What it is
Mitral valve prolapse (hereinafter referred to as MVP) is the most common valvular pathology of the heart.
The disease affects approximately 2.5% of the world's population. It is often found in children and adolescents. The predominant number of patients are women and girls. MVP is distinguished separately from valvular heart defects for two reasons. Firstly, the anomaly has a different nature of occurrence. Secondly, unlike heart defects, this pathology is benign, but can also have unpleasant consequences. Often a person does not know about its presence: MVP becomes an “accidental finding” during a medical examination or examination for another disease.
To understand the essence of this disease, it is important to understand the process of valve operation. The human heart has 4 cavities, or chambers. Normally, blood circulates in only one direction: from the atria to the ventricles, then to the large vessels (aorta and pulmonary artery). This is possible thanks to the synchronous operation of the valves, which open and close at the right time. Closed valves prevent regurgitation - the direction of blood flow in the opposite direction.
With MVP, its main function is disrupted. During the systole phase, when the left ventricle contracts, the valve leaflets cannot withstand the blood pressure and begin to protrude into the cavity of the left atrium. The main problem is that some of the blood returns to the left atrium. This is called regurgitation. All the ensuing adverse effects of MVP are associated with this process. Severe regurgitation can lead to disability.
Heart valve surgery
Often heart defects do not manifest themselves for a long time, because the heart adapts to working under overload. In the case where the heart defect is “moderate” and does not lead to serious overload of the heart, in some cases they are limited to observation or drug therapy. But when the defect is severe, it must be treated surgically.
The following operations are performed on heart valves: reconstruction or complete replacement of a damaged valve.
Heart valve reconstruction
Sometimes during surgery it is possible to preserve the valve flaps and only correct their shape. This procedure is called valve repair.
.
Sometimes the shape of the valve can be restored by strengthening its base with threads, or by sewing a special ring to the base, while the valve’s own flaps are preserved. This procedure is called annuloplasty.
, it is possible only for the mitral and tricuspid valves.
Valve reconstruction can largely restore its function. For severe heart valve damage, valve replacement surgery may be the only treatment option. The results of these operations exceed the effect of drug therapy. Today, heart valve surgery can be performed on patients of any age group.
Access for operations on the aortic valve or on several valves simultaneously is made through an incision in the center of the sternum. When performing operations on the mitral valve, it is possible to use the “keyhole technique,” when surgical access is made through a small incision in the projection of the mitral valve: on the side and below the chest.
When it is impossible to save the leaflets of the native valve, or if they are preserved, there is a high probability of the defect returning and repeated surgery, the native valve is excised and implanted in its place
artificial
valve prosthesis
.
The most commonly performed surgeries are mitral valve reconstruction. In this case, the own valve is preserved - this is very important.
, Ross surgery is performed to treat aortic disease.
. The damaged aortic valve is replaced with the patient's own pulmonary valve, which is similar in structure, and an artificial prosthesis is implanted instead of the excised pulmonary valve.
When the aortic valve and aortic wall are damaged, it may be necessary to replace the ascending aorta with a valve-containing aortic graft
(sometimes called a conduit). In this case, not only the aortic valve is replaced, but also the adjacent ascending aorta.
Your attending physician will inform you about the possibility of reconstructive surgery on the heart valve in your case. In some cases, the question of the possibility of valve reconstruction is decided during the operation: if reconstruction is not possible, then an operation is performed to replace the damaged valve.
Causes of the defect
Based on its origin, mitral valve prolapse is of two types:
- primary;
- secondary.
Primary MVP is caused by genetic defects. And although the gene mutations responsible for the development of the pathology have not yet been precisely determined, there is evidence of the hereditary nature of the disease in the form of frequent cases of prolapse in close relatives.
Therefore, if one of your parents or siblings was diagnosed with MVP, there is a high probability that you have it too.
Primary prolapse is divided into types:
- MVP itself as an independent disease;
- MVP as a manifestation of connective tissue development disorders.
The latter refers to hereditary diseases caused by a defect in the formation of collagen protein. Such diseases include Marfan and Ehlers-Danlos syndromes, as well as common undifferentiated connective tissue dysplasias. In addition to MVP, these pathologies are characterized by different clinical manifestations:
- increased vulnerability and hyperextensibility of the skin;
- frequent subluxations and dislocations;
- hypermobility of joints - a person is able to bend his elbows and knees in the opposite direction, touch his thumb to his forearm, close his palms, placing his hands behind his back;
- chest deformities – keeled, funnel-shaped;
- curvature of the spine - scoliosis, kyphosis;
- flat feet;
- early myopia;
- aneurysms of the interatrial septum and aorta;
- early development of varicose veins of the lower extremities, hemorrhoids;
- diaphragmatic and vertebral hernias;
- frequent nosebleeds;
- prolapse of internal organs - stomach (gastroptosis), intestines (colonoptosis), kidneys (nephroptosis).
Secondary prolapse, as the name suggests, develops against the background of other diseases. MVP occurs due to expansion of the cavities of the heart, stretching of the fibrous ring of the valve, due to wrinkling, inflammation of the valve leaflets or the deposition of calcium salts in them.
Causes of secondary prolapse:
- cardiac ischemia;
- cardiomyopathy;
- myocarditis;
- congenital and acquired heart defects;
- chronic rheumatic heart disease.
Separately, I would like to highlight the “harmless or physiological” MVP, which develops due to the immaturity of the valve itself (fibrous ring, leaflets) and the subvalvular apparatus (tendon filaments or chords and papillary muscles). During ventricular systole, the papillary muscles contract and tighten the chordae, which keep the valve leaflets from sagging.
It often happens that in a growing child’s body, some heart structures develop earlier, while others develop later.
Consequences of this:
- the formation of too long valves or chords;
- large diameter of the fibrous ring;
- insufficient contraction of the papillary muscles.
This can lead to prolapse of the mitral valve leaflets. However, physiological prolapse is called “harmless” for good reason. By the age of 18–20, all structures of the heart have fully matured, and the valve functions as in a healthy person.
Frequent symptoms
Most people with “harmless” mitral valve prolapse, especially children and adolescents, have an asymptomatic course of the disease and nothing bothers them. Sometimes patients complain only of minor chest discomfort. I would like to note that the clinical picture may not correspond to the degree of pathology.
Symptoms of mitral valve prolapse:
- pain in the left side of the chest or behind the sternum: stabbing, pressing, squeezing, moderate intensity. The duration varies from a few seconds to a day. Pain can occur either during a strong experience or performing physical exercise, or spontaneously, for no apparent reason. Often the unpleasant sensation is accompanied by a feeling of lack of air, the appearance of cold sticky sweat, anxiety and even fear of death;
- dizziness due to low blood pressure;
- rapid heartbeat, sensations of “interruptions, rolling, freezing” in the chest;
- frequent pre-fainting conditions, in which a person experiences a feeling of lightheadedness and nausea, accompanied by flashing spots before the eyes and blurred vision;
- with severe and prolonged mitral regurgitation, signs of congestive heart failure are added - difficulty breathing, rapid onset of fatigue, swelling in the legs, especially in the evening, heaviness in the right side due to an enlarged liver.
Also, in people with mitral valve prolapse, often due to hereditary connective tissue disorders, I observe symptoms of autonomic dysfunction:
- constant pressure changes;
- fainting;
- increased sweating;
- neurotic disorders - such patients are usually anxious and suspicious, suffer from various phobias, hypochondriacal and obsessive-compulsive neuroses, they often invent non-existent diseases;
- “chilliness” and cold fingers and toes;
- increased sensitivity to cold;
- vegetative crises, better known as panic attacks.
Types and degrees of mitral valve prolapse
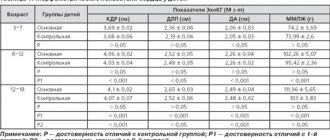
Echocardiography (ultrasound of the heart) is the main research method for diagnosing MVP. With its help, the severity of prolapse is assessed: the degree of prolapse of the valves and regurgitation. Prolapse refers to the extent to which the valve leaflets bend into the cavity of the left atrium.
Table. Classification of mitral valve prolapse
| PMC degree | Prolapse distance |
| 1st degree | From 3 to 6 mm |
| 2nd degree | 6 to 9 mm |
| 3rd degree | More than 9 mm |
There are pathologies:
- with regurgitation;
- without regurgitation.
The disorder is also assessed by ultrasound of the heart, but in Doppler mode.
There are 4 degrees:
- 1st degree - reverse blood flow penetrates into the cavity of the left atrium at a distance of up to 20 mm;
- 2nd degree – penetration to the middle of the atrium;
- 3rd degree - blood flow passes more than half of the atrium;
- Grade 4 – regurgitation to the opposite wall of the atrium.
Approximately 30% of people with MVP, which developed against the background of hereditary connective tissue diseases, additionally have tricuspid valve prolapse, and 4-5% have aortic valve prolapse.
PMC: prognosis and prevention.
In general, the prognosis for MVP is quite favorable, the main thing is constant clinical monitoring of the patient to determine the degree of mitral valve insufficiency. Often, mitral valve prolapse does not affect physical activity (among people with MVP there are professional athletes, dancers, etc.), however, there are signs, the identification of which is an “alarm bell” and leads to a ban on active anaerobic exercise:
- long QT syndrome;
- Marfan syndrome;
- history of loss of consciousness (without reason);
- left ventricular dysfunction;
- attacks of atrial tachycardia;
- severe mitral regurgitation.
All patients with MVP need to monitor their health, avoid frequent infections and be sure to treat them if they occur.
Prevention of MVP is the absence of adverse effects on the health of the pregnant woman and the fetus developing in the womb, timely diagnosis and treatment of diseases that damage the valvular apparatus of the heart.
Do not under any circumstances neglect the diagnosis of MVP and always strictly follow the doctor’s recommendations!
Diagnosis criteria
To make an accurate diagnosis, I use specially developed criteria:
- The main ones.
- Additional.
- Non-specific.
The first include:
- late systolic click/click, late systolic murmur at the apex of the heart on auscultation. Sometimes, in order to better listen to the noise, I resort to some tricks: I ask the patient to do 10 squats or lie on his left side;
- displacement of the leaflets at the time of ventricular systole, prolapse (bending) of the leaflets more than 3 mm.
Additional criteria:
- neurotic disorders;
- the presence of MVP in close relatives (father, mother, grandparents, siblings);
- The patient’s appearance is tall, thin, long arms and legs, malocclusion, deformities of the chest or spine.
Non-specific criteria include:
- patient complaints - pain in the heart, difficulty breathing, rapid heartbeat, panic attacks;
- changes on the ECG film - negative T wave in leads II, III, aVF, frequent extrasystoles and slowing of intraventricular conduction.
The presence of 2 main criteria or one main and 2 additional criteria allows one to reliably make a diagnosis of mitral valve prolapse. In addition, these criteria help to carry out differential diagnosis, that is, to distinguish MVP from acquired heart defects.
Forecast
Favorable in the first stage of mitral valve prolapse. Surgery is not always necessary. Survival rate is maximum and is almost 100%. With rapid progression of the disease, the probability is slightly lower. It correlates with the speed of the violation.
Negative factors significantly worsen the prognosis, first for the course of prolapse, and then for life in general.
Among the unfavorable points:
- Bad family history. There is partial genetic causation. At least predispositions.
- The presence of somatic concomitant pathologies.
- Poor response to treatment.
- Impossibility of surgical intervention when indicated.
- Age over 50 years.
- Several heart defects at the same time.
- Genetic nature of the deviation.
- Being male.
The more negative aspects, the worse the prognosis for the development of the condition.
- Prolapse of the anterior leaflet of the mitral valve, grade 1
Is treatment required?
Factors that help determine whether treatment for mitral valve prolapse is necessary:
- symptoms;
- degree of prolapse and regurgitation;
- presence or absence of complications.
If a person has a hemodynamically insignificant grade 1 MVP and does not experience any discomfort, then treatment is not required. For such people, I only recommend giving up smoking, excessive coffee consumption, and undergoing regular examinations with a cardiologist and echocardiography (once every 3 years).
Mitral valve prolapse of the 1st degree with regurgitation of the 1st degree and mitral valve prolapse of the 2nd degree, and even more so signs of rhythm disturbances and circulatory failure, are an indication for the prescription of specific drug therapy: drugs from the group of beta-blockers (Metoprolol, Bisoprolol).
These pharmacological drugs cope well with pain, normalize heart rate and blood pressure levels. They slow down the progression of regurgitation and prevent dangerous tachyarrhythmias. Also, with the help of beta-blockers, it is possible to compensate for the effects of heart failure. If they fail, then I use calcium channel blockers (Diltiazem, Verapamil).
However, it is important to remember that there are contraindications to the use of these medications:
- severe bradycardia, i.e. slow heart rate (less than 55 beats per minute);
- atrioventricular blockades of 2 and 3 degrees;
- low blood pressure (below 100 mmHg).
“Biogenic stimulants” help in the fight against hypotension:
- Eleutherococcus;
- ginseng;
- lemongrass
To treat anxiety, I first prescribe herbal sedatives - valerian, motherwort, hawthorn. For severe neurotic disorders and for the prevention of panic attacks, stronger drugs are needed (Diazepam, Phenazepam). To get a prescription for them, I refer patients for a consultation with a neurologist, psychiatrist or psychotherapist.
When chronic heart failure develops, I prescribe ACE inhibitors (Perindopril) and potassium-sparing diuretics (Spironolactone). For severe heart rhythm disturbances that cause deterioration in health, I use antiarrhythmic drugs (Amiodarone, Propafenone). To prevent blood clots in atrial fibrillation, I use anticoagulants (Warfarin).
In the later stages of prolapse with grade 4 mitral regurgitation or severe circulatory failure, surgery is required - plastic surgery or valve replacement.
Separately, it is worth considering the issue of pregnancy during MVP. Drug treatment is not fundamentally different. If severe regurgitation occurs (grade 3–4) and serious complications develop, further actions depend on the timing:
- up to 22 weeks - medical termination of pregnancy or vacuum aspiration;
- after 22 weeks - caesarean section and placing the child in a special incubator to preserve life.
Subsequently, surgical treatment of prolapse is performed. Such radical measures are due to the high danger for the mother and fetus: death is likely.
Diagnosis of heart valve diseases
After listening to the symptoms you describe and examining your medical record, the doctor will measure your pulse and blood pressure and listen to your heart using a stethoscope.
If your doctor suspects that you have a heart disease, he may ask you to undergo a series of special diagnostic tests that will help make an accurate diagnosis and prescribe the necessary treatment.
One of these research methods is a non-invasive method, i.e. which does not require any internal intervention.
Another type of research is invasive: with the help of instruments inserted into the body, which, as a rule, causes only minor inconvenience to the patient.
Chest X-ray
This test allows the doctor to obtain valuable information about the size of the heart, heart chambers and the condition of the lungs.
Electrocardiogram (ECG)
An electrocardiogram monitors the electrical current passing through the heart and stimulates the chambers to contract. An ECG is especially useful in diagnosing abnormal heart rhythms and rates.
These studies also show muscle enlargement or damage, and the presence of congestion on one side or another of the heart.
Echocardiogram (EchoCG)
This test is carried out using a “small” microphone placed on the surface of the chest, which emits high-frequency sound waves.
Sound waves are reflected back (hence the term "echo") from each layer of the heart wall and valves and then displayed on a monitor screen. The “echo” image from different points allows you to see a cross-section of the heart at the moment of its operation.
During the echo, the speed of blood flow is also recorded, the direction of blood movement is monitored: is the blood moving in the normal forward direction or is there a reverse movement (as in the case of valve insufficiency).
A narrowed (or stenotic) valve causes increased blood flow. The degree of valve stenosis is in many cases accurately determined by the increased blood flow velocity.
This test will not only show how the heart valves work, it will also provide useful and comprehensive information about the size of the heart chambers, as well as the thickness and function of the heart muscle.
Cardiac catheterization and angiogram
These tests are done by inserting a thin, hollow tube (catheter) through a vein or artery in the arm or groin area and into the chambers of the heart, using X-rays.
During catheterization, the pressure in the chambers of the heart is measured and the volume of blood in the bloodstream is determined.
Angiography consists of the injection of a radiopaque contrast agent, which is visible using X-rays and allows you to evaluate the work of the heart in pumping blood, the function of the valve and the patency of the arteries (coronary) that supply blood to the heart muscle.
Despite the fact that similar studies have been routinely carried out before, it is not at all necessary that they are needed in your case if the information obtained by echocardiography is complete and accurate.
In many cases, the only invasive test required before surgery is a coronary angiogram if it is determined that the patency of one or more arteries is impaired.
If there are blockages in the coronary arteries, the doctor will usually perform bypass surgery at the same time as heart valve surgery.
to the top of the page
Does the prognosis change for people with MVP?
Mitral valve prolapse is a benign pathology.
But the forecast directly depends on the following factors:
- degree of prolapse;
- regurgitation is present or absent;
- Are there any complications?
With minor prolapse (1st degree without regurgitation or with 1st degree regurgitation), the prognosis is favorable. This pathology does not affect life expectancy.
For prolapse with 2nd degree regurgitation, in addition to taking medications, it is important for patients to follow a restrictive regimen. For example, boxing, weightlifting, and professional running are contraindicated for patients. Young people have restrictions on their suitability for military service. At the military medical commission, depending on the presence of complications, they are assigned categories “B”, “C”, and “D”.
Possible and negative consequences
Despite its apparent harmlessness, mitral valve prolapse is dangerous due to complications that can become a real threat to the patient’s life.
Adverse effects of MVP include:
- chronic heart failure - due to regurgitation, some of the blood does not enter the aorta, so the left ventricle is forced to compensatory hypertrophy (thicken). Over time, this will lead to its dysfunction and deterioration of blood circulation throughout the body;
- heart rhythm disturbances (atrial fibrillation, prolongation of the QT interval, paroxysmal supraventricular and ventricular tachycardia). Regurgitation leads to stretching and expansion of the cavity of the left atrium, in the wall of which foci of pathological electrical activity may appear;
- ischemic stroke - a vortex flow of blood is created in the dilated cavity of the left atrium, which contributes to its thickening and the formation of blood clots;
- acute mitral regurgitation - with a pronounced degree of prolapse and regurgitation, the tendon threads that are attached to the valves are strongly stretched. As a result, their rupture and sudden overload of the parts of the heart located on the left are possible;
- infective endocarditis - during some medical procedures (tooth extraction, catheter installation, bronchoscopy), a small amount of bacteria enters the general bloodstream. With prolapse, they can settle on the valve flaps and begin to multiply. To prevent this, people with MVP are advised to take antibiotics before procedures.
These complications can quickly lead to the death of the patient.
Acquired heart defects (AHD)
Heart valve defects
Valvular heart disease is characterized by damage or defect of one of the four heart valves: mitral, aortic, tricuspid or pulmonary.
The mitral and tricuspid valves control the flow of blood between the atria and ventricles (the upper and lower chambers of the heart). The pulmonary valve controls the flow of blood from the heart to the lungs, and the aortic valve regulates the blood flow between the heart and the aorta, and therefore the blood vessels to the rest of the body. With normal heart valve function, blood flows with the proper force in the right direction at the right time.
With a heart defect, the function of the valve is impaired; it can become too narrow (stenosis), which is why it does not open completely, or expand and cannot close completely (insufficiency). A narrowed valve prevents blood from flowing out of the chamber of the heart, while when it fails, the blood flows back into the chamber from which it previously came out. Impaired valve function leads to enlargement and thickening of the heart muscle, reducing its elasticity and efficiency.
The most common defects are the mitral and aortic valves.
The severity of heart disease varies. In mild cases there may be no symptoms, but in advanced cases the defect can lead to congestive heart failure and other complications. Treatment depends on the extent of the disease.
Causes of heart valve defects
There are many reasons. Some of them are present at birth (congenital), while others can be acquired later in life:
- aging of valves: heart valve tissue can degrade with age due to atherosclerosis, lose elasticity and become hard;
- rheumatism;
- bacterial endocarditis;
- high blood pressure;
- myocardial infarction;
- heart tumors
- systemic diseases (rheumatoid arthritis, systemic lupus erythematosus, syphilis);
- radiation therapy used to treat cancer.
Symptoms that may appear due to heart valve disease
Symptoms of heart disease can occur suddenly, depending on how quickly the disease progresses. When the disease progresses slowly, your heart may adjust and you may not notice the onset of any symptoms. It is important to understand that the severity of symptoms is not equivalent to severe heart valve disease and, conversely, symptoms may be completely absent in cases of severe heart valve disease.
Symptoms of heart disease include:
- Shortness of breath during exercise, fatigue
- Swelling of the extremities, rapid weight gain due to fluid accumulation
- Palpitations or irregular heartbeat
- Chest pain
- Dizziness or fainting
- Fever (if the valve is infected)
To identify and treat heart valve diseases, correct and timely diagnosis is important.
Diagnosis of defects
Valvular heart disease can be detected by listening to characteristic sounds known as heart murmurs.
To fully diagnose the defect, you need to undergo one or more of the following studies:
- An electrocardiogram (ECG) shows the heart's electrical activity, regularity of heartbeats, thickening (hypertrophy), and damage to the heart muscle from coronary artery disease.
- A chest x-ray shows enlargement of the heart chambers due to dysfunction of the heart valves.
- Echocardiogram (EchoCG) is the gold standard in modern diagnostics. In an echocardiogram, sound waves bouncing off the heart are recorded and converted into images. The scans can reveal abnormal size, shape, and movement of the heart and valve dysfunction.
- Coronary angiography, which involves inserting a catheter into the heart to assess the condition of the vessels supplying the heart.
Mitral valve defects
There are three types of mitral valve dysfunction:
- Mitral valve prolapse is when both valve leaflets are enlarged and bulging, preventing them from closing evenly.
- Insufficiency is when the valve leaflets do not close tightly, causing blood to leak back into the left atrium of the heart. Deficiency can occur suddenly (acute) or, more often, gradually over time (chronic). Acute mitral valve regurgitation is often caused by damage to the heart, such as a heart attack or infective endocarditis.
There are many reasons why chronic mitral valve insufficiency can develop. Symptoms include fatigue, shortness of breath on exertion and while lying down, and irregular heartbeat.
- Stenosis—the mitral valve leaflets thicken, become rigid, and may even fuse together. Because of this, the valve opening narrows. Among adult patients, stenosis is more common in women, and the main cause is rheumatism. Symptoms include shortness of breath on exertion, swelling of the lower extremities, and cardiac arrhythmias. In some patients, clots (thrombi) form in the left atrium. These clots can travel through blood vessels and damage the brain, spleen, or kidneys.
Aortic valve defects
Aortic valve regurgitation occurs when the valve leaflets do not close and blood flows back into the left ventricle of the heart. A patient may have significant aortic regurgitation for many years without developing significant symptoms. Signs of the disease include palpitations, shortness of breath on exertion or while lying down (there may be sudden severe shortness of breath in the middle of the night), chest pain.
Aortic valve stenosis affects men more often than women. This is a condition where the valves thicken, become stiff and fuse together, narrowing the valve and preventing the normal flow of blood from the heart to the aorta and the rest of the body. Aortic valve stenosis usually does not cause symptoms until the valve opening has narrowed to about one-third of normal size. Symptoms include shortness of breath on exertion, chest pain, and fainting.
Tricuspid valve insufficiency
This is a heart defect characterized by incomplete closure of the tricuspid valve leaflets and the reverse flow of blood from the right ventricle into the right atrium.
Damage to the tricuspid valve, like other heart valves, can be caused by rheumatism, myxomatosis, infective endocarditis, or chest trauma.
Tricuspid valve insufficiency may also not be associated with damage to the valve itself, but may arise as a result of a long course of mitral and aortic defects, in the absence or improper treatment of them.
Treatment of heart valve defects
Treatment for heart valve disease will depend on the type and severity of the condition and may include medication or surgery.
If the heart defect is significant and medications do not help, surgery is performed to repair or replace the heart valve. Currently, heart valve surgery strives to perform valve-sparing operations. Thanks to improvements in reconstructive surgery techniques, it is possible to restore the valve even with infective endocarditis. In other cases, the valve is replaced with an artificial prosthesis.
Artificial heart valves
Artificial heart valves have improved significantly since their invention, and cardiac surgeons now have prostheses that can perform the function of their own valve as closely as possible.
Depending on the composition, artificial heart valves can be mechanical or biological. Mechanical valves are made entirely of synthetic materials, their advantages are strength, durability and wear resistance. The disadvantage is the need for lifelong use of anticoagulants (blood thinners) to prevent the formation of blood clots.
Artificial heart prostheses
Biological valves are made from animal heart tissue and treated with special solutions that increase wear resistance and prevent immune rejection after implantation. The advantages of biological prostheses are that there is no need for lifelong use of anticoagulants. Disadvantage: rapid wear, limited age of the patient. Biological prostheses are recommended for patients over 70 years of age; their service life is about 10-15 years.
Heart surgery
In most cases, the surgeon makes an incision in the middle of the sternum to reach the heart, uses a heart-lung machine to circulate blood throughout the body during surgery, stops and opens the heart to reach the diseased valve, then repairs or replaces the valve.
Heart valve surgery is also performed through a small incision on the right side of the chest using video support.
Patients with aortic stenosis can undergo aortic valve replacement with a biological prosthesis through the femoral artery or the apex of the heart - without cutting the sternum and stopping the heart. This operation is performed on older patients at high risk of standard open heart surgery. In this case, only biological prostheses are implanted.
After heart surgery
The World Health Organization (WHO) has defined health as not only the absence of disease and illness, but also the presence of physical, mental and social well-being. The goal of heart surgery is not only to prolong life, but also to improve functional mobility and quality of life.
Open heart surgery is a major procedure and requires time to fully recover. It depends on the age and general health of the person, as well as the complexity of the operation.
If you seek surgical help in a timely manner, it is possible to avoid postoperative complications and go through a short recovery path in almost 100% of cases.
During the first two weeks the patient feels tired and weak, the general condition gradually recovers over the next month. During this period, you need to limit heavy physical activity and give up sports. You need to leave the house at least 2 times a day for a short walk and try to increase your load a little every day. The sternum will heal completely within two months, after which it will be possible to return to normal household activities.
For many patients, returning home after heart surgery is a great relief, but for some it can be quite frightening. Follow the recommendations of your doctor, take prescribed medications on time, the duration and quality of your life depends on this.
Expert advice: treatment of MVP for connective tissue dysplasia
People suffering from hereditary connective tissue disorders have a magnesium deficiency. This microelement promotes the formation of collagen fibers, and consequently the strengthening of connective tissue. Therefore, I recommend that such patients include foods rich in magnesium in their diet: oatmeal, bananas, nuts, buckwheat and others. It is also worth taking additional dietary supplements: Magne B6, Magnerot. To improve magnesium absorption, you can add ascorbic acid.
Case study: a woman with arrhythmias and prolapse
I would like to present to you a case of arrhythmia caused by mitral valve prolapse.
A 38-year-old woman approached me. For a long time, she was worried about “interruptions in the heart,” an irregular pulse, as well as episodes of rapid heartbeat, during which her well-being significantly worsened, which manifested itself in the form of nausea and dizziness. During the last such attack, the woman fainted, which is why she got scared and decided to turn to me. During the general examination, the patient’s thinness and tall stature were striking. During the examination, it was possible to note hypermobility of the elbow and wrist joints. The woman also said that as a child she often had dislocations in her arm joints. I ordered Holter ECG monitoring and echocardiography, which showed QT prolongation, episodes of torsade de pointes (TdP), and leaflet prolapse of 7 mm without signs of regurgitation. Based on the results, I made a diagnosis: grade 2 mitral valve prolapse without regurgitation with complications (prolonged QT interval, PVT, CHF class 0). I prescribed Bisoprolol (1 tablet once a day) and Magne B6 (2 tablets 3 times a day). I also provided the patient with a list of foods high in magnesium.
When taken again after 3 months, the woman noted a significant improvement: her pulse returned to normal and the attacks stopped. And the ECG showed no signs of heart rhythm disturbances.
Nutrition
The diagnosis of Barlow's disease requires the patient to reconsider his habits and lifestyle. To avoid excessive stress, it is necessary to avoid the abuse of alcohol and caffeine, avoid smoking, and intense physical exercise.
The cardiovascular system is negatively affected by excess fat and salt. If you have MVP, you should avoid or minimize the consumption of fatty meat dishes, store-bought confectionery, smoked meats, marinades, fatty and hot sauces, and snacks with a high salt content. The choice of products for MVP is quite wide. The body should receive a sufficient amount of potassium and magnesium and vitamins. The optimal diet is one that includes lean meat, fresh and baked vegetables, fruits, vegetable oils, fish and seafood, nuts, milk and low-fat dairy products, and cereals. Instead of baked goods and industrially produced flour products, you should eat bread made from wholemeal flour.
Honey, dried apricots, prunes, raisins, dates are suitable as a dessert. It is better to drink tea and coffee with milk. Sources of heart-healthy magnesium include almonds, oatmeal, cashews, pumpkin seeds, and buckwheat. Potassium is found in dried apricots, raisins, beans, pumpkin and flax seeds, bananas, and potatoes.