any type of diabetes.
An implicit contraindication to taking diuretics is ventricular arrhythmia. This clinical condition requires adjustment of the therapeutic dose and strict medical supervision.
Diagnostic methods
To correctly understand the reason for the appearance of such symptoms, it is necessary to carry out a number of diagnostic procedures, including:
- general blood test (extended form);
- blood test for coagulation (prothrombin, fibrinogen, INR);
- blood test to determine hormone levels;
- ultrasound duplex scanning of vessels (arteries and veins) of the lower extremities;
- ultrasound examination of the abdominal organs, retroperitoneal space and pelvis;
- electrocardiography;
- X-ray of the chest organs.
But first of all, the examination must begin with a visit to a doctor - phlebologist and angiologist.
Diuretic tablets for edema
To combat swelling, the most effective drugs are:
- Lasix is a loop diuretic that prevents sodium and chlorine retention.
- Britomar is available in the form of tablets for oral administration. Has long-term therapeutic activity.
- Diuver is a loop diuretic medicine. Often prescribed for heart failure and severe edema.
All medications have contraindications, so they must be taken as prescribed by a specialist.
Why does the face swell in adults?
Swelling on the face can occur at different times of the day - mainly in the morning or late afternoon, or they persist throughout the day, decreasing or increasing.
There are two types of reasons:
- physiological (or natural, not associated with diseases), they are usually not pronounced, not very strong, and disappear quickly;
- pathological, can be very strong, with changes in facial features, signs of inflammation, and are often quite persistent.
Each type of edema has the most typical causes; they occur mainly in the morning or evening hours, or do not depend in any way on the time of day. These characteristics are important for the doctor so that he can identify the leading causes and determine the tactics of examination and treatment.
Diuretic pills for weight loss
Taking diuretics has a positive effect on weight loss. This is due to a decrease in excess fluid in the body, acceleration of metabolism and a decrease in appetite. However, you should take medications carefully to avoid side effects. Therefore, you should consult your doctor first.
List of effective diuretics for weight loss:
- Furosemide.
- Hypothiazide.
- Veroshpiron.
- Phytonephrol.
- Phytolysin.