Introductory part
Before heart surgery, a person has many questions. Some of them we ask the doctor, and some we cannot even formulate. When we understand what is happening to our body and what we can do to restore health, it is easier for us to endure all procedures.
Acquired heart valve defects
- these are diseases that are based on morphological and/or functional disorders of the valve apparatus (valve leaflets, annulus fibrosus, chordae, papillary muscles), developed as a result of acute or chronic diseases and injuries, disrupting the function of the valves and causing changes in intracardiac hemodynamics.
Valve defects can be congenital or acquired.
Congenital defects occur when the structures of the heart are formed incorrectly during intrauterine development; sometimes they do not make themselves felt until adulthood. Acquired defects arise due to rheumatism, infection, metabolic disorders (when calcium is deposited in the valves), trauma and other reasons.
The main types of heart valve defects:
- mitral stenosis
- mitral valve insufficiency
- mitral valve prolapse
- aortic stenosis
- aortic valve insufficiency
- tricuspid stenosis
- tricupidal insufficiency
The normal functioning of the heart largely depends on the functioning of its valve apparatus.
Obstacles to the passage of blood cause overload, hypertrophy and expansion of the structures above the valve. Obstructed heart function disrupts the nutrition of the hypertrophied myocardium and leads to heart failure.
Etiology and pathogenesis
Etiology of stenosis
and combined rheumatic disease,
insufficiency
- usually rheumatic, rarely septic, atherosclerotic, traumatic, syphilitic.
Stenosis is formed as a result of cicatricial fusion or cicatricial rigidity of the valve leaflets and subvalvular structures; valve insufficiency - due to their destruction, damage or scar deformation.
Failure
valve damage occurs due to destruction or damage to its valve flaps. Valve insufficiency is characterized by incomplete closure of the leaflets and occurs as a result of their wrinkling, shortening, perforation or expansion of the fibrous valve ring, deformation or separation of the chordae and papillary muscles. In some cases, valve insufficiency develops as a result of dysfunction of the valve apparatus, in particular the papillary muscles.
Often stenosis and insufficiency develop on one valve (the so-called combined defect
).
In addition, there are cases when the defects affect two or more valves - this is called combined
heart disease.
Affected valves form an obstacle to the passage of blood - anatomical in case of stenosis, dynamic in case of insufficiency. The latter is that although some of the blood passes through the hole, it returns back in the next phase of the cardiac cycle.
A “parasitic” volume is added to the effective volume, performing a pendulum-like movement on both sides of the affected valve. Significant valvular insufficiency is complicated by relative stenosis (due to increased blood volume). Obstruction to the passage of blood leads to overload, hypertrophy and expansion of the overlying chambers of the heart.
The expansion is more significant with valve insufficiency, when the overlying chamber is stretched by additional blood. With stenosis of the atrioventricular orifice, the filling of the underlying chamber is reduced (left ventricle with mitral stenosis, right ventricle with tricuspid stenosis); There is no hypertrophy or expansion of the ventricle.
With valve insufficiency, the filling of the corresponding ventricle is increased, the ventricle is dilated and hypertrophied. Difficulty in the functioning of the heart due to improper functioning of the valve and degeneration of the hypertrophied myocardium leads to the development of heart failure.
to the top of the page
Structure
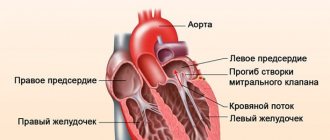
The mitral valve (MV) consists of a fibrous opening and leaflets that are attached around its circumference. The structure of the MV includes chordae tendineae, papillary papillary muscle fibers adjacent to the cardiac myocardium of the left ventricle, and its own fibromuscular ring. Each element ensures the normal functioning of the microcontroller.
Anatomy of the left atrioventricular orifice:
- The MV is divided into two valves by commissural septa, of which the anterior one is rounder and longer, the posterior one is short and somewhat reminiscent of a square;
- in some cases there may be from 3 to 5 valves;
- the number of additional elements depends on the size of the fibrous ring (AF);
- in the places where the valves close, papillary muscle fibers are attached (normally, a person has up to 3 anterior and 1-5 posterior muscles);
- tendon fibers (chordae) are attached to the fibrous surface of the MV, directed into the cavity of the left ventricle, which are further divided into threads for each leaflet;
- the movement of structures depending on the phase of contractility is smooth and precise;
- all elements ensure full opening of the bicuspid mitral valve of the heart in the antiphase diastole phase - multidirectional physiological movement of the valves, facilitating the outflow of blood.
Histological structure of the mitral valve
The main tissue components of MC:
- valves formed by three-layer connective tissue, attached to the atrioventricular opening;
- own valve ring made of fibrous and muscle tissue;
- the inner surface is lined with the lining of the heart, the endocardium;
- the middle section is made of spongy tissue.
What the mitral valve of the left chambers of the heart looks like and what it is is shown in the photo below:
Anatomy of the heart
A healthy heart is a strong, continuously working organ, about the size of a fist and weighing about half a kilogram.
In addition to maintaining steady, normal blood flow, it quickly adapts and adapts to the body's ever-changing needs.
For example, the heart pumps more blood when it is active and less when it is at rest. During the day, the heart produces an average of 60 to 90 beats per minute - 42 million beats per year!
The heart is a two-way pump that circulates blood throughout the body. It consists of 4 chambers.
A muscular wall called the septum divides the heart into left and right halves. Each half has 2 chambers.
The upper chambers are called atria, the lower chambers are called ventricles. The right atrium receives all the blood returning from the upper and lower parts of the body.
Then, through the tricuspid valve, it sends it to the right ventricle, which in turn pumps blood through the pulmonary valve to the lungs.
In the lungs, the blood is enriched with oxygen and returns to the left atrium, which sends it through the mitral valve to the left ventricle.
The left ventricle pumps blood through the arteries through the aortic valve throughout the body, where it supplies the tissues with oxygen. Oxygen-depleted blood returns through the veins to the right atrium.
Four valves (tricuspid, pulmonary valve, mitral, aortic) act as a door between the chambers, opening in one direction.
These valves help blood move forward and prevent it from flowing in the opposite direction.
The petals of a healthy valve are thin, flexible tissue of perfect shape. They open and close when the heart contracts or relaxes.
Heart valves can become abnormal due to birth defects. They can become damaged or scarred due to rheumatic fever, infection, hereditary factors, age or heart attacks.
The mitral valves are most susceptible to such changes.
Regardless of the case, the heart valve can become stenotic (narrowed opening) or insufficient (does not close completely).
With valve stenosis, the heart must work harder to pump the required amount of blood through the narrowed opening.
Valve insufficiency causes blood to flow backwards through the valve after it closes. Once again, the heart has to work harder to pump enough blood for the body's needs to make up for the deficiency caused by the backflow of blood.
Both cases - stenosis and failure - force the heart to work harder to pump the required amount of blood. This extra work can weaken the heart, cause it to enlarge, and cause various diseases.
to the top of the page
Mechanism and features of operation
The main function of the bicuspid atrioventricular valve is to prevent backflow (regurgitation) into the left atrium and direct its flow into the ventricle.
MK functions
All valve leaflets are mobile and pliable structures that move during contraction phases under the influence of directed blood flow. At the moment of diastole, the muscles of the cardiac cavities relax and fill with blood, the large anterior valvular valve closes the aortic cone, thereby preventing reflux into the aorta.
During systole, when the atrium and ventricles contract, the elements of the left atrioventricular orifice are compressed along thickened valve lines, which are held by the chordae. This prevents regurgitation and maintains normal hemodynamics in the systemic circulation.
Normal valve performance
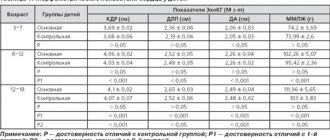
Echocardiographic examination (ultrasound of the heart) identifies average normal values:
- the diameter of the fibromuscular ring is 2.0-2.6 cm, the valve is up to 3 cm;
- MK area up to 6.5 cm2;
- the thickness of the valves is 1-2 mm;
- the movement of all doors is active and smooth;
- the surface is uniform and smooth;
- in the systole phase, the deflection of the elements into the ventricular cavity is no more than 1.5-2 mm;
- chords in the form of long, linear and thin fibers.
Diagnosis of heart valve diseases
After listening to the symptoms you describe and examining your medical record, the doctor will measure your pulse and blood pressure and listen to your heart using a stethoscope.
If your doctor suspects that you have a heart disease, he may ask you to undergo a series of special diagnostic tests that will help make an accurate diagnosis and prescribe the necessary treatment.
One of these research methods is a non-invasive method, i.e. which does not require any internal intervention.
Another type of research is invasive: with the help of instruments inserted into the body, which, as a rule, causes only minor inconvenience to the patient.
Chest X-ray
This test allows the doctor to obtain valuable information about the size of the heart, heart chambers and the condition of the lungs.
Electrocardiogram (ECG)
An electrocardiogram monitors the electrical current passing through the heart and stimulates the chambers to contract. An ECG is especially useful in diagnosing abnormal heart rhythms and rates.
These studies also show muscle enlargement or damage, and the presence of congestion on one side or another of the heart.
Echocardiogram (EchoCG)
This test is carried out using a “small” microphone placed on the surface of the chest, which emits high-frequency sound waves.
Sound waves are reflected back (hence the term "echo") from each layer of the heart wall and valves and then displayed on a monitor screen. The “echo” image from different points allows you to see a cross-section of the heart at the moment of its operation.
During the echo, the speed of blood flow is also recorded, the direction of blood movement is monitored: is the blood moving in the normal forward direction or is there a reverse movement (as in the case of valve insufficiency).
A narrowed (or stenotic) valve causes increased blood flow. The degree of valve stenosis is in many cases accurately determined by the increased blood flow velocity.
This test will not only show how the heart valves work, it will also provide useful and comprehensive information about the size of the heart chambers, as well as the thickness and function of the heart muscle.
Cardiac catheterization and angiogram
These tests are done by inserting a thin, hollow tube (catheter) through a vein or artery in the arm or groin area and into the chambers of the heart, using X-rays.
During catheterization, the pressure in the chambers of the heart is measured and the volume of blood in the bloodstream is determined.
Angiography consists of the injection of a radiopaque contrast agent, which is visible using X-rays and allows you to evaluate the work of the heart in pumping blood, the function of the valve and the patency of the arteries (coronary) that supply blood to the heart muscle.
Despite the fact that similar studies have been routinely carried out before, it is not at all necessary that they are needed in your case if the information obtained by echocardiography is complete and accurate.
In many cases, the only invasive test required before surgery is a coronary angiogram if it is determined that the patency of one or more arteries is impaired.
If there are blockages in the coronary arteries, the doctor will usually perform bypass surgery at the same time as heart valve surgery.
to the top of the page
Why does a defect form?
Anatomically, the valve is located between the left ventricle and the aorta. Normally it has a 3-leaf structure. This allows it to effectively perform its functions and prevents hemodynamic disturbances.
The formation of the main elements of the heart (aortic, tricuspid, pulmonary and mitral valves) occurs at 6–8 weeks of pregnancy. Accordingly, it is the course of this period that largely determines the normal formation of the baby’s organs. If exposed to aggressive agents at this time, proper embryogenesis may be disrupted with the appearance of heart disease. Such etiological factors include:
- Acute respiratory infections, bacterial infections. The most dangerous are measles rubella and cytomegalovirus.
- Bad habits: alcohol abuse, taking amphetamines, drugs, smoking.
- Burdened hereditary history.
- Severe course of the first trimester of pregnancy with symptoms of severe toxicosis, threat of miscarriage.
- Fetoplacental insufficiency.
- Emotional overload.
- HIV.
- Genetic diseases of the fetus - Marfan, Down, Ehlers-Danlos syndrome.
However, what exactly served as the trigger for the formation of heart disease in a child is difficult to say.
Heart valve surgery
Often heart defects do not manifest themselves for a long time, because the heart adapts to working under overload. In the case where the heart defect is “moderate” and does not lead to serious overload of the heart, in some cases they are limited to observation or drug therapy. But when the defect is severe, it must be treated surgically.
The following operations are performed on heart valves: reconstruction or complete replacement of a damaged valve.
Heart valve reconstruction
Sometimes during surgery it is possible to preserve the valve flaps and only correct their shape. This procedure is called valve repair.
.
Sometimes the shape of the valve can be restored by strengthening its base with threads, or by sewing a special ring to the base, while the valve’s own flaps are preserved. This procedure is called annuloplasty.
, it is possible only for the mitral and tricuspid valves.
Valve reconstruction can largely restore its function. For severe heart valve damage, valve replacement surgery may be the only treatment option. The results of these operations exceed the effect of drug therapy. Today, heart valve surgery can be performed on patients of any age group.
Access for operations on the aortic valve or on several valves simultaneously is made through an incision in the center of the sternum. When performing operations on the mitral valve, it is possible to use the “keyhole technique,” when surgical access is made through a small incision in the projection of the mitral valve: on the side and below the chest.
When it is impossible to save the leaflets of the native valve, or if they are preserved, there is a high probability of the defect returning and repeated surgery, the native valve is excised and implanted in its place
artificial
valve prosthesis
.
The most commonly performed surgeries are mitral valve reconstruction. In this case, the own valve is preserved - this is very important.
, Ross surgery is performed to treat aortic disease.
. The damaged aortic valve is replaced with the patient's own pulmonary valve, which is similar in structure, and an artificial prosthesis is implanted instead of the excised pulmonary valve.
When the aortic valve and aortic wall are damaged, it may be necessary to replace the ascending aorta with a valve-containing aortic graft
(sometimes called a conduit). In this case, not only the aortic valve is replaced, but also the adjacent ascending aorta.
Your attending physician will inform you about the possibility of reconstructive surgery on the heart valve in your case. In some cases, the question of the possibility of valve reconstruction is decided during the operation: if reconstruction is not possible, then an operation is performed to replace the damaged valve.
conclusions
Mitral valve stenosis, prolapse or insufficiency significantly impairs the patient’s quality of life. The severity of symptoms depends on the degree of hemodynamic impairment. Chronic progressive course increases the risk of disability with an unfavorable prognosis, and mortality when complications develop. When the defect is identified, all patients are prescribed treatment. Medications and drug regimens are less effective than minimally invasive surgery. Therapy is carried out in a cardiology hospital.
Source: cardiograf.com
Valves are:
casement
semilunar
The leaflet valves are located between the atrium and the ventricle. Valve leaflets are composed of endothelium. A chorda tendineum extends from each leaflet into the ventricle. The chorda tendineum attaches to the papillary muscles of the myocardium (muscle trabecula).
There are two flap valves:
tricuspid valve (TC), or tricuspid - has 3 leaflets and is located between the right atrium and the right ventricle (in the right atrioventricular orifice)
mitral valve (MK), or bicuspid - has 2 leaflets and is located between the left atrium and the left ventricle (in the left atrioventricular orifice)
The valves prevent blood from flowing back from the ventricles into the atria.
Regurgitation is the reverse flow of blood from the ventricles into the atria.
Semilunar valves
Semilunar valves consist of three valves that look like pockets. When the ventricles contract, the valves bend inside the arteries (AO and pulmonary trunk).
There are two semilunar valves:
aortic valve (AK) - located at the entrance to the Ao, between the left ventricle and the Ao
pulmonary valve (VV) - located at the entrance to the pulmonary trunk, between the right ventricle and the pulmonary trunk
Structure of the heart wall
The wall of the heart consists of 3 layers, each layer has its own name.
The endocardium is the inner layer of the heart. It consists of endothelium.
Myocardium is the middle layer. It consists of cardiac striated muscle tissue. It consists of cardiomyocytes connected by intercalated discs, due to which 2 atria and 2 ventricles contract simultaneously. The myocardium consists of 2 layers (atria) and 3 layers (ventricles).
The myocardium of the atria is thinner than that of the ventricles. The myocardium of the left ventricle is thicker than the right (since the BCC begins there).
The pericardial sac is the outer layer. It consists of 2 layers:
The epicardium - the inner layer of the bag - consists of squamous epithelium and fuses with the myocardium.
The pericardium, the outer layer of the bursa, consists of a single layer of squamous epithelium and connective tissue. Outside, the pericardium fuses with the tendon center of the diaphragm and the sternum.
Between the epicardium and the pericardium there is a small space - the pericardial cavity, filled with serous fluid. Its function is to prevent friction between the two layers of the pericardial sac.
PHYSIOLOGY OF THE HEART
Source: studopedia.ru
Treatment Options
If there is a bicuspid aortic valve of the heart with slight regurgitation, no complaints or abnormalities according to additional studies, then drug treatment is not prescribed.
The patient is given a number of general recommendations:
- elimination of physical overload;
- good dream;
- proper nutrition;
- daily walks in the fresh air;
- for teenagers and adults – refusal of coffee, nicotine, alcohol;
- For children who are bottle-fed, high-calorie formulas are selected.
Patients are required to undergo annual scheduled examinations, including cardiac ultrasound.
If there are clinical manifestations of a bicuspid aortic valve, drug support is prescribed:
- metabolic drugs;
- antiarrhythmic drugs;
- disaggregants;
- anticoagulants;
- diuretics;
- β-blockers.
Large regurgitation on the affected valve, rhythm disturbances, severe symptoms are indications for surgical treatment.
There are 2 options for operations:
- heart transplantation;
- valve replacement.
The second option is more preferable due to the patient’s minor trauma and rapid recovery.
Clinical manifestations
If the defect is mild, a newborn baby may have no symptoms of the disease. They appear as the child grows. Typical complaints associated with pathology of the bicuspid aortic valve in infants are:
- poor weight gain or progressive weight loss;
- frequent regurgitation, independent of food intake;
- the appearance of periodic bluishness of the skin;
- decreased number of urinations;
- lethargy.
For older children and adults it is common to:
- discomfort to the left of the sternum;
- shortness of breath, feeling of lack of air;
- poor tolerance to stress and physical activity;
- decreased performance, concentration;
- fast fatiguability;
- presyncope, fainting;
- dizziness;
- palpitations, interruptions in heart function.
With a well-compensated heart defect, there may be no complaints for many years.
The bicuspid valve may debut in such patients with severe complications - stroke, pulmonary embolism, fatal arrhythmias.
How is pathology diagnosed?
A doctor may suspect congenital heart disease in children and adults based on:
- Typical complaints.
- Anamnesis data.
- Results of the general examination. Auscultation of the heart plays a key role in identifying pathological murmurs and additional tones. Their listening point is located to the right of the sternum in the 2nd intercostal space.
The disease is confirmed and a final diagnosis is made only after an ultrasound of the heart - transthoracic or transesophageal.
Based on the results of the study, they determine where the defect is located, its degree, the presence/absence of regurgitation, and damage to other parts are determined.
Additionally, to assess the clinical picture and determine drug therapy, patients are advised to undergo:
- Cardiography;
- daily ECG monitoring;
- Ultrasound of the abdominal cavity;
- X-ray of the lungs.
Patients with a high degree of defect, a pronounced clinical picture and the need for surgical treatment are prescribed coronary angiography.