Despite improvements in the diagnosis and treatment of arterial hypertension (AH), there is an increase in morbidity and mortality associated with this disease worldwide. The connection between blood pressure (BP) and the risk of cardiovascular diseases has been proven by numerous epidemiological studies conducted in various countries around the world, including Russia. The prevalence of hypertension is above 140/90 mmHg. among the Russian population is quite high: 31–39.2% of men aged 18–74 years and 37–41.1% of women [1]. The structure is dominated by mild and moderate hypertension, with significant growth observed in 40-60 years, which requires special attention to this age group [1].
In general, the data obtained indicate a high prevalence of hypertension in the Russian population, poor awareness of patients about the presence of the disease (especially among men), insufficient prescription of drug therapy for patients with hypertension and its catastrophically low effectiveness [2].
In the Republic of Uzbekistan, as in all countries, hypertension remains one of the pressing problems. This is confirmed by a one-time epidemiological study of the population aged 20 to 79 years in one of the districts of Tashkent. The prevalence of hypertension in the population was 35.7% (28.1% among men and 40.6% among women). There was a significant increase in the prevalence of hypertension with age: from 8.2% at the age of 20-29 years to 71.9% at the age of 70 years or more. The most common degree of hypertension in the study population, regardless of gender, was 66.2% of men and 60% of women; II degree - 16.2% of men and 25.2% of women; III degree - 17.6% of men and 14.8% of women [3].
People with high blood pressure have a significantly higher risk of stroke, coronary artery disease (CHD), other heart diseases, and kidney failure. Effective control of hypertension involves not only the correctness of medication prescriptions (drug selection, dose, regimen, etc.), but also the correction of the main risk factors that are closely related to the patient’s behavioral habits [4]. Most people with hypertension have unfavorable risk factors that negatively affect the prognosis of the development and course of the disease. Only about 7-10% of patients with hypertension are under medical supervision (dispensary observation), however, even in these patients, high levels of risk factors often remain and target blood pressure is not achieved, which is unfavorable for the prognosis [5, 6].
Numerous studies [2, 7—9] of the reasons for inadequate control of hypertension in real practice have shown that the main obstacle to improving the quality of preventive medical care is the low adherence of patients to fulfilling medical prescriptions. Scientific research in recent years [5-7, 9-12] has shown that one of the main methods that increases the completeness and accuracy of medical prescriptions is patient education. The condition for organizing schools requires the presence of trained personnel and methodological support in the medical institution [13]. Patient education allows you to expand the doctor’s sphere of influence from disease treatment to prevention. With this approach, medical control over the disease is complemented by control of ill health factors caused by the patient’s lifestyle, habits, and behavioral characteristics that affect health and the course of the disease [10, 11, 13].
Primary and secondary prevention of cardiovascular diseases are based on measures aimed at correcting the main risk factors - low physical activity, obesity, lipid disorders, high blood pressure, smoking [14]. Great importance is attached to increasing the educational level of patients with essential hypertension (HD) to improve their awareness and active participation in the diagnostic and treatment process [15, 16]. At the same time, achieving agreement between the doctor and the patient becomes one of the decisive values in the successful treatment of hypertension and the prevention of its complications, especially at the outpatient stage [17-19]. Participation of patients with hypertension in an educational program (training in schools) should become an integral part of measures for long-term prevention of cardiovascular complications [14].
The Health School helps each patient identify individual priorities, which is important for maintaining intentions to improve behavioral habits. It is schools for patients that make it possible to use not only informational, but also motivational learning technologies, implement psychological approaches to the formation of motivation in practice, and provide the social support so necessary for many patients. It is, in essence, a technology of group preventive counseling, the success of which is facilitated by a trusting atmosphere of communication between the doctor and the patient, mutual understanding and a sense of empathy, as well as effective feedback (the ability to listen, discuss, clearly explain the goals of training, etc.). As a rule, all preventive measures for patients are associated with certain restrictions or efforts (for example, controlling the energy composition of food or quitting smoking, etc.). At the same time, advice is perceived better and is more convincing if it is given with an emphasis on positive associations, does not contain difficult, cumbersome recommendations and is not perceived by patients as something unnatural for them, requiring effort, restrictions in action and additional means. It is advisable to accompany the advice with written recommendations and reminders [4].
Currently, experience has already been accumulated in assessing the effectiveness of health schools in various groups of patients with hypertension and in various organizational models of activity. Thus, training of patients who are registered at the local dispensary [5, 6], compared with usual observation, showed a more persistent reduction in behavioral risk factors, caused, in particular, by eating habits, physical activity, and smoking. As a result of training, patients’ adherence to taking antihypertensive drugs and following comprehensive medical recommendations increases [2, 5, 6]. The training was accompanied by a 2-fold increase in the number of patients who achieved target blood pressure, which was not noted during routine follow-up [5, 6]. In the group of trained patients, the number of cases of temporary disability and the frequency of hospitalizations steadily decreased. The positive effect of educational technology was noted not only in terms of increasing the level of knowledge and skills of self-control and improving behavioral habits, but also in terms of reducing the total risk of cardiovascular complications, as well as the frequency of myocardial infarction and strokes (by 2 times). Patient education in health schools is economically feasible as it will reduce treatment costs [7, 9]. Thus, testing of educational medical preventive technology aimed at multifactorial prevention of hypertension has convincingly demonstrated, on the one hand, the feasibility of its implementation in practice, and on the other hand, its effectiveness in various groups of patients with hypertension. The data obtained are the basis for recommending a wider introduction of educational technology for multifactorial prevention of hypertension into healthcare practice, which will improve the prognosis and quality of life of patients, and reduce the economic losses of society due to complications of this disease [4].
Health schools, as one of the preventive medical services, can serve as a standard for the quality of preventive medical care and be a model for the development of a new direction - assessing the quality of preventive medical care, based on the principles of healthcare reform and orientation towards the provision of medical care in primary healthcare [20].
It should be noted that, unlike narrow specialists, a family doctor has the opportunity to continuously and long-term monitor his population, as a result of which conditions are created for primary, secondary and tertiary prevention of hypertension, including patient education at the primary health care level.
The purpose of the study is to improve the effectiveness of the prevention and treatment of hypertension by educating patients in hypertension schools at the primary health care level. To achieve the goal, the following tasks were formulated: to study the tactics of patient management, the awareness of general practitioners about the principles of prevention and treatment, as well as the adherence of patients with hypertension to compliance with non-drug and drug recommendations at the primary health care level; develop a structured program for training patients with hypertension with information interventions in a family clinic and rural medical centers; compare the results of patient adherence to treatment, analyze the results of therapeutic and preventive interventions before and after 24 months of observation.
Material and methods
A retrospective analysis of data (over the last 5 years) was carried out on 222 randomly selected outpatient records of patients with hypertension who were registered at a family clinic (n=54) and in some rural medical centers of the Republic of Uzbekistan (n=168). Data from a retrospective analysis of outpatient records were compared with the results of examination of patients (questioning, examination, anthropometry, blood pressure measurement, cholesterol determination, etc.). Doctors from the Tashkent polyclinic and medical centers in rural regions of the republic who completed 10-month retraining courses for general practitioners were interviewed. A survey of 156 doctors before training and 119 doctors after training was conducted, as well as a survey and examination of 236 patients with hypertension who were undergoing dispensary observation in clinics and medical centers. Subsequently, some of them (the main group; n=122) completed a training course at a school for hypertensive patients, and some (the comparison group; n=114) did not participate in the educational program. All patients were under our observation for 2 years with subsequent re-examination and examination. In the main group (patients' age from 45 to 71 years, average - 51.75±1.85 years; 29.5% men, 70.4% women), the distribution of patients by disease stage was as follows: stage I hypertension - 45 ( 36.8%) people; Stage II - 62 (50.8%); Stage III - 15 (12.2%). A crisis course of the disease was observed in 40 (32.7%) patients. The comparison group consisted of 114 patients (80 (70.1%) women and 34 (29.8%) men, aged 44-75 years, average - 52.6 ± 1.62 years), treated according to the traditional method and not participating in the educational program. In this group, stage I hypertension was detected in 41 (35.9%) people; Stage II - in 61 (53.5%); Stage III - in 12 (10.5%) people. A crisis course of the disease was observed in 37 (32.4%) patients. The groups were comparable in terms of main clinical and laboratory-instrumental parameters.
In the main group, 46 (37.7%) patients had an average risk of cardiovascular complications, 63 (51.6%) had a high risk, and 14 (11.4%, p <0.05) had a very high risk.
In the comparison group there were 41 (35.9%), 62 (54.3%) and 11 (9.6%, p <0.05) patients, respectively.
Schools for hypertensive patients are organized on the basis of the Educational and Medical Center No. 3 at the Tashkent Medical Academy, located in the family clinic No. 32 of Tashkent, and rural medical centers in two regions of the republic; Methodological materials were developed taking into account the specifics of the work of family doctors. When compiling the training technology, the level of education of the patients was taken into account. In our opinion, taking into account the mentality of our population, 10 lessons of 90-120 minutes each with a break of 15-20 minutes (once a week, preferably on Saturday) can be considered optimal. Study material should be presented according to a structured syllabus in a logical sequence across the following sections.
— Meeting the group, talking about the need for hypertension training at school and conducting a survey. What is AG? Mechanisms of blood pressure regulation in the body. Cardiovascular diseases are lifestyle diseases. Risk factors for hypertension.
- Complications of hypertension - hypertensive crises, myocardial infarction, cerebral stroke. Training in the method of measuring blood pressure, determining pulse rate, and keeping a self-monitoring diary.
— What leads to increased blood pressure and how to avoid it? Non-drug methods for treating and preventing hypertension. Excess body weight as a significant risk factor for cardiovascular diseases. Body weight control. Types of obesity. Determination of excess body weight.
— Rational nutrition for hypertension and obesity. The effect of table salt on the body, the relationship between sodium chloride and high blood pressure.
— Therapeutic exercises for hypertension. What is regular dosed physical activity and how to do it?
— Basics of drug treatment of hypertension. Concept and principles of basic antihypertensive therapy. Inadmissibility of course treatment of hypertension and treatment from case to case. The concept of target blood pressure is below 140/90 mmHg.
— The main manifestations of a hypertensive crisis and the factors that provoke it. Self-help for acute increases in blood pressure, emergency first aid kit for hypertension.
— Improving and practicing practical skills acquired in the classroom. Training in independent outpatient daytime blood pressure monitoring (SADMAD method) and its significance.
— Analysis of self-monitoring diaries with patients. Conducting repeated surveys of patients on risk factors, tactics of management and treatment of hypertension after completing the training course.
— Final lesson. Psychological causes of hypertension. Learning to deal with stress appropriately. Analysis of questionnaires filled out in classes before and after training. Presentation of school completion certificates.
When organizing schools for hypertensive patients, it is necessary to adhere to the following methodology for conducting classes: recruiting patients into groups of 10-14 people; venue - a specially prepared thematic room; necessary technical means for training: banners, multimedia projector, phantoms, scales, height meter, measuring tape, blood pressure measuring device, etc.; the form of presentation of the material is an interactive conversation-lecture; The duration of classes is 90-120 minutes with an interval of 15-20 minutes (Table 1).
Students should be encouraged to keep a self-monitoring diary assessing and monitoring controllable risk factors, blood pressure results, and a schedule for taking antihypertensive medications. To acquire practical skills in self-control and self-help during acute increases in blood pressure, special attention should be paid to classes in which patients are taught the principles and skills of non-drug and drug treatment of hypertension. Teach SADMAD techniques, pulse counting and other practical skills (determining excess body weight, stocking an emergency first aid kit and providing self-help for acute increases in blood pressure) for adequate control of blood pressure levels. This will allow you to evaluate changes in blood pressure and heart rate in the early morning and several times during the day before going to bed, it is not burdensome for the patient, it is informative and will increase the patient’s adherence to treatment, and allows you to monitor the effectiveness of antihypertensive therapy. SADMAD is recommended as a mandatory method for studying hemodynamics in an outpatient setting when assessing the effectiveness of antihypertensive therapy, in diagnosing hypertension, especially in hypersensitive patients with high levels of anxiety and depression, as well as in patients without any symptoms.
Results and discussion
In a retrospective analysis of risk factors recorded in outpatient records of the clinic (n=54) and medical stations (n=168), the following results were obtained. Compounded heredity was established in the clinic in 34 (62.9%) cases and in medical centers - in 88 (52.3%), smoking - in 16 (29.6%) and 47 (27.9%) cases, excess weight body - in 18 (33.3%) and 35 (20.8%), alcohol abuse - in 9 (16.6%) and 37 (22.0), hypercholesterolemia - in 21 (38.8%) and 43 (25.6%), physical inactivity - in 25 (46.2%) and 57 (33.9%), stress - in 38 (70.3%) and 115 (68.4%), respectively. The most common risk factors were family history, stress, excess body weight, and physical inactivity.
In most outpatient records, recommendations for non-drug treatment are given incompletely. Limiting table salt is recommended by 35 (64.8%) clinic doctors and 53 (31.5%) rural doctors; auto-training - 24 (44.4%) and 64 (38.0%); restriction of fat consumption - 31 (57.4%) and 71 (42.2%); fluid restriction to 1-1.5 l/day - 25 (46.2%) and 54 (32.1%); weight loss in obesity - 37 (68.5%) and 71 (42.2%); smoking cessation - 11 (20.3%) and 72 (42.8%); regular physical education - 37 (68.5%) and 67 (39.8%), respectively. A comparative analysis of retrospective indicators from outpatient records with data from oral interviews with doctors and examinations of the same patients revealed a significant discrepancy (p<0.001) in these risk factors. These data allow us to conclude that the majority of patients did not undergo timely identification and correction of hypertension risk factors.
While studying outpatient records, we paid attention to the rules for prescribing antihypertensive drugs with proven effectiveness. β-Adrenergic blockers are prescribed in the clinic in 44.4% of cases, in medical centers - in 8.9%; diuretics - in 35.1 and 10.7%, respectively; calcium antagonists - in 24 and 5.9%; ACE inhibitors - in 51.8 and 42.2%, respectively. Despite the prescription of first-line antihypertensive drugs, dibazole, papazole, adelfan, raunatin, papaverine and no-spa were also prescribed, in courses without a specific regimen or duration of use.
Antihypertensive drugs are regularly prescribed by 35 (64.8%) doctors at a polyclinic and 30 (17.8%) at medical centers; short courses are prescribed by 19 (35.1%) and 138 (82%) doctors, respectively; the differences in both cases are highly significant ( p<0.001).
Thus, in most cases, general practitioners do not adhere to the principles of non-drug treatment methods and basic drug therapy based on continuous long-term use of drugs in effective doses.
An anonymous survey of doctors from clinics and medical centers who underwent 10-month retraining courses revealed an underestimation of risk factors and their correction by doctors in patients with hypertension. After training, the number of doctors who attach importance to identifying and correcting risk factors significantly increased (p<0.001). Thus, reducing the consumption of table salt before training was recommended by 46.0% of clinic doctors and 30.1% of medical stations, after training - 92.3 and 76.1%, respectively; weight loss before training - 26.9 and 15.0% of doctors, after - 96.1 and 85.0%, respectively; Limiting fat intake was recommended by 20.6 and 16.1% of doctors before training, and by 94.2 and 43.2%, respectively, after training.
Most doctors do not fully understand the methods of modern prevention of hypertension. Reducing negative factors caused by lifestyle is the main goal of preventing hypertension, an effective means of lowering blood pressure and preventing complications. The role of the general practitioner in convincing patients to follow simple recommendations is extremely important.
A total of 236 patients were involved in a questionnaire survey of patients undergoing follow-up for hypertension. When analyzing the questionnaires, the following groups of signs were assessed: patients’ awareness of hypertension, blood pressure levels, and its complications; the ability to provide self-help in case of a sharp increase in blood pressure; knowledge of non-drug treatment methods for hypertension; possession of practical skills (independent measurement of blood pressure, determination of pulse rate, etc.); attitude towards taking antihypertensive drugs.
Patients participating in the educational program significantly (p<0.001) improved their knowledge of risk factors and practical skills to improve the quality of hypertension control (Table 2).
In the group of patients who did not undergo training, no particular difference in the provision of self-help was detected before being taken under observation and after 2 years of observation. All 122 patients who completed the training mastered the skills of independently measuring blood pressure and counting pulse. In the comparison group, these indicators remained almost at the same level. Repeated questioning after training showed a significant (p <0.001) increase in the number of patients taking antihypertensive drugs; 82.7% of trained patients began to take them “constantly” and 9.0% of trained patients “occasionally” with an excessive increase in blood pressure.
The majority of patients in the comparison group do not have the skills to provide self-help in case of a sudden increase in blood pressure and self-monitoring of blood pressure. In addition, one of the principles of drug antihypertensive therapy (taking medications with regularity and duration) is not supported. After 24 months of observation, the rules for taking antihypertensive drugs remained almost unchanged. The results of a survey of patients prove the need to train patients with hypertension in a number of skills and abilities that allow timely provision of self-help with an acute increase in blood pressure and maintaining its target level while observing non-drug treatment methods and rules for taking antihypertensive drugs.
One of the main links in the measures taken to prevent hypertension at the outpatient stage should be increasing the educational level of patients. If a general practitioner takes time for each patient and develops an individual program of non-drug and drug treatment, then it will be very difficult to implement it, since untrained patients lack motivation for treatment. Only after being informed about the principles of preventing hypertension and its complications do patients’ adherence to treatment increase and they become responsible for their health. A hypertension school at the primary health care level is an ideal and appropriate method of increasing the knowledge, skills and abilities of patients for quality control and monitoring of their condition.
Among the factors influencing the effectiveness of treatment of patients with hypertension, along with the clinical features of the disease and the correctness of medical prescriptions (choice of drug, dose, regimen, etc.), patients’ adherence to treatment is of great importance, i.e. completeness and correctness of implementation of medical recommendations.
In patients who completed the training, there was a positive change in the lipid spectrum: the number of patients with hypertriglyceridemia (p<0.001) and hyper-LDL cholesterol (p<0.001) decreased (Table 3)
All patients stopped drinking alcohol (p<0.001) and quit smoking; physical inactivity was observed only in 30.3% (p <0.001). The number of patients with impaired glucose tolerance decreased (p<0.001).
Significant changes in the clinical picture of the disease were also noted: dizziness and headaches began to occur less frequently (p<0.001), and there was a tendency towards a decrease in shortness of breath during physical activity (p<0.001) (Table 4).
The number of patients suffering from exertional angina, as well as those with rhythm disturbances, has not increased.
Patients who completed the training significantly (p<0.001) increased the intake of long-acting antihypertensive drugs: ACE inhibitors - from 19.6 to 91.8%; β-blockers - from 29.5 to 39.3%; calcium antagonists - from 6.5 to 59.0%; diuretics - from 13.1 to 66.3%, respectively (Fig. 1).
Figure 1. Long-acting antihypertensive drug use in a hypertensive school-trained cohort. The differences between the indicators before and after training were significant in all cases (p<0.001). AT-1 receptor blockers were taken before training in 5.7% of cases; after 2 years of observation, the frequency of prescription of these drugs significantly (p<0.001) increased and amounted to 13.1%.
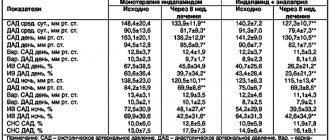
The majority of patients who completed the training achieved positive dynamics in the levels of systolic (SBP) and diastolic (DBP) pressure (Table 5).
The reduction in blood pressure levels achieved during 2 years of follow-up was characterized by a positive association with learning.
In the group of patients who did not attend school, target blood pressure levels were achieved only in 29 (25.8%) patients (p <0.01).
Patients who completed training at the hypertension school showed a significant (p <0.001) improvement in knowledge about hypertension risk factors and awareness of the presence of hypertension, increased adherence to treatment and drug treatment with achievement of the target blood pressure level (Table 6).
The course of hypertension was accompanied by a significant decrease in the frequency of hypertensive crises and hospitalization, and side effects of drug therapy.
In the comparison group, against the background of prescribed therapy, positive significant dynamics were noted: patients began to monitor their blood pressure more often, the selection of adequate drug therapy improved, although patients’ awareness of the presence of hypertension, patients’ knowledge of the main risk factors for hypertension, adherence to treatment remained low, and a decrease in the number of hypertensive crises was unreliable.
It should be noted that 118 (96.7%) patients began to independently monitor blood pressure using the SADMAD method and keep a self-monitoring diary, which contributed to increased adherence to drug therapy and improved the relationship between the doctor and the patient.
The most difficult thing for patients was the conscious implementation in practice of such measures to normalize lifestyle, such as losing body weight, increasing physical activity, adhering to the principles of rational nutrition, limiting the use of table salt, quitting smoking, and alcohol abuse. After 2 years, 48 (39.3%) patients increased physical activity, 49 (40.1%) limited their salt intake. Of the dietary recommendations for 98 (80.3%) patients, limiting the consumption of animal fats and increasing unsaturated fats in the diet were easily feasible. In general, these measures were accompanied by a decrease in blood cholesterol levels and a decrease in the number of patients with impaired glucose tolerance.
The role of SADMAD in the formation of adherence to treatment has been revealed. In the main group, SADMAD in the amount of 10 measurements per day was carried out by 51 (41.8%) patients; 6 measurements per day - 35 (28.6%); 4 measurements per day - 22 (18.0%); 2 measurements per day - 10 (8.1%). SADMAD was carried out before the prescription of medications and against the background of antihypertensive treatment. The identified features of the chronostructure of SADMBP in patients with hypertension allowed us to develop tactics for drug prescriptions for a specific patient with corresponding positive dynamics in the daytime blood pressure profile.
Once target BP has been achieved with therapy, follow-up examinations should be scheduled at 6-month intervals for patients at average and low risk who regularly measure BP at home. For patients at high and very high risk, as well as for patients receiving only non-drug treatment, and for those with low adherence to treatment, the intervals between visits should not exceed 3 months [14]. Regular medical examinations that provide continuous monitoring can be ensured by involving patients in activities related to education and acquisition of self-control skills.
Treatment of a patient with hypertension is carried out continuously, in most patients - for life, since its withdrawal is accompanied by an increase in blood pressure. With persistent normalization of blood pressure for 1 year and compliance with lifestyle changes in patients with low and average risk, a gradual reduction in the amount and/or dose of antihypertensive drugs taken is possible. Reducing the dose and/or reducing the number of medications used requires increasing the frequency of visits to the doctor and performing SADMAD at home to ensure that there are no repeated increases in blood pressure [14].
When analyzing ECG registration and observation data in the main group, it should be noted that there were no negative dynamics in changes in the PQ, QRS, QT intervals, which could indicate side effects of antihypertensive therapy (Table 7).
After 2 years, a significant (p <0.01) decrease in ST segment depression was observed in the main group.
Stabilization of the general condition (absence of exacerbations) in patients who completed training at the school of hypertension occurred in 96.7% of cases, target blood pressure levels were achieved in 82.7% of patients. Hypertensive crises recurred only in 4 (3.2%) cases, mainly in patients with stage III hypertension (Fig. 2).
Figure 2. Clinical outcomes of HD patients in the studied groups over 2 years of follow-up. 1 — headache exacerbations per year; 2 — stabilization of condition; 3 — target blood pressure level; 4 — myocardial infarction; 5 - cerebral stroke; 6—death.
conclusions
1. At the primary health care level, in most patients with hypertension, risk factors are not fully identified; Some of them do not undergo correction of identified modifiable risk factors; The vast majority of patients use antihypertensive drugs in short courses, without observing the regularity and duration of use.
2. There is low awareness among general practitioners about the principles of prevention and treatment of hypertension in an outpatient setting.
3. Patients with hypertension are not sufficiently aware of the risk factors (33.9%) that influence the course and prognosis of the disease; do not have the skills of self-control (63.3%) and self-help (75%) in case of acute increase in blood pressure; there is low adherence (24%) of patients to following medical recommendations.
4. Antihypertensive therapy in patients with hypertension who do not participate in the educational program does not significantly affect manageable risk factors and does not lead to the achievement of target blood pressure levels (29%).
5. The School of Hypertension is an effective system for organizing patient education and conducting complex therapy in clinics and medical centers; significantly contributes to the prevention of cardiovascular complications, adequate control of SBP and DBP (96.7%).
6. SADMAD is an informative and objective method of monitoring patients on an outpatient basis, promotes the formation of patient adherence to antihypertensive therapy, and allows assessing its effectiveness.
7. Patients who completed the training began to independently monitor blood pressure using the SADMAD method and keep a self-monitoring diary, which contributed to increased compliance with the drug therapy regimen and improved interaction between the doctor and the patient.
8. Adequate pharmacotherapy is optimally possible in patients participating in the educational program; in our study, this training made it possible to achieve the target blood pressure level in 82.7% of patients, reduce the pharmacological load on the body and thereby reduce the number of adverse reactions of drug therapy.
How to eat properly if you have hypertension?
Here is a healthy eating pyramid. It is based on grain products (7-8 servings per day), vegetables and fruits.
Proper nutrition for hypertension involves:
- low salt intake - no more than 1 teaspoon per day;
- eating 4-6 times a day in small portions;
- enriching the diet with fresh vegetables (4-5 servings per day) and fruits (2-4 servings per day);
- consumption of low-fat dairy products (2-3 servings per day);
- It is preferable to eat fish, lean meats, preferably boiled;
- limiting the consumption of sweets to 1 time per week.
1 serving is:
- dairy products: 250 ml 1% milk or 120 ml 2% yogurt;
- boiled meat, fish, poultry - 84 g;
- vegetables, fruits: 160 grams of boiled or fresh vegetables, 180 ml of vegetable or fruit juice, 1 medium-sized fruit;
- grain products: 1 slice of bread (preferably wholemeal flour), 120 ml of oatmeal.
Tomatoes clean vessels
And the University of Cambridge (England) pleased with the news about the unexpected side of tomatoes. It turns out that the substance lycopene, which is part of their composition, has an amazingly beneficial effect on the endothelium - the inner walls of blood vessels. The benefits of lycopene as an antioxidant have been discussed more than once, but now it has become clear that it also cleanses blood vessels from the inside, improving their permeability by 53%. Of course, this is if the vessels were in poor condition; in healthy ones, it simply maintains the norm. Conveniently, lycopene, unlike many useful substances, is not afraid of heat, so tomatoes can be stewed and baked with a clear conscience.
Hypertension threatens dementia
A study by the National Institute on Aging (Maryland, USA) found that dementia in people after 70 years of age is directly related to high blood pressure after 50 years of age. “What do you want,” say the researchers, “when the blood literally puts pressure on the brain, the nerve cells will not be able to work normally!” There is also good news: lowering blood pressure to normal helps restore memory and cognitive abilities by 10%. So the recommendation to monitor your blood pressure and, if necessary, take medications regularly is especially important for those who earn their living by mental work.
Similar data were obtained at Brigham Youth University (Utah, USA). Here they recommend monitoring your blood pressure for anyone who suffers from forgetfulness, irritability, and generally believes that they have become poor at understanding everyday matters. According to them, losing weight to normal and replacing fatty foods with vegetables improves brain function by 2.7–4.6%.