Medicinal and herbal diuretics.
Thursday, September 23
5155
4.7
1
Content
- How to choose a diuretic
- What are the types of diuretics?
- Classes of diuretics and indications for their use
- The best diuretics
- Hydrochlorothiazide
- Furosemide
- Indapamide
- Veroshpiron
- Torasemide
- Triampur compositum
- Diuver
- Dog-rose fruit
- Diuretic collection
- Juniper fruits
The doctor prescribes diuretics for various edema, hypertension, for the prevention of kidney stones, etc. It is no secret that some women even try to lose weight with the help of diuretics, but this is dangerous to health. The fact is that diuretics, together with liquid, remove potassium from the body - muscle contraction (including the heart muscle) is disrupted. That is why such drugs should be prescribed exclusively by a doctor, taking into account the underlying disease, possible contraindications and side effects.
Read also How to treat dehydration: 5 solutions for rehydration What drugs for dehydration are most often prescribed by doctors?
Contraindications of drugs
The use of diuretics is not always advisable. There are certain conditions that prohibit the use of this type of medicine. These include:
- Low potassium levels in the blood.
- Individual intolerance to sulfonamide substances.
- Severe form of respiratory failure.
- Acute kidney diseases.
- Any type of diabetes.
An implicit contraindication to taking diuretics is ventricular arrhythmia. This clinical condition requires adjustment of the therapeutic dose and strict medical supervision.
How to choose a diuretic
There are specific factors to consider if you choose a diuretic.
- Speed of action.
There are diuretics for emergency use: if you need to quickly lower high blood pressure (used in combination with other drugs), remove morning puffiness under the eyes. You should not take such medications often because they are addictive. Long-acting diuretics are prescribed to treat hypertension and edema associated with poor heart and liver function. - Pregnancy and breastfeeding.
Any diuretic medications are prohibited for pregnant and lactating women. And only in cases where a pregnant or lactating woman has a threat to her health and life, is it possible to use them. Usually this phrase sounds like “the benefit to the mother outweighs the risk to the fetus.” The exception is practically harmless herbal diuretics, but a woman should talk to her doctor before using them. - Tendency to allergies.
People with allergies may experience an undesirable reaction to both the active ingredient of the diuretic drug and its minor components. If you are allergic, consult your doctor before treatment.
In addition to diuretic medications, mild herbal remedies are often used. They are usually prescribed in the complex treatment of cystitis, urethritis, etc. Herbal diuretics not only remove excess water, but also relieve inflammation.
Drinking diuretics for weight loss is dangerous - the heart muscle suffers
Photos from open sources
Diuretics: what are they, why are they prescribed?
The term "diuretics" is quite common. But few people know what they are and how to take them correctly. In simple terms, diuretics or diuretics are medications that remove excess fluid from body tissues. At the same time, cleaning occurs from:
- toxins;
- salts
Attention! When taking diuretics, it is important to understand their mechanism of action. It is quite simple - the components of the drug act on the body in such a way as to enhance the outflow of fluid that is excreted naturally.
As a result, the total blood volume decreases and the load on the body decreases.
Sites of action of diuretics
Diuretics are divided into several categories:
- loop - the most powerful of all diuretics are prescribed for serious diseases, but have a short-lived effect and simultaneously remove potassium;
- thiazides are effective and safe even for newborns, but with regular use and if the dosage is exceeded, they cause potassium removal and an increase in blood sugar levels;
- potassium-sparing - have a long period of action and are successfully combined with other drugs, but in monotherapy the result will be weak;
- carbonic anhydrase inhibitors - prescribed in strictly defined circumstances, as they give a very insignificant effect;
- of plant origin - a practically harmless and gentle diuretic, which is not suitable for serious diseases.
There are many reasons for prescribing diuretics:
- various kidney diseases;
- cardiovascular diseases;
- endocrinological disorders;
- allergy;
- PMS;
- pregnancy;
- individual reaction of the body to elevated environmental temperatures.
Diuretics are usually perceived as a first aid medicine for edema. And they give good results. But uncontrolled use can cause serious harm to the body.
The list of negative consequences includes:
- potassium withdrawal;
- addictive effect;
- water-electrolyte imbalance;
- convulsions;
- decrease in pressure;
- arrhythmia and more.
Therefore, you can start taking it only in consultation with a specialist.
Anti-edema medications are often used for weight loss. And indeed, in a week the drugs can help you lose up to 5 kilograms. But this process has nothing to do with real weight loss. The effect can be achieved by removing fluid from the tissues and it is not always superfluous. Therefore, there is a high risk of getting dehydration, and with it:
- general deterioration of health;
- drying of the skin;
- weakness.
Diuretics for excess weight are indicated in combination with other measures and only in very dosed doses.
Let's look at Diuretics video
What are the types of diuretics?
All diuretic drugs are divided into several categories: according to their spectrum of use and mechanism of action.
- Loop diuretics.
These drugs have the strongest effect (they begin to act literally a few minutes after administration), but the effect ends just as quickly. Such drugs are well suited for the treatment of hypertension and heart failure. But loop diuretics have a significant disadvantage - along with water, they remove potassium from the body, which is fraught with the development of arrhythmia. - Thiazide diuretics.
Another effective diuretic drug. They not only get rid of excess fluid, but also dilate peripheral vessels. Thiazide diuretics also reduce the response of blood vessels to adrenaline, so they spasm less. Such diuretics are also prescribed for the treatment of urolithiasis. Among the “side effects” are the excretion of potassium and an increase in uric acid, which can then accumulate in the joints and cause gout. - Potassium-sparing diuretics.
Such diuretics do not remove potassium from the body, protecting the patient from various heart complications. But these drugs are not as potent as the previous ones. - Osmotic diuretics.
This group of drugs reduces blood plasma pressure - excess water is quickly removed from the tissues, swelling goes away. The pressure in the tissues and in the plasma becomes the same. Typically, osmotic diuretics are prescribed to relieve swelling of the brain, lungs, and high intraocular or intracranial pressure.
The history of the study and practical use of synthetic diuretics goes back just over 50 years. The first thiazide diuretic, hydrochlorothiazide, was synthesized in 1952 and after a relatively short period of time, in 1956, it was introduced into clinical practice. After intensive laboratory research, the loop diuretic furosemide was first used in 1963. The following years were characterized by the active use of diuretics, the accumulation of clinical experience, and the development of new classes of diuretics (osmotic, potassium-sparing). Recent decades in the history of diuretics have been marked by the emergence of drugs with new pharmacological properties (indapamide). Diuretics occupy an important place, first of all, in the treatment of chronic heart failure (CHF), due to their unique pharmacological properties. This circumstance allows us to consider some practical aspects of their use using the example of this nosological form, which represents the final stage of the development of many cardiovascular diseases.
The modern classification of diuretics can be presented as follows [1]:
acting on the glomerulus: - Euphyllin
· acting on the proximal tubule: - osmotic diuretics - Mannitol, Urea, Isosorbitol, Potassium acetate
;
- carbonic anhydrase inhibitors - Acetazolamide
.
· loop: - Furosemide, Ethacrynic acid, Bumetanide, Piretanide, Torsemide
;
· acting on the initial part of the distal tubule: - thiazide sulfonamides - Hydrochlorothiazide, Polythiazide, Cyclopenthiazide, Metolazone
- non-thiazide sulfonamides -
Clopamide, Chlorthalidone, Indapamide, Xipamide
.
· acting on the final part of the distal tubule: - competitive aldosterone antagonists - Spironolactone, Potassium Canreonate
;
- Na transport blockers - Triamterene, Amiloride
.
· herbal diuretics: Bearberry leaf, Birch buds, Lingonberry leaf, Horsetail herb, Juniper fruit, Blue cornflower herb.
· combined diuretics: Triampur, Moduretic.
Diuretics reduce preload and afterload on the heart, eliminate congestion in the internal organs and peripheral edema. The effectiveness of their action depends on which part of the nephron they affect. The most powerful diuretics are furosemide and uregit, as they act throughout the loop of Henle, where the main reabsorption of sodium occurs. The effect of thiazide diuretics, which exert their effect only in the cortical segment of the loop of Henle, is less pronounced. Aldosterone antagonists have weak diuretic activity, but unlike other diuretics, they retain potassium in the body, their effectiveness increases in secondary hyperaldosteronism, and in primary hyperaldosteronism they are the drugs of choice [2].
Diuretics actually used in the treatment of CHF have a number of features. Thiazide and thiazide-like diuretics have a more moderate diuretic and natriuretic effect than loop diuretics; they are ineffective in renal failure; an increase in the diuretic effect with increasing their dose occurs in a very limited range (for hydrochlorothiazide - 25-100 mg).
Loops have a powerful diuretic effect, high efficiency in renal failure, a pronounced dependence of the effect on the dose (furosemide in chronic renal failure is administered up to 2000 mg/day);
Potassium-sparing (relatively weak) drugs are effective for primary and secondary aldosteronism. They can cause hyperkalemia and are often used in combination with other drugs.
The main diuretics used to treat CHF [5] and their proprietary names are presented in Table 1.
Table 1
The main diuretics used to treat CHF and their proprietary names
| A drug | Proprietary names |
| A) Thiazide and thiazide-like diuretics | |
| Hydrochlorothiazide | Hypothiazide, esidrex |
| Indapamide | Indapamide, indap, natrilix, arifon |
| Xipamide | Aquaphor |
| Chlorthalidone | Hygroton, oxodoline |
| Metolazone | Zaroxoline |
| Cyclopenthiazide | Cyclomethiazide |
| B) Loop diuretics | |
| Bumetanide | Bumex, Bufenox |
| Torasemide | Demadex |
| Furosemide | Lasix, furosemide, furesis |
| Ethacrynic acid | Uregit |
| B) Potassium-sparing diuretics | |
| Amiloride | Midamor, modamide |
| Spironolactone | Veroshpiron, spironol |
| Triamterene/div> | Pterofen, daitek |
Diuretics vary significantly in their pharmacological properties and doses used [2, 4]. Summary data for this section is presented in Table 2.
Table 2
Main pharmacological properties of diuretics most often used in the treatment of CHF
| A drug | Bioavailability (%) | T 1/2, (hours) | Main route of elimination | Initial dose per day (mg) | Duration of action (hours) | Therapeutic doses (mg/day) | Frequency of intake per day |
| Thiazide and thiazide-like diuretics | |||||||
| Hydrochlorothiazide | 60 — 80 | 10 — 12 | kidneys | 25 | 12 — 18 | 25-200 | 1 |
| Indapamide | 90 — 100 | 15 — 25 | kidneys + liver(30%) | 1,25 | 12 — 24 | 1,25 — 2,5 | 1-2 |
| Chlorthalidone | 60 — 65 | 24 — 50 | kidneys + liver | 25 | 24 — 72 | 25-100 | 1 |
| Metolazone | 50 — 60 | 8 — 14 | kidneys + liver | 2,5 | 12-36 | 10 | 1 |
| Loop diuretics | |||||||
| Furosemide | 10 — 90 | 0,3 — 3,4 | kidneys + liver(40%) | 10 — 40 | 6 — 8 | 20 — 200 | 2-1 |
| Bumetanide | 60 — 90 | 60 — 90 0,3 — 1,5 | kidneys + liver | 0,5 — 1,0 | 4 — 6 | 10 | 1 |
| Torasemide | 80 — 90 | 0,8 — 6.0 | kidneys + liver | 5-10 | 24 | 10-100 | 1 |
| Potassium-sparing diuretics | |||||||
| Spironolactone | 60 — 90 | 14 | kidneys + liver(20%) | 25 | 8 — 12 | 25-200 | 2 |
| Triamterene | 50 | 3 — 5 | kidneys + liver | 50 | 12 | 150-300 | 2 |
| Amiloride | 50 | 6 — 9 | kidneys + liver(50%) | 5 | 24 | 5-20 | 1 |
The use of diuretics for CHF is usually associated with loop diuretics. Indeed, furosemide is used most often for heart failure.
Furosemide (Lasix)
causes a fast, powerful, but not long-lasting diuretic effect. Has a fairly pronounced withdrawal syndrome. Enhances the excretion of potassium, phosphates, calcium and magnesium without affecting the glomerular filtration rate, increases the excretion of bicarbonates and increases the pH of urine. Can be used for renal failure. Usually the drug is prescribed orally at a dose of 20-240 mg/day. When taken orally, its effect begins after 1 hour and lasts 4-6 hours. When administered intravenously, the effect occurs after 10-15 minutes and lasts 2-3 hours. Standard regimen The use of furosemide for CHF involves taking the drug orally 1-2 times a week. In case of development of renal failure and in the absence of adequate diuresis from therapeutic doses, the last maximum dose is doubled and continues to be doubled every 30-60 minutes until the effect is achieved (sometimes up to 2-3 g per day).
Ethacrynic acid (uregitis)
somewhat less active than furosemide, otherwise the drugs are similar. Prescribed 50-200 mg/day. The onset of action is after 30 minutes, the maximum effect when taken orally occurs after 2 hours and lasts about 4-6 hours. With intravenous administration, the diuretic effect occurs after 15 minutes and lasts 2-3 hours.
Furosemide and ethacrynic acid, administered intravenously, reduce pressure in the pulmonary artery and filling pressure of the left ventricle, cause veno- and arteriodilatation, which is associated with an improvement in myocardial contractility. The drugs affect different parts of sodium reabsorption (furosemide has an additional effect on the proximal tubule), so they can be prescribed simultaneously or replaced with one another when the diuretic effect decreases. The biotransformation of both drugs is impaired in liver cirrhosis.
Side effects of loop diuretics:
hyperchloremic alkalosis, hypokalemia, hyperuricemia, hyperglycemia, potentiation of toxic effects when used together with antibiotics (cephalosporins, aminoglycosides).
Thiazide and thiazide-like diuretics are somewhat less important in the treatment of CHF.
Hydrochlorothiazide
(hypothiazide, dichlothiazide, Nephrix, Ezidrex) are used orally at 25-200 mg/day, maintenance dose 6.25-12.5-50 mg once a day in the morning, 1-3 times a week. The onset of action is after 2 hours, its peak is after 4 hours, the duration of the diuretic effect is about 10-12 hours. It is most advisable to take hydrochlorothiazide for arterial hypertension associated with CHF, since the long-term and moderate hypotensive effect of this drug largely corresponds to the goals of treating hypertensive diseases.
Klopamide
(brinaldix), unlike other thiazide and other thiazide-like diuretics, increases venous tone (indicated for patients with orthostatic reactions). Used in doses of 10-40 mg in the morning, maintenance dose 10-20 mg once a day or every other day. The onset of action is 1-3 hours, its duration is 8-20 hours. The main feature of the drug is a long-term diuretic effect without forced diuresis.
CHF is quite often a consequence of arterial hypertension, which makes combined treatment of patients with ACE inhibitors and diuretics preferable. Indapamide can be considered one of the drugs of choice among diuretics, which reduces the level of intracellular calcium, preserves magnesium content, reduces the rigidity of the vascular wall and promotes more effective relaxation of the cardiomyocyte in diastole. In this case, there is an increase in the synthesis of prostacyclins, a decrease in platelet aggregation and the release of thromboxane A2, which ultimately has a positive hemodynamic effect by reducing the afterload for the left ventricle. Indapamide is expected to have a cardioprotective effect comparable to ACE inhibitors. The effect of the drug on blood pressure without a significant effect on diuresis is manifested in a daily dose of up to 2.5 mg, with an increase in which the diuretic effect becomes dominant. Take indapamide in the morning, the duration of action is up to 24 hours.
Side effects of thiazide diuretics
: atherogenic and diabetogenic effects, hypokalemia, hyperuricemia. It should be noted that these side effects were noted when studying maximum doses of diuretics and with their long-term use, however, clinical observations show that hypokalemia and hyperuricemia can develop with small doses of thiazides, especially in patients with “compromised” metabolism of electrolytes and purines. The great advantage of indapamide is the absence of rebound syndrome and adverse metabolic disorders (negative effects on carbohydrate and lipid metabolism) when using it.
In recent years, potassium-sparing diuretics have occupied a special place in the treatment of CHF.
Triamterene
(pterophen) as a potassium-sparing agent is used at 25-100 mg/day, with further individual dose selection (no more than 300 mg/day in 2 doses). For CHF, drugs combined with hydrochlorothiazide are often used (Triampur, 1-2 tablets per dose, 1-2 times a day). The onset of action is after 2-4 hours, its peak is 6-8 hours, duration is 7-9 hours. Taking triamterene in the elderly is associated with an increased risk of hyperkalemia and hyponatremia.
Spironolactone
(veroshpiron) has a diuretic effect dependent on the level of aldosterone in the blood plasma. The main feature of the drug’s action is considered to be neuro-hormonal modulation of the activated RAAS. For CHF, it is prescribed together with hydrochlorothiazide or furosemide. Spironolactone is prescribed after the diuretic effect of more active thiazide or loop diuretics wanes after 1-2 weeks of therapy. The onset of action is after 24-48 hours, its peak is 2-3 days of administration, duration is 4-6 days. The drug is prescribed at a dose of 50-100 mg/day in 1-2 doses, but not more than 400 mg/day.
The standard recommended dose, which has the effect of maximum neurohormonal modulation, is 25 mg/day. If it is necessary to increase the potassium concentration in patients with CHF against the background of aggressive diuretic therapy, the dose of spirolactone can be increased to 200-400 mg, but only for a short period of time, since increased doses of veroshpiron help reduce antitumor protection.
Eplerenone
(inspra) is a new potassium-sparing diuretic that is being actively studied at the stage of practical use in the clinic.
Side effects of potassium-sparing diuretics:
hyperkalemia, menstrual irregularities, deepening of voice, hirsutism, gynecomastia.
Potassium-sparing diuretics are contraindicated for hyperkalemia (chronic renal failure or a combination of potassium supplements and ACE inhibitors). The latter circumstance in clinical practice seems to be very relative, since in case of persistent and severe hypokalemia associated with repolarization disorders, arrhythmogenesis, the entire available arsenal is used to increase potassium concentration, including, as a rule, potassium-sparing diuretics, ACE inhibitors and potassium preparations directly.
Diuretic therapy tactics
Diuretics are prescribed when the first signs of edema syndrome appear, and the activity of therapy should directly depend on the degree of its severity [3, 4].
Begin treatment with small doses of thiazide or thiazide-like drugs (25 mg hydrochlorothiazide or equivalent doses of others) to avoid large and rapid losses of water and electrolytes. This is due to the rapid emergence of tolerance to diuretics and activation of the renin-angiotensin-aldosterone and sympathoadrenal systems, antidiuretic hormone, which in CHF plays a leading role in maintaining disturbances of central and peripheral hemodynamics.
As necessary, increase the dosage of drugs; instead of thiazide diuretics, loop diuretics are prescribed or 2-3 diuretics with different mechanisms of action are combined. This allows, with an increase in diuresis, to correct unfavorable electrolyte-metabolic changes and reduce the risk of developing resistance to therapy. To avoid excessive loss of potassium during treatment with thiazide or loop diuretics, it is necessary to limit the intake of table salt (up to 5 g/day) and water (up to 1.5 l/day). It is better to combine thiazide or loop diuretics with one of the potassium-sparing drugs - veroshpiron, triamterene. In patients with CHF outside of emergency situations, taking diuretics should cause fluid loss in a volume of no more than 1.0 l/day (decrease in body weight by 1 kg), so as not to cause a sharp decrease in the volume of circulating blood, which, in turn, adversely affects the systemic hemodynamics and neurohumoral regulation.
For stage II CHF, hydrochlorothiazide is prescribed 50 mg 1-2 times a week, if necessary increasing the dose to 100-150 mg. The effectiveness of treatment is assessed by diuresis, which should increase by 1.5-2 times (1.5-2 liters of urine). For severe edematous syndrome, powerful “loop” diuretics are used. Furosemide is administered 40 mg parenterally or orally 2-3 times a week or more often. If the effect is insufficient, the dose can be increased to 160 mg/day or more. The accumulation of fluid in the abdominal or other cavities indicates the presence of secondary hyperaldosteronism; in such cases, it is advisable to combine furosemide with spironolactone (150-200 mg/day).
It should be borne in mind that active diuretic therapy may be complicated by dehydration, hypokalemia (muscle weakness, anorexia, ST segment depression, decreased T wave amplitude), and hyponatremia. Therefore, as the patient's condition improves, diuretics should be used less frequently and in lower doses.
The causes of resistance to the action of diuretics are: dilution hyponatremia, hyperaldosteronism, active inflammatory process, hypoproteinemia, plethora (polycythemia), arterial hypotension, hypoxia. Patients may become refractory to high doses of diuretics if they consume large amounts of dietary sodium, are taking medications that may block the effects of diuretics (eg, NSAIDs, including COX-2 inhibitors), or have a significant deterioration in renal function or perfusion.
Resistance can be avoided (depending on its cause) by administering sodium chloride solutions, using veroshpiron, anti-inflammatory and antibacterial agents, administering albumin and plasma, bloodletting, using cardiac glycosides and glucocorticoids. Resistance to diuretics can often be overcome by intravenous administration (including the use of continuous infusions), use of two or more diuretics in combination (eg, furosemide and metolazone), or use of diuretics with drugs that increase renal blood flow (eg, positive inotropic agents).
To overcome refractoriness to treatment with diuretics, a more expanded set of methods can be used [5]:
1. Strict restriction of salt intake (not liquid!). 2. Prescribing diuretics only intravenously. 3. Use of high doses of diuretics. There are reports of overcoming refractoriness to therapy when prescribing up to 2000 mg of Lasix. In particularly difficult cases, a bolus injection of Lasix intravenously at a dose of 40-80 mg is recommended, followed by drip administration at a rate of 10-40 mg over 48 hours. 4. Creating conditions for normalizing blood pressure:
- refusal to take vasodilators, most often nitrates prescribed without indications, only due to a diagnosis of coronary artery disease;
- if necessary, use of steroid hormones (prednisolone intravenously up to 180-240 mg and orally up to 30 mg), cordiamine;
- in critical situations, intravenous drip infusion of dopamine is used at a “renal” rate of 0.5-2.0 mg/kg/min, lasting up to 24 hours. In this case, the drug, due to its effect on dopaminergic receptors, in isolation increases the renal fraction of blood flow, glomerular filtration and slightly reduces proximal reabsorption. With an increase in the duration of dopamine administration, as well as with an increase in the infusion rate, other effects of the drug begin to predominate (stimulation of beta-1 and then alpha-1 receptors), accompanied by an increase in blood pressure and inotropic effects, which allow maintaining an acceptable level of glomerular filtration.
5. Normalization of the neurohormonal profile (prescription of ACE inhibitors and aldosterone antagonists). Aldactone (veroshpiron) is best prescribed in the morning, during the maximum circadian rise in aldosterone levels at a dose of 200-300 mg/day. It must be remembered that the drug prescribed orally begins to act only on the 3rd day, so in the first 2-3 days it is better to administer the drug intravenously. 6. Normalization of the protein profile - the use of albumin (200-400 ml/day), together with diuretics, which increases the rate of their filtration. 7. At a sufficient level of blood pressure, it is possible to additionally prescribe drugs that increase the glomerular filtration rate (positive inotropic drugs, aminophylline). 8. Combination of several diuretics. We have already talked about the advisability of combining active diuretics with carbonic anhydrase inhibitors, which avoids the development of alkalosis, under which the effect of thiazide and loop diuretics is weakened. Diacarb, firstly, acidifies the urine, and secondly, due to the disruption of sodium reabsorption in the proximal tubules, it maintains a higher concentration of this ion in primary urine. Because of this, the ascending part of the loop of Henle is more “loaded” with sodium ions and the substrate for the action of loop and thiazide diuretics increases.
Similarly, the combined use of loop and thiazide diuretics increases the flow of sodium ions into the distal tubules, where aldosterone antagonists act, and thereby increases the effectiveness of veroshpiron.
This is an important rule: the prescription of any diuretic drug leads to the fact that due to impaired sodium reabsorption, the “loading” of more distal parts of the nephron with this ion increases. As a result, the effect of diuretics aimed at the underlying tubules is potentiated.
The methods of use and dosage regimens of spironolactone can be presented in the form of the following sequence of actions: 1) assess the severity of CHF (spironolactone should be prescribed only for severe CHF); 2) make sure that the potassium content in the blood serum is below 5.0 mmol/l, and creatinine is below 250 mmol/l; 3) first prescribe spironolactone at a dose of 25 mg/day; 4) assess potassium levels after 4-6 days; 5) if the potassium concentration is from 5 to 5.5 mmol/l, the dose should be reduced by 2 times; if potassium levels are above 5.5 mmol/L, spironolactone should be discontinued; 6) if after 1 month of therapy symptoms of HF persist and there is no hypokalemia, it is advisable to increase the dose of spironolactone to 50 mg/day, followed by assessment of the level of potassium in the blood after 1 week.
Controlled studies have demonstrated the ability of diuretics to increase urinary sodium excretion and reduce symptoms of fluid retention in patients with CHF. In these short-term studies, diuretic therapy led to reductions in central venous pressure, pulmonary congestion, peripheral edema, and body weight, all of which were observed in the first days of therapy. In studies with medium follow-up, diuretics improved cardiac function and exercise capacity, and reduced symptoms in patients with CHF. There have been no long-term studies of diuretic therapy in CHF, and thus the effect on morbidity and mortality is unknown.
Optimal use of diuretics is the cornerstone of any successful approach to the treatment of HF. When using diuretics in patients with CHF, physicians should remember the following points [6]:
1. Diuretics provide clinical improvement more quickly than any other drug for the treatment of CHF. They can reduce pulmonary and peripheral edema within hours or days, whereas the clinical effects of cardiac glycosides, ACEIs, or beta blockers may take weeks or months to become apparent.
2. Diuretics are the only drugs used to treat CHF that can adequately correct fluid retention. Although both cardiac glycosides and low-dose ACEIs can increase urinary sodium excretion, few patients with CHF can maintain sodium balance without the use of diuretics. Attempts to replace diuretics with ACE inhibitors can lead to fluid accumulation in the periphery and in the cavities.
3. Diuretics should not be used as monotherapy in the treatment of CHF. Even when diuretics are successful in controlling symptoms and fluid retention, they alone are not able to maintain clinical stability in patients with CHF over the long term. The risk of clinical decompensation may be reduced when diuretics are combined with digoxin, an ACE inhibitor, or a beta blocker.
4. The use of diuretics in adequate doses and appropriate regimens is a key element in the effectiveness of other drugs used to treat CHF. Inappropriate use and inappropriately low doses of diuretics can cause fluid retention, which may reduce response to ACEIs and increase the risk of complications with beta blockers. In contrast, the use of inappropriately high doses of diuretics will lead to a reduction in volume, which may increase the risk of hypotension with ACEIs and vasodilators and the risk of renal failure with ACEIs and angiotensin II receptor antagonists.
Practical use of diuretics
Patient selection.
Diuretics should be prescribed to all patients with symptoms (and most patients with a previous history) of fluid retention. Diuretics should be combined with an ACEI and a beta blocker (and usually digoxin) [7].
Initiation and implementation of therapy.
The most commonly used loop diuretic for the treatment of CHF is furosemide, but some patients respond favorably to newer agents in this category (eg, torsemide) due to their higher bioavailability. Studies have shown that torsemide may reduce the risk of progression of heart failure more effectively than furosemide, but this issue remains controversial.
In outpatients with CHF, therapy usually begins with low doses of diuretics, and the dose is increased until diuresis increases and body weight decreases, on average, by 0.5-1.0 kg daily. Further increases in the dose or frequency of diuretics may be necessary to maintain active diuresis and weight loss. The ultimate goal of treatment is to eliminate symptoms of fluid retention, either by restoring central venous pressure to normal, eliminating the presence of edema, or a combination of these mechanisms.
Diuretics are usually combined with moderate dietary sodium restriction (less than 3 g daily). If signs of electrolyte imbalance appear, they must be persistently combated and diuretic therapy must be continued. If hypotension or azotemia occurs before treatment goals are achieved, the clinician may elect to reduce diuretic doses, but diuresis should still be maintained until fluid retention is corrected, even if this strategy will result in a modest decrease in blood pressure or renal function as long as the patient remains asymptomatic. Excessive concern about hypotension and azotemia may lead to underprescription of diuretics and the development of resistant edema.
Chronic volume overload not only contributes to the persistence of symptoms, but may also limit the effectiveness and compromise the safety of other drugs used to treat HF.
Once fluid retention has resolved, diuretic treatment should be continued to prevent recurrence of volume overload. Patients are usually prescribed a fixed dose of a diuretic, but the dosage of these medications must be adjusted periodically. In many cases, this adjustment can be made by measuring the patient's body weight daily and providing recommendations for dosage adjustments as body weight increases or decreases beyond certain limits.
The response to a diuretic depends on the concentration of the drug and the time it is eliminated in the urine. Patients with moderate CHF respond favorably to low doses because absorption occurs quickly in the intestine and these drugs quickly reach the renal tubules. However, in advanced CHF, drug absorption may be reduced due to intestinal edema or insufficient intestinal perfusion, and drug delivery may be reduced due to chronically decreased renal perfusion. Consequently, clinical progression of CHF is characterized by the need to increase doses of diuretics.
Dangers of diuretic treatment.
The major adverse effects of diuretics include electrolyte imbalance, hypotension, and azotemia. Diuretics can also cause hearing impairment, but this is usually limited to individual intolerance or occurs when very high doses of the drug are prescribed. Diuretics can cause loss of important cations (potassium and magnesium), which may predispose patients to serious arrhythmias, especially when treated with cardiac glycosides [7, 8]. The risk of electrolyte depletion increases markedly when two diuretics are used in combination. The loss of electrolytes is associated with increased delivery of sodium to the distal renal tubules and the exchange of sodium for other cations, a process that is potentiated by activation of the renin-angiotensin-aldosterone system. Potassium deficiency can be corrected by short-term administration of potassium and, in severe cases, additional administration of magnesium. Concomitant administration of ACE inhibitors or their combination with potassium-sparing agents can prevent electrolyte depletion in most patients taking loop diuretics. When these drugs are prescribed, long-term oral potassium intake is unnecessary and may even be harmful.
Excessive use of diuretics can decrease blood pressure, impair kidney function and exercise capacity. Hypotension and azotemia may also occur as a result of progression of CHF, which may be exacerbated by attempts to reduce the dose of diuretics. If there are no signs of fluid retention, hypotension and azotemia are likely due to a decrease in blood volume and may resolve after reducing the diuretic dose. If symptoms of fluid retention are present, hypotension and azotemia appear to reflect progressive CHF and decreased effective peripheral perfusion. Such patients should be treated with maintenance doses of diuretics and improvement of end-organ perfusion.
The criteria for the positive effect of diuretics in CHF are:
: improvement in the clinical condition of patients (reduction of edema, loss of body weight, shortness of breath, increase in exercise tolerance, etc.), persistent decrease in ventricular filling pressure at rest and during exercise, reduction in the frequency of sudden death, development of acute vascular accidents, increase in duration life.
Thus, the presented analysis, based on the available literature data and practical experience in the use of diuretics, reflects the main clinical aspects of the use of diuretics in chronic heart failure. The authors of the material hope that the background, theoretical and practical information provided in the article will help doctors optimize the prescription of diuretics to patients with CHF.
Literature.
1. Bobrov L.L., Gaivoronskaya V.V., Shcherbak Yu.A., Kulikov A.N., Obrezan A.G., Filippov A.E. Clinical pharmacology and pharmacotherapy of internal diseases (methodological manual), - St. Petersburg. - 2000 - 365 p.
2. Kushakovsky M.S. Chronic congestive heart failure. Idiopathic cardiomyopathies. St. Petersburg: Foliot, 1998. - 320 p.
3. Mareev V.Yu. Diuretics in the treatment of heart failure // Heart failure. - 2001. - T.2, No. 1. — P.11-20.
4. Mareev V.Yu. Recommendations for the rational treatment of patients with heart failure // Consilium medicum. - 1999. - T.1, No. 3. — P.109-147.
5. Obrezan A.G., Vologdina I.V. Chronic heart failure. — St. Petersburg: “Vita Nova.” - 2002. - 320 p.
6. Recommendations for the diagnosis and treatment of chronic heart failure // Heart failure. - 2001. - T.2, No. 6. — P.251-276.
7. ACC/AHA/ Guidelines for the Management of Patients With Chronic Heart Failure //
8. Braunwald E.. Heart disease: a textbook of cardiovascular medicine / Ed. E.Braunwald. — 4th ed. - Philadelphia.: Sounders. - 1992. - 1874, Xl.IV p.
Start
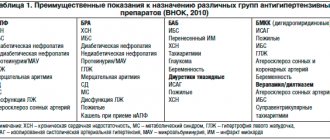
Classes of diuretics and indications for their use
Main indications for the use of diuretics of various classes
| Diuretic class | Indications |
| Osmotic | Edema of the brain, lungs, acute attack of glaucoma, barbiturate poisoning |
| Carbonic anhydrase inhibitors | Edema due to pulmonary heart failure, glaucoma, epilepsy |
| Loop | Hypertensive crisis, cerebral edema, chronic renal failure, poisoning with water-soluble poisons |
| Thiazides and thiazide-like diuretics | Hypertension, cardiovascular failure, liver cirrhosis, nephrosis, pregnancy nephropathy, glaucoma |
| Potassium-sparing | Hypertension, heart failure, liver cirrhosis, hypokalemia during treatment with diuretics of other groups |
| Vegetable | Renal edema, whistitis, chronic renal failure |
| Xanthine derivatives | Hypertension, heart failure (in complex therapy) |
Hydrochlorothiazide
One of the most effective means for removing excess fluid and sodium salts from the body. Hydrochlorothiazide is prescribed for diseases of the kidneys, heart, lungs, to reduce blood pressure and reduce swelling. The drug does not form metabolites and is excreted unchanged by the kidneys. The maximum effect of the diuretic is achieved 4 hours after administration, and it lasts for 12 hours. Patients about it has a pronounced diuretic effect, any swelling quickly goes away, it is inexpensive. Among the disadvantages is a large list of “side effects” and the removal of important microelements from the body (including potassium and magnesium).
Hydrochlorothiazide
OZON, Russia; Pranapharm LLC, Russia; PJSC "Biokhimik", Russia; OJSC Borisov Plant of Medical Preparations (Borimed), Belarus; PJSC Valenta Pharm, Russia
A diuretic drug that is used for: Arterial hypertension, edema syndrome of various origins (chronic heart failure, nephrotic syndrome, renal failure, fluid retention in obesity), diabetes insipidus, glaucoma (subcompensated forms).
from 34
5.0 1 review
546
- Like
- Write a review
Distinguishing the cause of edema
Of course, this material is not addressed to doctors, but a specialist should understand the causes of edema. But the modern Russian healthcare system is designed in such a way that it is extremely difficult to immediately get free access to a specialist; you must first visit a therapist as a “divorce”. Therefore, many turn to a paid doctor, and the main thing is to choose exactly who to turn to for edema: a cardiologist, a vascular surgeon who deals with the problems of varicose veins, or, for example, a nephrologist.
In order to figure this out right away and not spend extra money, we can tell you general but important information about edema:
- You should visit a cardiologist if swelling occurs in the legs; it is symmetrical and painless, intensifies in the evening, and leaves a pit of doughy consistency after pressing. Additional symptoms include shortness of breath; the patient often has long-term chronic heart damage, for example, valvular defects, previous myocardial infarction or arrhythmia;
- if swelling also occurs in the legs, but together with a feeling of heaviness in the calves, aching pain, night cramps, and appears after prolonged standing or long walking, and decreases overnight, then this is due to varicose veins of the lower extremities . This is especially true if, after a long period of such edema, spider veins, peeling of the skin, or the phenomenon of varicose dermatitis occur. We need a phlebologist or vascular surgeon;
- if in this case the swelling of the leg is asymmetrical, on the one hand, the leg is hotter than the other, then, most likely, we are talking about thrombosis of the venous vessels, and here you need to contact a vascular surgeon;
- if the patient has a long-term chronic pathology of the kidneys, swelling appears on the face, on the eyelids, does not change its location depending on changes in the state of the body in space, is not accompanied by shortness of breath, and in matcha tests a high protein is determined, more than 3 g per day, then speech It's about nephrotic syndrome. If the patient has high blood pressure and a small amount of urine, then it is necessary to urgently visit a nephrologist or kidney disease specialists;
- if a person had jaundice, active hepatitis, cirrhosis was diagnosed, the amount of protein in the blood plasma was reduced, the level of bilirubin and transaminases was high, and his stomach swells like a drum, his navel protrudes, then everything is clear. We are talking about the development of ascites, or the accumulation of fluid in the abdominal cavity and portal hypertension, and here it is necessary to visit either a hepatologist for liver diseases, or an infectious disease specialist in the case of chronic viral hepatitis, or a surgeon.
Finally, if lymphatic edema associated with lymphostasis occurs, then at first the edema may be asymmetrical, on the one hand. But even if they become double-sided, they may also not be the same. At first these are soft swellings, like dough, they can intensify in hot weather, the skin over them easily moves. If they exist for a long time, then the skin over them thickens and becomes denser, the hole no longer remains, and in the later stages complete tissue fibrosis develops. The skin becomes lumpy and separated by deep folds. This happens when lymph nodes and lymphatic vessels are compressed, and in our country this most often occurs in advanced forms of cancer pathology. An urgent consultation is needed, first of all, with an oncologist.
Treatment of edema should always be comprehensive, and treatment should begin with attempts to eliminate the cause. So, if the cause is chronic heart failure, then it is necessary to enhance the work of the heart, for example, by using cardiac glycosides. In the presence of glomerulonephritis, it is necessary to use hormones and cytostatics; in the presence of hypothyroidism and myxedema, thyroid hormones must be prescribed, and so on.
However, in addition to etiotropic treatment aimed at the direct cause of edema, it is necessary to limit the intake of fluid, and for generalized edema it is necessary to limit salt intake, and one of the most important methods of pathogenetic treatment of edema syndrome is the prescription of modern diuretics, or diuretics. How are diuretics used, and what are diuretics? What caution should patients and physicians take when using them?
Furosemide
This diuretic is one of the most popular and frequently prescribed, and is a strong diuretic. Furosemide removes excess water and sodium salts from the body well and quickly, and relieves swelling. The drug is indicated for hypertension, poor functioning of the heart, kidneys and liver. Diuretic tablets begin to act 20-30 minutes after administration. Furosemide is usually used in emergency cases. You cannot take the drug without medical supervision, because self-medication can lead to dehydration. Furosemide is inexpensive, acts quickly, but has many side effects, including the removal of potassium and magnesium.
Furosemide
Sopharma, Bulgaria; PJSC "Biosintez", Russia; Binnopharm, Russia; JSC Avexima, Russia; Update, Russia; JSC Pharmstandard-TomskKhimPharm, Russia; "Moskhimfarmpreparaty" named after. N. A. Semashko, Russia; Ozon LLC, Russia; OJSC Borisov Plant of Medical Preparations (Borimed), Belarus; JSC Dalkhimfarm, Russia
Edema syndrome of various origins (with chronic heart failure, cirrhosis of the liver (portal hypertension syndrome); edematous syndrome of renal origin (with nephrotic syndrome, treatment of the underlying disease is in the foreground), acute heart failure, especially with pulmonary edema (used in combination with other therapeutic agents) measures); cerebral edema; severe forms of arterial hypertension; hypertensive crisis; forced diuresis in case of poisoning with chemical compounds excreted unchanged by the kidneys.
from 17
2.0 1 review
924
- Like
- Write a review
Modern diuretics
Let us remind you once again that this material is intended, for the most part, not for patients suffering from edema syndrome, who are observed by a cardiologist for heart failure, and routinely take diuretics. Still, they are under the supervision of doctors and have a significantly lower risk of uncontrolled use of diuretics. This material is intended for those people who for some reason decided to use diuretics at their own risk.
It is no secret, for example, that the use of 1-2 tablets of furosemide in combination with intensive drinking of mineral water, vitamin C, and taking a hot shower can quickly eliminate a hangover and get a person in shape. Yes, forced diuresis is one of the effective means of removing the human body from a state of alcohol intoxication, and even from binge drinking.
But at the same time, it is necessary to remember the disadvantages that even the best modern diuretics have. Thus, treatment with these drugs alone, without correction of the ionic composition of the plasma, can lead to a large loss of fluid and mineral salts from the vascular bed, and this output will be greater than from the intercellular space. This can lead to a decrease in the amount of liquid part of the blood, or plasma, a decrease in the pumping function of the myocardium and a sharp drop in blood pressure, which can manifest as collapse. If the patient also has symptoms of heart failure, this will cause a reduced return of venous blood to the heart, and will further aggravate the low cardiac output.
Always, when using this or that diuretic, you need to find out about its capabilities, how powerful it is. Thus, thiazide diuretics, which act on the renal tubules and reduce carbonic anhydrase activity, are very common, and the most powerful are loop diuretics. Potassium-sparing diuretics can be considered quite mild and relatively harmless, since they have a rather weak effect.
Diuretics from the osmotic group, for example, Mannitol, will not be listed below. The scope of their application is completely different, for example, Mannitol is widely used in neuroreanimation and neurosurgery for the prevention and treatment of cerebral edema after surgery and in cases of severe traumatic brain injury. This section will not talk about those drugs for edema that reduce the symptoms of chronic venous insufficiency and are used in the treatment of varicose veins. These include various plant bioflavonoids, horse chestnut, rutin preparations, diosmin and others. They will be discussed in the relevant materials devoted to the treatment of varicose veins; their area of application is completely different, and they are not diuretics.
We will look at diuretics that have a common mechanism of action and affect the kidneys. There are not many of these drugs, and there are not many commercial copies or generics of them. But in any case, the international nonproprietary name (INN) will be given first, then, if available, the original drug, which was first introduced to the market and has the largest number of studies on effectiveness and safety, will be named first. The various generics, or commercial copies, will then be named, followed by the price. Prices are valid for the beginning of spring 2021 for pharmacies of all forms of ownership in the Russian Federation.
The following list of medicines does not aim to create advertising or anti-advertising for any manufacturer or drug; all these medicines are included in the State Pharmacopoeia and are used in accordance with national and clinical recommendations for the management of patients with edematous syndrome. Some of the medications that cannot be found in pharmacies will not be listed here, as well as older, obsolete, rather toxic mercury diuretics.
Indapamide
This is a moderate-acting drug that is usually prescribed for edema associated with heart failure. "Indapamide" is quickly absorbed into the gastrointestinal tract. Diuretic tablets reduce the load on the heart and peripheral vessels and stabilize blood pressure. The effect occurs an hour after taking the drug and lasts 12-18 hours. You can buy Indapamide with a prescription, it is inexpensive, but it is a generic (not the original drug). Be sure to check the possible side effects.
Indapamide
OZON, Russia
Arterial hypertension;
sodium and water retention in chronic heart failure. from 8
771
- Like
- Write a review
Side effects
The list of such is numerous. But in reality, not everything is so dangerous. Negative phenomena are relatively rare.
- Nausea, vomiting, abdominal discomfort, heartburn, belching. Indigestion. Manifestations of dyspepsia. Diarrhea, constipation.
- Headache, weakness, drowsiness.
- Allergy.
- Dandruff formation, temporary baldness (hair loss).
- Spasms of the calf muscles. Relatively often. Especially against the background of an inadequately low dosage when taking loop or thiazide drugs in parallel.
- Dizziness. Inability to properly navigate in space.
- Acute renal failure with a critical drop in the amount of daily urine, up to its complete absence (anuria).
Changes in urine and blood are also observed, which must be taken into account when conducting tests.
Veroshpiron
This is a potassium-sparing diuretic, which is prescribed for edema due to chronic heart failure and hormonal problems. And although Veroshpiron has a weak diuretic effect, the drug does not remove potassium and does not upset the acid-base balance in the body. The maximum effect of the diuretic occurs after 2-3 days and lasts a long time. You can buy Veroshpiron with a prescription; it is important to take into account the impressive list of contraindications.
Veroshpiron
Gedeon Richter, Hungary
The drug Veroshpiron is a potassium-sparing diuretic.
from 72
762
- Like
- Write a review
Read also Diet pills: effective drugs for weight loss List of the most effective weight loss pills.
The importance of the element potassium in the functioning of the body
Most of the potassium is found in the cells that make up any organism. A small amount of it is found in the intercellular fluid. In the intercellular space, it is responsible for the passage of nerve impulses, monitors muscle contraction, including the heart muscle, and maintains blood pressure levels. Intracellular potassium regulates acid-base and water balance, participates in the work of nerve cells in the brain, and interacts with enzymes. If the balance of this element is not restored after taking diuretics, its deficiency can lead the body to neurosis, cause serious heart problems, and cause a stroke.
Natural losses of potassium in the body occur when stomach acid is released during the digestion of food. Some potassium is lost during intense sweating in the heat or during physical activity. Part is excreted through the kidneys. The largest amount of the element can be washed out when you start taking some diuretics. There are drugs that have virtually no effect on the excretion of potassium, for example, tripas, but there are those that have a significant effect on its balance in the body.
The diuretic effect of diuretics from the group of thiazides (hydrochlorothiazide, furosemide) is based on the removal of sodium from the body, followed by the removal of water. But in addition to sodium, these diuretics also remove potassium. Blood pressure mediators usually simultaneously produce a diuretic effect, but they have a potassium-saving mechanism, so it is not recommended to take potassium preparations simultaneously with them to avoid intoxication from an overdose of this element. Another nuance is related to the presence of magnesium in the body. Magnesium deficiency prevents the absorption of potassium and prevents the restoration of the balance of this element in the body.
Monitor your magnesium level, try to replenish it if necessary, then taking potassium-containing drugs will give the desired effect.
Torasemide
This diuretic drug is one of the most effective today. "Torasemide" is prescribed for acute and chronic heart failure, as well as renal failure. The product can also be taken to prevent edema. The drug effectively reduces high blood pressure by quickly removing excess fluid and sodium salts. The effect occurs an hour after administration and lasts 12-18 hours. Patients note that the diuretic effect does not occur immediately, so in the first hour after taking the drug you do not have to limit your activity. "Torasemide" is inexpensive and works well to relieve swelling of the face. You can buy diuretic tablets with a prescription; there are some side effects.
Torasemide
Berezovsky Pharmaceutical Plant, Russia
Edema syndrome of various origins, incl.
for chronic heart failure, diseases of the liver, kidneys and lungs; - arterial hypertension. from 81
436
- Like
- Write a review
pharmachologic effect
Diuretics increase the volume of urine excreted by reducing the reabsorption (reabsorption) of water in the tubules or by increasing the filtration of primary urine in the capillaries of the nephron glomeruli - the structural and functional units of the kidneys.
In addition, diuretic drugs have a decongestant effect and also reduce blood pressure, intracranial pressure, and intraocular pressure.
Diuretics of plant origin additionally have anti-inflammatory and antimicrobial effects.
Triampur compositum
This diuretic does not have a very pronounced effect and does not remove potassium from the body, only water, salts and toxins. That is why Triampur compositum is considered the safest diuretic drug, which is prescribed for edema due to chronic heart failure and liver problems. Triampur begins to act 15 minutes after administration, and the effect lasts about 12 hours. Doctors say that this diuretic is safe for relieving facial swelling, is quickly absorbed into the gastrointestinal tract, and has a gentle effect.
Triampur compositum
AVD.pharma, Croatia
-arterial hypertension;
—edematous syndrome of various origins (with chronic heart failure, nephrotic syndrome, liver cirrhosis). from 256
306
- Like
- Write a review
DIURETICS (CLASS S 5)[edit | edit code]
According to the 2008 List of Prohibited Substances and Methods, masking agents include various types of diuretics.
Diuretics in the List of Prohibited Substances and Methods (2008) are represented by the drugs acetazolamide, amiloride, bumetanide, canrenone, chlorthalidone, ethacrynic acid, furosemide, indapamide, metolazone, spironolactone, thiazides (for example, bendroflumethiazide, chlorothiazide, hydrochlorothiazide), triamterene, and other substances with a similar chemical structure or similar biological effects (with the exception of drosperinone, which is not prohibited). With regard to diuretics, it is noted that the permit for their therapeutic use is not valid if the athlete’s urine, in addition to the diuretic, contains another prohibited substance in a threshold or subthreshold concentration.
Diuretics (diuretics)
- medicines of different chemical structures that help increase the formation and excretion of urine. Due to the fact that in the mechanism of the diuretic action of most drugs the main role is played by increasing the excretion of salts from the body, drugs in this group are also called saluretics (Latin sal - salt).
Historical background[edit | edit code]
The history of diuretics is quite interesting. Edema has attracted attention since ancient times. Throughout the existence of medicine, intensive searches have been carried out for organic and inorganic substances, which today we classify as diuretics. These searches were unsuccessful, and by the beginning of the 20th century. medicine had in its arsenal very weak drugs - calomel, sea onion, etc. Later, ineffective drugs (close to caffeine) were also used. Only in 1919-1920. By chance, due to a medical error, the diuretic effect of mercury compounds used in the treatment of syphilis was discovered. These were the first highly active diuretics, but they had significant toxicity. Now diuretic mercury drugs are not used, but their study played a huge role in the development of modern ideas about the diuretic and extrarenal mechanisms of action of diuretics. Thanks to these data, since the 1960s, dozens of groups of diuretics with different mechanisms of action have been created, used in practical work, and designed according to predetermined properties in an unusually short time.
Amiloride was isolated in 1966 as a result of exploratory screening for antikaliuretic activity of 25 thousand purposefully synthesized compounds. The creation of thiazides and other modern diuretics is associated with observations in which it was discovered that patients receiving sulfonamides developed metabolic acidosis with alkalinization of urine. It has been established that these drugs cause diuresis with the release of sodium bicarbonate. Understanding the possible benefit of this diuretic effect led to the development of acetazolamide and later the thiazides.
When acetazolamide's competitor, dichlorphenamide, was synthesized, it was found to increase sodium chloride excretion to a greater extent relative to sodium bicarbonate excretion. This change appeared to be desirable, indicating a mechanism of action other than carbonic anhydrase inhibition. Further modifications of the molecule led to the creation of disulfamoylchloroaniline, although a weak diuretic, but which served as the basis for the synthesis of the cyclic compound chlorothiazide (the first thiazide). This compound had little effect on carbonic anhydrase activity, but selectively inhibited the reabsorption of sodium chloride in the distal tubules. Loop diuretics were subsequently created based on thiazides.
It should be noted that scientists of the former USSR - physiologists, pharmacologists and clinicians E. B. Berkhin, A. V. Vinogradov, A. G. Ginetsinsky, G. A. Glezer, O. M. Eliseev, A. A. Lebedev, A. K. Merzon, Yu. V. Natochin, M. Ya. Ratner, B. A. Sidorenko, E. M. Tareev and others - made a significant contribution to the study of the mechanism of action of diuretics and the features of their use in various diseases.
Of all the diuretics in sports, furosemide is most often used, for the use of which in 1988, in particular, the Bulgarian weightlifters M. Grablev and A. Genchov were disqualified.
Diuver
Modern diuretic tablets from the group of loop diuretics. The active ingredient of the drug, turasemide, copes well with edema of various natures. “Diuver” has the mildest, prolonged action; the effect after administration occurs within 3-4 hours. Although it is not a potassium-sparing diuretic, it removes much less potassium than other diuretics. Diuver is prescribed for diseases of the kidneys, liver, lungs and heart failure. You can buy Diuver with a prescription (by the way, it is not cheap), be sure to familiarize yourself with the contraindications and side effects.
Diuver
JSC "Biolek", Ukraine
- edematous syndrome of various origins, incl.
for chronic heart failure, diseases of the liver, kidneys and lungs; - arterial hypertension. from 236
613
- Like
- Write a review
Natural Diuretics
Photos from open sources
How to replenish potassium loss
Under normal conditions, when you do not suffer from kidney disease, hypertension, edema of various natures, you do not often engage in grueling training or heavy physical work with intense sweating, potassium from food is enough for you. Good sources of potassium include tea, natural coffee, cocoa powder, all nuts and sunflower seeds, and raisins. Instead of sodium salt, you can use preventive food salt containing potassium salts.
The daily intake of potassium for an adult ranges from 2 to 4 grams. For significant physical activity – up to 5 grams. In total, a woman’s body should contain approximately 225 g of potassium, and a man’s body should have 250 g.
A whole series of drugs has been developed to simultaneously restore the balance of potassium and magnesium. The drug “Potassium-magnesium aspartate” and others like it restore electrolyte balance, replenish potassium and magnesium reserves, and normalize metabolic processes. The drugs “Aspangin”, “Asparkad”, “Asparkam” have a similar effect.
If you are taking triazides diuretics or diuretic herbs, you should then replenish your potassium balance with the help of Asparkam and Panangin. If you take a diuretic and Asparkam together, this will protect you from potassium loss. One Asparkam tablet contains 14.3 mg of potassium. The Panangina tablet contains 36.2 mg.
The selection of drugs should be entrusted to a doctor, because their combinations and mutual influence, if chosen independently, can lead to an overdose of potassium and harmful consequences for the entire body.
Dog-rose fruit
In addition to medicinal diuretics, herbal drugs have a mild diuretic effect. Firstly, it is rosehip. In addition to being a diuretic, it is famous for its general strengthening effect, helping the body resist various infections (also for urinary tract diseases). Rosehip improves the functioning of the digestive and cardiovascular systems. The value of rosehip is that it contains a lot of useful vitamins. Rose hips relieve swelling, reduce cholesterol levels, normalize blood clotting, and help cells recover faster.
Rosehip fruits
OJSC Krasnogorskleksredstva, Russia
For the prevention of hypovitaminosis C and R. In the complex therapy of acute and chronic infectious diseases, asthenic conditions, during the period of recovery after serious illnesses, surgical operations
from 28
379
- Like
- Write a review
When does a doctor prescribe diuretics?
List of indications for use:
- Arterial hypertension not complicated by renal failure
. A decrease in systolic pressure occurs due to a decrease in blood volume in the vascular system. There is no sharp drop in pressure; its levels decrease moderately, without the development of hypotension. The hypotensive effect is achieved by increasing the potassium content and decreasing sodium. After 1-2 months, diastolic pressure normalizes while maintaining cardiac output. Diuretics are not addictive and do not affect potency or libido.
- Chronic circulatory failure due to edema and arterial hypertension
. To correct this condition, strong diuretics of short and medium duration are used. Indications for emergency treatment: pulmonary edema, cerebral edema, barbiturate poisoning.
- Prevention of hypokalemia and secondary hyperaldosteronism
against the background of hypertension and chronic renal failure.
- Diabetes insipidus.
- Glaucoma.
Diuretic collection
Herbal infusions are very popular for the treatment of many diseases, including as a diuretic for edema. Diuretic collection in complex treatment helps cure urinary tract infections. Medicinal herbs in the diuretic collection act very gently, relieve spasms and inflammation. A diuretic preparation is often prescribed for cystitis; it is suitable for preventing relapses of this disease and is available in almost every pharmacy. Disadvantages include an unpleasant taste and green coloration of urine.
Diuretic collection
ST-Medipharm, Russia
Combined product of plant origin.
It has diuretic, anti-inflammatory, antiseptic, antispasmodic effects. from 76
5.0 1 review
262
- Like
- Write a review
Juniper fruits
Juniper helps with urinary tract infections by reducing inflammation and destroying germs. And thanks to the diuretic effect, pathogenic microflora is quickly eliminated from the body. Juniper fruits are also used as an appetite stimulant and to improve the functioning of the gastrointestinal tract. In addition, this herbal preparation stabilizes blood pressure and has a mild laxative effect. Contraindications include pregnancy, breastfeeding and childhood.
Juniper fruits
OJSC Krasnogorskleksredstva, Russia
In the complex treatment of edematous syndrome (with heart failure, insufficiency of kidney and/or liver function), cystitis
from 41
212
- Like
- Write a review