Composition per tablet:
| Active ingredient, mg: | ||
| Simvastatin (calculated as 100% substance) | 10.00 mg | 40.00 mg |
| Excipients, mg: | ||
| Crospovidone | 3,00 | 12,00 |
| Lemon acid | 1,25 | 5,00 |
| Magnesium stearate | 1,00 | 4,00 |
| Potato starch | 0,50 | 2,00 |
| Ascorbic acid | 0,25 | 1,00 |
| Butylated hydroxytoluene | 0,02 | 0,08 |
| Lactose monohydrate to obtain an uncoated tablet weighing: | 100,00 | 400,00 |
| Excipients of the shell, mg: | to obtain the coated tablet mass: | |
| 102,50 | 410,00 | |
| Mixture for preparing film coating “Opadray® white” [hypromellose 2910 - 30.0%, hyprolose - 30.0%, talc - 20.0%, titanium dioxide - 20.0%]. | 2,50 | 10,00 |
Description:
Round biconvex tablets, film-coated, white or almost white. On a cross section, the kernel is almost white or white with a yellowish tint.
Pharmacotherapeutic group:
Lipid-lowering agent – HMG-CoA reductase inhibitor.
ATX code:
S10AA01
Pharmacological properties
The drug Simvastatin is a lipid-lowering drug obtained synthetically from a fermentation product of Aspergillus terreus
.
Pharmacodynamics:
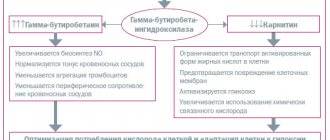
After oral administration, simvastatin, which is an inactive lactone, undergoes hydrolysis in the liver to form the corresponding form (β-hydroxy acid of simvastatin, which is the main metabolite and has high inhibitory activity against HMG-CoA (3-hydroxy-3-methylglutaryl coenzyme A) reductase, an enzyme that catalyzes the initial and most significant stage of cholesterol biosynthesis.Clinical studies have shown the effectiveness of the drug simvastatin in reducing the concentration of total cholesterol (TC) in the blood plasma, low-density lipoprotein cholesterol (LDL-C), triglycerides (TG) and very low lipoprotein cholesterol density (VLDL-C), as well as an increase in the concentration of high-density lipoprotein cholesterol (HDL-C) in patients with heterozygous familial and non-familial hypercholesterolemia or mixed hyperlipidemia in cases where increased cholesterol concentration is a risk factor and the prescription of diet alone is not enough. A noticeable therapeutic effect is observed within 2 weeks of taking the drug, the maximum therapeutic effect is within 4-6 weeks after the start of treatment. The effect persists with continued therapy. When you stop taking simvastatin, cholesterol concentrations return to the original value observed before treatment.
The active metabolite of simvastatin is a specific inhibitor of HMG-CoA reductase, an enzyme that catalyzes the formation of mevalonate from HMG-CoA. Despite this, taking the drug Simvastatin in therapeutic doses does not lead to complete inhibition of HMG-CoA reductase, which allows maintaining the production of the biologically necessary amount of mevalonate. Since the early stage of cholesterol biosynthesis is the conversion of HMG-CoA to mevalonate, it is believed that the use of the drug Simvastatin should not cause the accumulation of potentially toxic sterols in the body. In addition, HMG-CoA is rapidly metabolized back to acetyl-CoA, which is involved in many biosynthetic processes in the body.
Although cholesterol is a precursor to all steroid hormones, no clinical effect of simvastatin on steroidogenesis has been observed. Since simvastatin did not increase bile lithogenicity, it is unlikely to increase the incidence of cholelithiasis.
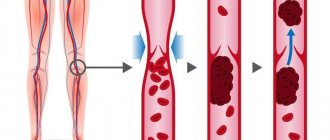
Simvastatin reduces both elevated and normal concentrations of LDL cholesterol. LDL is formed from very low-density lipoproteins (VLDL). LDL catabolism is predominantly mediated by the high-affinity LDL receptor. The mechanism for reducing the concentration of LDL cholesterol after taking simvastatin may be due to both a decrease in the concentration of VLDL cholesterol and activation of LDL receptors, which leads to a decrease in the formation and increased catabolism of LDL cholesterol. Simvastatin therapy also significantly reduces the concentration of apolipoprotein B (apo B). Since each LDL particle contains one molecule of apo B, and small amounts of apo B are found in other lipoproteins, it can be assumed that simvastatin not only causes loss of cholesterol in LDL particles, but also reduces the concentration of circulating LDL particles.
In addition, simvastatin increases the concentration of HDL cholesterol and reduces the concentration of TG in the blood plasma. As a result of these changes, the TC/HDL-C and LDL-C/HDL-C ratios decrease.
In the Simvastatin Survival Effects Study, the impact of simvastatin therapy on overall mortality (median patient participation time 5.4 years) was assessed in 4444 patients with coronary artery disease (CAD). Simvastatin reduced the risk of total mortality, mortality from coronary artery disease, and the incidence of nonfatal confirmed myocardial infarction. Simvastatin also reduced the risk of the need for surgical interventions to restore coronary blood flow (coronary artery bypass grafting or percutaneous transluminal coronary angioplasty). In patients with diabetes, the risk of major coronary events was also reduced. Moreover, simvastatin significantly reduced the risk of fatal and non-fatal cerebrovascular accidents (stroke and transient cerebrovascular accident).
In the 5-year Cardiac Protection Study, the effectiveness of simvastatin therapy was demonstrated in 20,536 patients with or without hyperlipidemia who were at high risk for developing coronary artery disease due to concomitant diabetes mellitus, a history of stroke, and other vascular diseases. In this study, simvastatin 40 mg per day compared with placebo reduced overall mortality, the risk of death attributable to coronary artery disease, the risk of major coronary events (including nonfatal myocardial infarction or death attributable to coronary artery disease), and the need for surgical interventions to restore coronary blood flow. (including coronary artery bypass grafting and percutaneous transluminal angioplasty), as well as peripheral blood flow and other types of non-coronary revascularization. Simvastatin reduced the risk of stroke, as well as the risk of hospitalization for angina pectoris. The risk of major coronary and vascular complications was reduced in patients with or without coronary artery disease, including patients with diabetes mellitus, peripheral vascular disease, or cerebrovascular disease. In patients with diabetes mellitus, simvastatin reduced the risk of developing serious vascular complications, including the need for surgical interventions to restore peripheral blood flow, amputation of the lower extremities, and the occurrence of trophic ulcers.
In another study of 404 patients, simvastatin (as measured by coronary angiography using quantitative assessment of coronary blood flow) slowed the progression of coronary atherosclerosis and the appearance of both new areas of atherosclerosis and new total occlusions, whereas patients receiving standard therapy showed steady progression of atherosclerotic lesions. damage to the coronary arteries. Subgroup analysis from two studies, which included 147 patients with hypertriglyceridemia (Fredrickson type IV hyperlipidemia), showed that simvastatin at a dose of 20 to 80 mg per day reduced the concentration of TG, LDL cholesterol, and non-high-density lipoprotein cholesterol (HLC). non-HDL, calculated as the difference between the concentration of total cholesterol and the concentration of HDL cholesterol) and increased HDL cholesterol.
In an analysis of another subgroup of 7 patients with dysbetalipoproteinemia (hyperlipidemia type III according to the Fredrickson classification), simvastatin at a dose of 80 mg per day reduced the concentration of LDL-C, including intermediate-density lipoproteins (IDL), as well as the concentration of VLDL-C and VLDL.
Pharmacokinetics:
Metabolism
Simvastatin is an inactive lactone that is rapidly hydrolyzed to simvastatin β-hydroxy acid (L-654.969), a potent inhibitor of HMG-CoA reductase. The main metabolites of simvastatin in blood plasma are β-hydroxy acid of simvastatin (L-654.969) and its 6′-hydroxy, 6′-hydroxymethyl and 6′-exomethylene derivatives. HMG-CoA reductase inhibition is the quantification criterion for all pharmacokinetic studies of β-hydroxy acid metabolites (active inhibitors) and active and latent inhibitors (all inhibitors) resulting from hydrolysis. Both types of metabolites are detected in blood plasma when simvastatin is taken orally.
Hydrolysis of simvastatin mainly occurs during the “first pass” through the liver, therefore the concentration of unchanged simvastatin in human plasma is low (less than 5% of the dose taken). The maximum concentration (Cmax) in the blood plasma of simvastatin metabolites is reached 1.3-2.4 hours after oral administration of a single dose. In a study with 14C-labeled simvastatin, plasma concentrations of total radioactivity (14C-labeled simvastatin + 14C-labeled simvastatin metabolites) peaked at 4 hours and decreased rapidly to approximately 10% of the maximum within 12 hours of a single oral dose. Despite the fact that the range of recommended therapeutic doses of simvastatin is from 5 to 80 mg per day, the linear nature of the AUC profile (area under the concentration-time curve) of active metabolites in the general bloodstream is maintained when the dose is increased to 120 mg.
Suction
About 85% of the ingested dose of simvastatin is absorbed.
Eating (as part of a standard cholesterol-lowering diet) immediately after taking simvastatin does not affect the pharmacokinetic profile of the drug.
Distribution
After oral administration, higher concentrations of simvastatin are detected in the liver than in other tissues.
The concentration of the active metabolite of simvastatin L-654,969 in the systemic circulation is less than 5% of the oral dose; 95% of this amount is in a protein-bound state.
The result of active metabolism of simvastatin in the liver (more than 60% in men) is its low concentration in the general bloodstream.
The possibility of simvastatin penetrating the blood-brain barrier and the blood-placental barrier has not been studied.
Removal
During the “primary passage” through the liver, simvastatin is metabolized with subsequent excretion of simvastatin and its metabolites in the bile.
In a study, when taking 100 mg of the drug (5 capsules of 20 mg), 14C-labeled simvastatin accumulated in the blood, urine and feces. About 60% of the administered dose of labeled simvastatin was detected in feces and about 13% in urine. Labeled simvastatin in feces was represented by both metabolic products of simvastatin excreted in bile and unabsorbed labeled simvastatin. Less than 0.5% of the administered dose of labeled simvastatin was detected in the urine as active simvastatin metabolites. In plasma, 14% of AUC was due to active inhibitors and 28% to all HMG-CoA reductase inhibitors. The latter indicates that the metabolic products of simvastatin are mainly inactive or weak inhibitors of HMG-CoA reductase.
In a dose proportionality study of simvastatin 5, 10, 20, 60, 90, and 120 mg, no significant deviation from linearity in total circulation AUC was observed with increasing dose. Pharmacokinetic parameters for single and repeated oral administration of simvastatin showed that simvastatin does not accumulate in tissues after repeated oral administration.
In a study in patients with severe renal impairment (creatinine clearance (CR) less than 30 mL/min), the total plasma concentration of HMG-CoA reductase inhibitors after oral administration of a single dose of a corresponding HMG-CoA reductase inhibitor (statin) was approximately 2 times higher than in healthy volunteers.
In a study involving healthy volunteers, the use of simvastatin at a maximum dose of 80 mg did not affect the metabolism of midazolam and erythromycin, which are substrates of the CYP3A4 isoenzyme. This means that simvastatin is not an inhibitor of the CYP3A4 isoenzyme and suggests that oral administration of simvastatin does not affect the plasma concentrations of drugs metabolized by the CYP3A4 isoenzyme.
Cyclosporine is known to increase the AUC of HMG-CoA reductase inhibitors, although the mechanism of drug interaction is not fully understood. The increase in simvastatin AUC is presumably due, in particular, to inhibition of the CYP3A4 isoenzyme and/or the transport protein OATP1B1 (see Contraindications).
In a pharmacokinetic study, when coadministered with diltiazem, there was a 2.7-fold increase in the AUC of the β-hydroxy acid simvastatin, presumably due to inhibition of the CYP3A4 isoenzyme (see Precautions, Myopathy/Rhabdomyolysis
).
In a pharmacokinetic study, when used concomitantly with amlodipine, an increase in the AUC of the β-hydroxy acid simvastatin was observed by 1.6 times (see Special Instructions, Myopathy/Rhabdomyolysis
).
In a pharmacokinetic study, with the simultaneous use of a single dose of 2 g of nicotinic acid sustained release and simvastatin 20 mg, a slight increase in the AUC of simvastatin and simvastatin β-hydroxy acid and Cmax of simvastatin β-hydroxy acid in plasma was observed (see Special Instructions, Myopathy/Rhabdomyolysis
).
The specific pathways for the metabolism of fusidic acid in the liver are unknown, but it can be assumed that there is an interaction between fusidic acid and statins, which are metabolized by the CYP3A4 isoenzyme (see Special instructions, Myopathy/Rhabdomyolysis
).
The risk of developing myopathy increases with increasing concentrations of HMG-CoA reductase inhibitors in the blood plasma. Potent inhibitors of the CYP3A4 isoenzyme may increase the concentration of HMG-CoA reductase inhibitors and lead to an increased risk of developing myopathy (see Interaction with other drugs; Special instructions, Myopathy/Rhabdomyolysis
).
Special patient groups
SLC01B1 gene polymorphism
Carriers of the c.521T>C allele of the SLC01B1 gene have lower activity of the OATP1B1 transport protein. The AUC of the main active metabolite, the hydroxy acid simvastatin, is 120% in heterozygous carriers (CT) of the C allele and 221% in homozygous carriers (CC), relative to patients with the most common genotype (TT). The frequency of occurrence of the C allele in the European population is 18%. Patients with the SLC01B1 gene polymorphism are at risk of increased exposure to the hydroxyacid simvastatin, which may lead to an increased risk of rhabdomyolysis (see Precautions).
What is Simvastatin and what is its composition?
Simvastatin is the active ingredient of the drug of the same name.
This is a synthetic lipid-lowering drug from the group of statins, produced by a special fungus from the genus Aspergillus through fermentation. It is an inactive compound that is transformed in the body through chemical reactions into an active structure. The mechanism of action of this drug is to inhibit the synthesis of mevalonte from HMG-CoA. This is the first link in the cascade of transformations leading to the formation of cholesterol.
As a result, the alkaloid Simvastatin leads to a decrease in the level of triglycerides, low-density lipoproteins and very low-density lipoproteins, instead increasing the concentration of high-density lipoproteins. At the same time, it is safer, unlike its predecessors, due to the lack of mutagenic action and influence on the synthesis of steroid hormones.
The drug produces an effect only 1.5-2 weeks after the start of use, which persists only with regular use. If the patient stops the course of treatment, cholesterol returns to the starting level.
Presented in the form of coated tablets, dissolving in the intestines, in a dosage of 10 or 20 mg of the active substance.
Indications for use:
Patients with coronary heart disease or at high risk of coronary artery disease
In patients at high risk for developing CAD (with or without hyperlipidemia), such as patients with diabetes mellitus, patients with a history of stroke or other cerebrovascular disease, patients with peripheral vascular disease, or patients with CAD or a predisposition to CAD Simvastatin is indicated for:
- Reducing the risk of overall mortality by reducing mortality due to coronary artery disease.
- Reducing the risk of serious vascular and coronary complications:
- non-fatal myocardial infarction,
- coronary death,
- stroke,
- revascularization procedures.
- Reducing the risk of the need for surgical interventions to restore coronary blood flow (such as coronary artery bypass grafting and percutaneous transluminal coronary angioplasty).
- Reducing the risk of the need for surgical interventions to restore peripheral blood flow and other types of non-coronary revascularization.
- Reducing the risk of hospitalization due to angina attacks.
Hyperlipidemia
- As an adjunct to diet, when diet alone and other non-drug treatments in patients with primary hypercholesterolemia, including heterozygous familial hypercholesterolemia (Fredrickson hyperlipidemia type IIa), or mixed hypercholesterolemia (Fredrickson hyperlipidemia type IIb), are insufficient to:
- reducing the increased concentration of total cholesterol, LDL cholesterol, TG, apolipoprotein B (apo B);
- increasing the concentration of HDL cholesterol;
- reducing the ratio of LDL cholesterol/HDL cholesterol and TC/HDL cholesterol.
- Hypertriglyceridemia (hyperlipidemia type IV according to the Fredrickson classification).
- Adjunct to diet and other treatments in patients with homozygous familial hypercholesterolemia to reduce elevated total cholesterol, LDL cholesterol, and apo B.
- Primary dysbetalipoproteinemia (hyperlipidemia type III according to the Fredrickson classification).
Use in children and adolescents with heterozygous familial hypercholesterolemia
The use of the drug Simvastatin simultaneously with a diet is indicated to reduce the increased concentration of total cholesterol, LDL cholesterol, TG, apo B in boys 10-17 years old and in girls 10-17 years old at least 1 year after menarche (first menstrual bleeding) with heterozygous familial hypercholesterolemia .
Contraindications:
- Hypersensitivity to any component of the drug.
- Liver disease in the active phase or persistent increase in the activity of “liver” transaminases in the blood plasma of unknown etiology.
- Pregnancy or breastfeeding period.
- Age up to 18 years (except for children and adolescents 10-17 years old with heterozygous familial hypercholesterolemia) (see Indications for use).
- Lactose intolerance, lactase deficiency or glucose-galactose malabsorption.
- Concomitant treatment with potent inhibitors of the CYP3A4 isoenzyme (itraconazole, ketoconazole, posaconazole, voriconazole, HIV protease inhibitors, boceprevir, telaprevir, erythromycin, clarithromycin, telithromycin, nefazodone and drugs containing cobicistat) (see Interaction with other drugs; Special instructions, Myopathy /Rhabdomyolysis
). - Concomitant treatment with gemfibrozil, cyclosporine or danazol (see Interactions with other drugs; Special instructions, Myopathy/Rhabdomyolysis
). - Concomitant use of simvastatin at a dose exceeding 40 mg with lomitapide in patients with homozygous familial hypercholesterolemia (see Interaction with other drugs, Other drug interactions
; Special instructions,
Myopathy/Rhabdomyolysis
).
What analogues of Simvastatin are present on the Russian market?
Structural substitutes for this drug include:
Actalipid;- Simvacard;
- Zorstat;
- Kholvasim;
- Simvor;
- Zokor;
- Syncard.
The following medications have a similar effect:
- Atorvastatin;
- Rosuvastatin;
- Lovasterol;
- Pravastatin;
- Kholvasim.
Carefully:
Severe renal dysfunction (creatinine clearance less than 30 ml/min); alcohol abuse before treatment; history of liver disease; hereditary muscle diseases, myopathy due to a history of taking statins, decreased or increased skeletal muscle tone of unknown etiology; uncontrolled hypothyroidism; planned surgical interventions, severe therapeutic and surgical diseases; simultaneous use with fibrates (except fenofibrate), nicotinic acid in lipid-lowering doses (more than 1 g/day), amiodarone, amlodipine, verapamil, diltiazem, ranolazine, dronedarone, grapefruit juice; diabetes; use in patients of the Mongoloid race, old age (over 65 years, especially women).
Drug interactions Simvastatin
The risk of developing myopathy increases with concomitant treatment with drugs that cause the development of myopathy when administered alone (gemfibrozil and other fibrates), as well as nicotinic acid in hypolipidemic doses (more than 1 g/day). Simvastatin and other HMG-CoA reductase inhibitors are metabolized by the cytochrome P450 isoform 3A4, so drugs that, at therapeutic doses, have an inhibitory effect on this metabolic pathway may significantly increase plasma levels of HMG-CoA reductase inhibitors and thus increase the risk of developing myopathy. These include cyclosporine, mibefradil (a calcium antagonist of the tetralol class), itraconazole, ketoconazole and other azole antifungals, macrolide antibiotics (erythromycin, clarithromycin), and the antidepressant nefazodone. Simvastatin may enhance the effect of coumarin anticoagulants.
Use during pregnancy and breastfeeding:
Pregnancy
The drug Simvastatin is contraindicated in pregnant women. Since safety for pregnant women has not been proven and there is no evidence that treatment with the drug during pregnancy brings obvious benefits, the drug should be stopped immediately if pregnancy occurs. Simvastatin should be prescribed to women of childbearing age only in cases where the likelihood of pregnancy is very low. Use of the drug Simvastatin during pregnancy may reduce the concentration of mevalonate (a precursor in cholesterol biosynthesis) in the fetus. Atherosclerosis is a chronic disease and usually stopping lipid-lowering drugs during pregnancy has little effect on the long-term risks associated with primary hypercholesterolemia. Therefore, Simvastatin should not be used in women who are pregnant, trying to become pregnant, or suspect that they are pregnant. Treatment with Simvastatin should be suspended for the entire duration of pregnancy or until pregnancy is diagnosed, and the woman herself is warned about the possible danger to the fetus (see Contraindications).
Breast-feeding
There are no data on the excretion of simvastatin and its metabolites in breast milk. If it is necessary to prescribe Simvastatin to a woman during lactation, it should be taken into account that many drugs are excreted in breast milk, and there is a risk of developing serious adverse reactions. As a result, if breastfeeding, the drug should be discontinued.
Fertility
There are no data on the effect of simvastatin on fertility in women. Simvastatin has no effect on fertility in male or female rats.
Directions for use and dosage:
To ensure the indicated dosage regimens, if it is necessary to use simvastatin at a dose of 5 mg per day, drugs from other manufacturers should be prescribed, in the dosage form of “5 mg tablets” or “10 mg tablets” with a score.
Before starting treatment with Simvastatin, the patient should be prescribed a standard cholesterol-lowering diet, which must be followed throughout the course of treatment.
Recommended doses of Simvastatin are from 5 to 80 mg per day. The drug should be taken once a day in the evening. If necessary, the dose of the drug is increased at intervals of at least 4 weeks to a maximum of 80 mg 1 time per day in the evening. A dose of 80 mg per day is recommended only for patients at high risk of cardiovascular complications, if treatment with the drug at lower doses has not achieved target lipid levels, and the expected benefit of therapy outweighs the possible risk (see Special Instructions, Myopathy/Rhabdomyolysis
).
Patients with coronary heart disease or high risk of developing coronary artery disease
The standard starting dose of Simvastatin for patients with a high risk of developing coronary artery disease in combination with or without hyperlipidemia (in the presence of diabetes mellitus, previous stroke or other history of cerebrovascular diseases, peripheral vascular diseases), as well as for patients with coronary artery disease is 40 mg 1 time per day in the evening. Drug therapy should be prescribed simultaneously with diet and physical therapy.
Patients with hyperlipidemia who do not have the above risk factors
The standard starting dose of Simvastatin is 20 mg once daily in the evening. For patients who require a significant (more than 45%) reduction in LDL cholesterol concentrations, the initial dose may be 40 mg once daily in the evening. In patients with mild or moderate hypercholesterolemia, therapy with Simvastatin can be prescribed at an initial dose of 10 mg once daily. If necessary, dose selection should be carried out in accordance with the above scheme (see Dosage and Administration).
Patients with homozygous familial hypercholesterolemia
The drug Simvastatin is recommended at a dose of 40 mg per day, taken once in the evening. A dose of 80 mg is recommended to be prescribed only if the expected benefit of therapy outweighs the possible risk (see Special instructions, Myopathy/Rhabdomyolysis
). In such patients, Simvastatin is used in combination with other lipid-lowering treatments (eg, LDL apheresis) or without such treatment if it is not available.
For patients taking lomitapide concomitantly with Simvastatin, the daily dose of Simvastatin should not exceed 40 mg (see Interactions with other drugs; Special instructions, Myopathy/Rhabdomyolysis
).
Concomitant therapy
The drug Simvastatin can be prescribed both in monotherapy and in combination with bile acid sequestrants.
In patients taking Simvastatin concomitantly with fibrates other than gemfibrozil (see Contraindications) or fenofibrate, the maximum recommended dose of Simvastatin is 10 mg per day.
For patients taking amiodarone, verapamil, diltiazem, drugs containing elbasvir or grazoprevir or amlodipine simultaneously with simvastatin, the daily dose of simvastatin should not exceed 20 mg. (See Interaction with other drugs; Special instructions, Myopathy/Rhabdomyolysis
)
Concomitant use of Simvastatin tablets containing 40 mg with fibrates (except fenofibrate), amiodarone, amlodipine, verapamil, diltiazem or drugs containing elbasvir or grazoprevir may increase the risk of myopathy/rhabdomyolysis. If it is necessary to simultaneously use simvastatin in doses of 10 mg and 20 mg, it is advisable to prescribe simvastatin preparations (tablets containing 10 mg and 20 mg of simvastatin).
If kidney function is impaired
Since simvastatin is excreted in small amounts by the kidneys, there is no need for dosage adjustments in patients with moderate renal impairment. In patients with severe renal failure (creatinine clearance <30 ml/min), the advisability of prescribing the drug in doses exceeding 10 mg per day should be carefully considered. If such dosages are considered necessary, they should be administered with caution (see Precautions).
Use in children and adolescents 10-17 years old with heterozygous familial hypercholesterolemia
The recommended starting dose is 10 mg per day in the evening. The recommended dosage regimen is 10-40 mg per day, the maximum recommended dose of the drug is 40 mg per day. Doses are selected individually in accordance with the goals of therapy.
Special instructions for the use of the drug Simvastatin
Simvastatin and other HMG-CoA reductase inhibitors sometimes cause myopathy, which is manifested by myalgia or muscle weakness associated with a significant increase in creatine kinase levels. Rhabdomyolysis is rare. Simvastatin therapy should be discontinued if myopathy is diagnosed or suspected. Before prescribing simvastatin and periodically during treatment, for 1 year or up to a year after the last dose increase, liver function should be monitored in all patients. Patients whose dose was increased to 80 mg should be re-examined after 3 months. Particular attention should be paid to patients with elevated levels of transaminases in the blood plasma. They need to immediately re-test these indicators, and repeat the tests more often during treatment. If there is a tendency to increase the level of plasma transaminases, especially if it consistently exceeds the upper limit of normal by more than 3 times, treatment should be stopped. Prescribe with caution to persons who abuse alcohol, as well as with a history of liver disease. Liver disease in the acute period or an unexplained increase in plasma transaminases are contraindications to treatment with simvastatin. The safety and effectiveness of simvastatin in children has not been established.
Side effect:
Simvastatin is generally well tolerated, and most side effects are mild and transient. Less than 2% of patients participating in clinical trials discontinued treatment due to the development of adverse events characteristic of Simvastatin drugs.
In pre-registration clinical studies, adverse events occurring with a frequency of at least 1% and assessed by the investigators as possibly, probably or definitely related to the drug were abdominal pain, constipation and flatulence. Other adverse events that occurred in 0.5-0.9% of patients were asthenia and headache.
There have been rare reports of the development of myopathy (see Special Instructions, Myopathy/Rhabdomyolysis).
In a clinical study in which 20,536 patients received simvastatin (n = 10,269 patients) at a dose of 40 mg per day or placebo (n = 10,267 patients) for an average of 5 years, the pattern of adverse events was similar in the simvastatin and placebo groups. The rate of treatment discontinuation due to adverse events was also comparable in the two groups (4.8% in the simvastatin group and 5.1% in the placebo group). The incidence of myopathy in patients taking simvastatin was less than 0.1%. An increase in liver transaminase activity (more than 3 times the upper limit of normal (ULN), confirmed in a repeat study) was observed in 0.21% of patients in the simvastatin group and 0.09% of patients in the placebo group.
World Health Organization (WHO) classification of the frequency of adverse reactions: very common (≥1/10); often (from ≥1/100 to <1/10); uncommon (from ≥1/1000 to <1/100); rare (from ≥1/10000 to <1/1000); very rare (from <1/10000); frequency unknown (cannot be estimated from available data).
Blood and lymphatic system disorders
Rarely: anemia.
Immune system disorders
Rarely: hypersensitivity syndrome developed, which was manifested by anaphylaxis, angioedema, lupus-like syndrome, polymyalgia rheumatica, dermatomyositis, vasculitis, thrombocytopenia, eosinophilia, increased erythrocyte sedimentation rate (ESR), arthritis, arthralgia, urticaria, photosensitivity, fever, flushing facial skin, shortness of breath and general weakness.
There have been very rare reports of immune-mediated necrotizing myopathy (autoimmune myopathy) associated with statin use. Immune-mediated myopathy is characterized by proximal muscle weakness and increased serum creatine phosphokinase (CPK) activity that persist despite discontinuation of statin treatment. Muscle biopsy shows necrotizing myopathy without significant inflammation. Improvement is observed with therapy with immunosuppressive drugs (see Special instructions, Myopathy Rhabdomyolysis).
There have also been rare post-marketing reports of cognitive impairment (eg, various memory impairments - forgetfulness, memory loss, amnesia, confusion) associated with the use of statins. These cognitive impairments have been reported with all statins. Reports were generally classified as non-serious, with varying duration to symptom onset (from 1 day to several years) and time to resolution (median 3 weeks). The symptoms were reversible and resolved after discontinuation of statin therapy.
Nervous system disorders
Rarely: dizziness, peripheral neuropathy, paresthesia.
Very rare: insomnia.
Frequency unknown: depression.
Respiratory, thoracic and mediastinal disorders
Not known: interstitial lung disease.
Gastrointestinal disorders
Rarely: dyspepsia, nausea, vomiting, diarrhea, pancreatitis, hepatitis/jaundice.
Very rare: fatal and non-fatal liver failure.
Skin and subcutaneous tissue disorders
Rarely: skin rash, itching, alopecia.
Musculoskeletal and connective tissue disorders
Rarely: myalgia, muscle cramps, rhabdomyolysis.
Frequency unknown: tendinopathy, possibly with tendon rupture.
Genital and breast disorders
Frequency not established: erectile dysfunction.
Laboratory and instrumental data
There are rare reports of the development of a pronounced and persistent increase in the activity of “liver” transaminases. Increased alkaline phosphatase and gamma-glutamyl transpeptidase activities have also been reported. Deviations in liver function tests are usually mild and transient. There is information about cases of increased CK activity (see Special instructions).
Increases in glycosylated hemoglobin (HbAlc) and fasting serum glucose concentrations have been reported with statins, including simvastatin.
The following adverse events have been reported with some statins:
- sleep disturbances, including nightmares;
- sexual dysfunction, gynecomastia.
Children and teenagers (10-17 years old)
In a clinical study of patients aged 10–17 years with heterozygous familial hypercholesterolemia, the safety and tolerability profile of treatment in the simvastatin group was comparable to the safety and tolerability profile of treatment in the placebo group (see Precautions, Use in Children and teenagers aged 10-17 years).