Publications in the media
Tricuspid valve stenosis is a narrowing of the tricuspid valve opening that prevents blood from flowing from the right atrium (RA) into the right ventricle (RV). Frequency • Severe tricuspid valve stenosis is observed in 14–15% of patients with heart defects • The ratio of men to women is 4:1.
Etiology • Rheumatism • Infectious endocarditis • Subendocardial fibroelastosis • Congenital anomalies (Ebstein's anomaly, etc.) • Idiopathic calcification • Myxoma of the right atrium • Secondary tumors of the right atrium (nephroblastoma sprouting from the inferior vena cava, metastases).
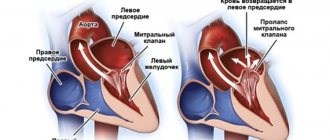
Pathophysiology • Hemodynamic abnormalities are similar to those of tricuspid regurgitation. The differences are that there are no changes in the pancreas, and stagnation in the systemic circulation occurs and progresses much faster • Since in the vast majority of cases, tricuspid stenosis is accompanied by insufficiency and defects of other valves, the general pathogenesis consists of the corresponding individual disorders • Based on the degree of narrowing of the valve opening, they are distinguished moderate (2.5–3 cm2), severe (1.5–2.5 cm2) and severe (less than 1.5 cm2) stenoses.
Clinical picture and diagnosis
• For complaints, see Tricuspid valve insufficiency.
• Valvular symptoms •• Strengthening of the first tone, the opening click of the tricuspid valve •• With sinus rhythm - fusiform low-frequency diastolic murmur (increases on inspiration) •• The intensity and duration of the murmur depend on the diastolic transtricuspid pressure gradient •• Auscultatory diagnosis of the defect is difficult due to sound phenomena associated with concomitant anomalies of other valves.
• For symptoms of circulatory failure in the systemic circle, see Tricuspid valve insufficiency.
• Symptoms of the underlying disease (rheumatism, myxoma of the heart).
Special studies
• ECG see Tricuspid valve insufficiency.
• Jugular venogram: increase in A-wave amplitude and gentle Y-decline.
• X-ray of the chest organs •• Bulging of the arch of the right atrium (with an isolated defect - without deviation of the contrasted esophagus) •• Dilation of the shadows of the vena cava •• Signs of concomitant lesions of other valves •• With a moderate isolated defect, there may be a normal x-ray picture.
• EchoCG •• Expansion of the cavity of the right atrium •• Expansion of the superior vena cava •• Fusion, deformation and thickening of the tricuspid valve leaflets, a decrease in the amplitude of their opening and dome-shaped protrusion in diastole •• In pulsed wave Doppler mode, the diastolic pressure gradient is determined •• Reduction in the area of the tricuspid orifice valves are calculated in Doppler mode (pressure gradient) and B-mode (the smallest value is taken as the basis for diagnosis) •• For candidates for surgical treatment, the internal diameter of the annulus fibrosus is measured •• Signs of other valvular or congenital anomalies •• Displacement of the annulus fibrosus and atrialization RV, as well as an increase in the amplitude of movement of the valves with Ebstein's anomaly •• Detection of space-occupying formations in RA tumors •• Transesophageal echocardiography is performed in all patients to exclude RA thrombosis and vegetations, even with a normal rhythm.
• Right heart catheterization •• Increased RA pressure, flattened Y-slope, steep X-slope, increased A-wave amplitude and transtricuspid diastolic pressure gradient •• In severe tricuspid stenosis, especially in combination with mitral stenosis and pulmonary hypertension, cardiac output low •• For tumors of the right heart, catheterization is contraindicated.
• Right atriography and coronary angiography. Performed when tricuspid stenosis is suspected, when echocardiography data is insufficient, as well as for diagnosing other valve defects and coronary artery disease.
TREATMENT
• Conservative therapy. Treatment of right ventricular failure: diuretics and venous vasodilators (use with caution as higher than normal CVP is required to maintain preload).
• Surgical treatment •• Indications ••• III degree stenosis with pronounced clinical manifestations ••• II degree stenosis when simultaneous cardiac intervention is necessary for other diseases •• Contraindications ••• Severe concomitant pathology that threatens the patient’s life ••• Terminal stage circulatory failure ••• The activity of the rheumatic process is not considered a contraindication to surgical treatment •• Methods of surgical treatment ••• Open commissurotomy or balloon valvuloplasty is performed if the valve apparatus is intact and with concomitant tricuspid insufficiency no higher than grade I ••• In other cases, valve replacement is performed biological prosthesis or, less commonly, mechanical ••• See also Tricuspid valve insufficiency.
For specific complications , see Tricuspid valve insufficiency.
For prognosis , see Tricuspid valve insufficiency.
Synonyms • Tricuspid valve stenosis • Right atrioventricular orifice stenosis • Tricuspid stenosis
Abbreviations • RV - right ventricle • RA - right atrium.
ICD-10 • I07 Rheumatic diseases of the tricuspid valve
Mitral valve stenosis - symptoms and treatment
Treatment tactics for mitral stenosis depend on its stage.
In stage I stenosis, patients are not indicated for surgical treatment, since compensatory mechanisms develop in the body. Compensation is supported by primary and secondary prevention of rheumatic fever.
The main task of primary prevention is to prevent the development of rheumatism. It involves the complete and timely elimination of streptococcal infections in sinusitis, rhinitis, sore throat and other diseases of the upper respiratory tract.
The goal of secondary prevention is to reduce the risk of re-exacerbation of rheumatism. It involves courses of bicillin prophylaxis (intramuscular injections of bicillin-5), observation by a rheumatologist, and the use of non-steroidal anti-inflammatory drugs in the event of colds and during various operations.
For primary and secondary prevention of rheumatism, it is important to follow the regimen. It consists of a healthy lifestyle, proper nutrition, exercise, absence of bad habits, good living conditions, timely visits to the dentist, medical supervision and treatment for colds.
In stage II stenosis, the indications for surgery are relative. Treatment options considered:
- closed mitral commissurotomy - an operation to widen the mitral valve, which is performed using a special dilator;
- reconstructive surgeries are valve-sparing surgeries in which valve function is restored using various suture technologies while preserving the valve leaflets and structures of the valve apparatus.
These operations make it possible to save patients' lives without leading to specific complications.
For stages III and IV of stenosis, surgical treatment is mandatory. Conservative therapy (taking cardiac glycosides and diuretics) brings only a short-term effect, since with an increase in physical activity, circulatory disorders still occur.
Closed mitral commissurotomy is indicated for patients with isolated mitral stenosis or re-fusion of the valve leaflets (restenosis) without gross changes in the valve structures, as well as with concomitant mitral regurgitation or grade I calcification. Mortality with this type of treatment is 0.5-1%. Repeated operations are performed in 35% of cases 10-15 years after the first surgical intervention [12].
In patients at high surgical risk, transcatheter balloon valvuloplasty is performed. It also aims to dilate the mitral valve. To do this, a percutaneous puncture of the common femoral vein is first made. Through it, the doctor inserts conductors and catheters into the right atrium. There, a puncture of the interatrial septum is performed, after which a balloon is inserted into the mitral valve ring and inflated [13].
Indications for reconstructive operations on the mitral valve are defects with predominant insufficiency without gross changes in the leaflets and structures of the valve apparatus, as well as the absence of calcification. Mortality after reconstructive surgery is 1.5-4%. Long-term survival rate is 90% [14].
In all other cases: valvular infective endocarditis, post-infarction defects, grade II or III calcification, the most effective operation is valve replacement with a mechanical or biological prosthesis. Mortality after such treatment ranges from 2-8%. The five-year survival rate of patients using modern types of artificial and biological prostheses is 75-90% [15].
Before any operation, the doctor must explain to the patient the course of the operation, anesthesia, possible risks and complications. After this, the patient signs consent for the operation. A few days before the planned intervention, drug therapy is carried out to stabilize the patient’s condition and prevent complications that may arise during or after surgical treatment. Hygienic treatment of the patient’s skin is also necessary: taking a shower, shaving surgical access sites. The patient should not eat food on the day before surgery.
After the operation, the patient is under observation in the intensive care unit. After stabilizing his condition and restoring the vital functions of the body, he is transferred to a specialized department under the supervision of the attending physician. At this time, the patient follows all recommendations for taking medications, activity and nutrition. With the help of a physical therapy doctor, the patient performs restorative exercises (breathing, motor) daily. The attending physician monitors the increase in the patient’s physical activity (metered walking), performs the necessary dressings and helps to recover psychologically.
After discharge, the patient must strictly follow all the doctor’s recommendations. It is necessary to be observed on an outpatient basis by a cardiologist and perform ECHO-CG annually. For patients with a mechanical heart valve, it is important to monitor such laboratory blood indicators as the INR (International Normalized Ratio) level. This is due to the use of warfarin, a blood thinning drug. Its target values should be in the range of 2-3.
Acquired heart disease - symptoms and treatment
There is no medicine that can reverse the process and restore the valve to its original state. With the help of medication, it is only possible to influence the cardiovascular system and reduce the risk of complications. In severe cases, surgical treatment methods are used.
Drug treatment
The goal of therapy is to eliminate the causes of circulatory failure, improve the functional state of the myocardium, restore normal blood circulation, microcirculation (transport of blood cells and substances to and from tissues) and prevent recurrent circulatory disorders. Treatment for chronic circulatory failure includes a complete balanced diet and drug therapy.
The main groups of drugs used for valve dysfunction:
1. ACE inhibitors (angiotensin-converting enzyme) - enalapril, lisinopril, ramipril, perindopril, fosinopril. The drugs block the conversion of the hormone angiotensin I to angiotensin II. Angiotensin II has a vasoconstrictor effect and causes a rapid increase in blood pressure. ACE inhibitors are used to treat hypertension and treat or prevent heart failure.
2. Beta blockers - carvedilol, bisoprolol, metoprolol. These drugs lower blood pressure and normalize heart rate. The action is caused by blocking beta-adrenergic receptors, which are responsible for the body's response to stress.
3. Mineralocorticoid receptor antagonists - spironolactone, eplerenone. The drugs lower blood pressure and have a diuretic effect, reducing fluid content in tissues.
There are different types of heart defects, and different combinations of drugs are used to treat each of them. Concomitant pathologies and individual characteristics of the patient are also taken into account.
For example, when congestion predominates, diuretics (furosemide, torsemide) are additionally prescribed, which reduce the volume of circulating blood, reducing congestion in the pulmonary and systemic circulation. If blood clots are present or there is a high risk of their occurrence, anticoagulants are used - drugs that reduce blood clotting (warfarin, rivaroxaban, dabigatran, apixaban).
Relatively recently, a new class of drugs was developed - angiotensin-neprilysin receptor inhibitors (sacubitril). Their main effect is to increase the amount of peptides cleaved by neprilysin. The drugs increase diuresis (urine volume), natriuresis (sodium excretion in the urine), cause relaxation of the myocardium and prevent processes of disruption of the structure and function of the heart.
If it is impossible to use beta blockers, it is recommended to replace them with If channel inhibitors (ivabradine), which also reduce the heart rate. If it is impossible to use ACE inhibitors, angiotensin receptor blockers (losartan, valsartan, candesartan, telmisartan, irbesartan, olmesartan) are used. They have properties similar to ACE inhibitors, but do not reduce the synthesis of angiotensin II, but block angiotensin receptors [6].
Surgery
If there are indications, the effectiveness of drug treatment is insufficient and there are no contraindications, surgical methods are used. Many patients are afraid of the need for heart surgery. In some cases, surgical methods do carry some risk, but there are fairly safe operations that are not open heart and without large incisions. Such operations include balloon commissurotomy for mitral valve stenosis. The method consists of widening the valve using a catheter passed through the artery.
Before surgery, the necessary laboratory and instrumental studies are carried out and the patient’s condition is stabilized with medications. When preparing for surgery, it is important to reduce shortness of breath, swelling, and normalize pulse and blood pressure.
A common surgical method is artificial or biological valve replacement. There are also valve-sparing operations, which involve plastic surgery of a damaged valve.
Surgical treatment significantly improves the quality of life, however, after surgery, medication continues, but is adjusted if necessary. In addition, after certain operations, such as artificial valve replacement, anticoagulant therapy is constantly taken. The drugs are necessary because the risk of thromboembolic complications (blockage of arteries with blood clots) increases [5].