Thoracic osteochondrosis
is a degenerative-dystrophic disease in the middle parts of the spine. It occurs much less frequently than lumbar and even cervical osteochondrosis and accounts for about 10% of all cases of the disease. Symptoms of thoracic osteochondrosis are associated with several features of the spine in the thoracic region: rigid fixation of the vertebrae due to the ribs and skeletal muscles and less mobility, a semicircular bend of the ridge in this region and the corresponding distribution of the load.
Thoracic osteochondrosis is a disease of the middle parts of the spine.
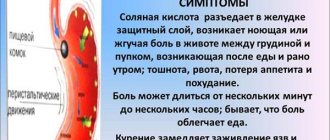
Symptoms of thoracic osteochondrosis begin with a violation of tissue trophism and dehydration of the intervertebral discs. Lack of nutrients and fluid leads to the fact that cartilage loses its elasticity, begins to crack and “sag”
.
This state of affairs is fraught with compression of the nerve roots, deterioration of sensitivity and functioning of internal organs, as well as severe pain. Often, the destruction of the vertebrae in the thoracic region is accompanied by the appearance of osteophytes
- bone outgrowths that injure the paravertebral tissues and lead to chronic inflammation.
Contrary to popular belief, thoracic osteochondrosis is not a natural age-related process and requires special treatment. The onset of the disease can occur at the age of 25 years
;
approximately 70% of the total number of patients are women aged 35 to 55 years. Since the disease begins long before retirement age, it can lead to limitations and even loss of ability to work
.
Unlike other types of osteochondrosis, thoracic osteochondrosis may not manifest itself for a long time - or disguise itself as other pathologies, which is why it is called a chameleon disease. It is also the most difficult to treat. Therefore, it is very important to promptly monitor the symptoms of thoracic osteochondrosis.
- and today we will tell you which ones.
Spinal problems
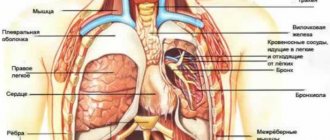
Chest pain when inhaling often appears due to pathologies of the spinal column. The fact is that the spine contains a huge number of nerve endings, inflammation and/or infringement of which can lead to pain radiating into the chest, causing pain when inhaling.
Osteochondrosis
It is a serious disease that affects the cartilage tissue of the spinal column. The intervertebral discs thin out and become less durable, resulting in a decrease in the distance between the vertebrae. Because of this, nerve tissue is pinched, which leads to pain. If the pain intensifies when you inhale, this may indicate that the thoracic spine is affected.
Intercostal neuralgia
Sharp acute pain in the chest when inhaling occurs when compression or irritation of the nerve roots that are located between the ribs occurs. This condition can last literally a couple of minutes or drag on for a day, preventing the person from taking a deep breath and causing significant discomfort. The pain can come on suddenly, for no apparent reason, and often makes a person worry and think that the heart is stabbing, although the reason is completely different.
Fractured ribs
If you have recently been injured and experience pain in your chest when you inhale, you may suspect a rib fracture. This is a dangerous condition, and with a visit to a traumatologist
/
the surgeon
cannot hesitate, since, among other things, you may have damage to internal organs.
The fracture itself, depending on its severity, can provoke additional damage.
Diagnostics
Such a complex symptom as aching or acute pain in the left chest requires careful diagnosis. The therapist decides where exactly to look for its cause.
by collecting detailed information about the circumstances under which the pain occurs and the patient's health status.
If necessary, the patient can be sent to a specialist neurologist
.
Diagnosis often begins with the exclusion of diseases of the cardiovascular system - an ECG
and a visit to
a cardiologist
; if necessary, the patient is prescribed
an echocardiogram
. In other cases, to diagnose diseases that cause chest pain on the left, blood tests, endoscopic, ultrasound and x-ray examinations can be prescribed.
Diseases and pathologies of the heart
Often, when inhaling, pain appears in the left chest if there is a heart problem. In this case, there may be quite a few reasons, and only an experienced pulmonologist
.
Pericarditis
Pericarditis is an inflammation of the heart sac - the outer lining of the heart, which is called the “pericardium”. The nature of such a disease can be infectious, rheumatic, or result from a heart attack. With pericarditis, not only does pain appear when inhaling on the right or left side of the chest; the condition is often accompanied by severe weakness, as well as shortness of breath if fluid leaks between the layers of the pericardium. Pericarditis with effusion can develop into suppuration and cause compression of the heart by accumulated secretions.
Pulmonary embolism
This is the name of the condition when the pulmonary arteries stop passing blood, i.e. clogged. This is a consequence of a blood clot (thrombus), drops of fat, bone marrow, catheter element or other foreign body entering the arterial bed. In this case, when inhaling, pain occurs in the left side of the chest, and the person needs urgent medical attention.
When pain is deadly
The most dangerous pain sensations are those associated with heart and lung diseases. This condition can be recognized by the following signs:
- The painful sensation lasts more than 5 minutes.
- A sharp burning pain behind the sternum, which gradually spreads to the neck, shoulders and back.
- There is a feeling of pressure and tightness in the chest.
- The heart rate increases greatly, the patient finds it difficult to breathe, and shortness of breath appears.
- The person breaks into a cold sweat, dizziness begins, weakness and nausea with vomiting appear.
If any of the listed symptoms occur, you should immediately call an ambulance.
Pulmonary pathologies
There are many causes of pain in the sternum during inspiration, which are associated with pathologies of the respiratory system. It is worth considering some cases when pain may appear when inhaling.
Pneumothorax
It is an accumulation of gas in the pleural cavity, which leads to the collapse of lung tissue, from which the process occurs. In this case, the mediastinum shifts towards the healthy organ, the blood vessels are compressed, which leads to respiratory disorders, and blood circulation is also impaired. Often pneumothorax is traumatic, and can also be a consequence of spontaneous disruption of tissue integrity.
Pleuropneumonia
If chest pain appears when taking a deep breath, this may indicate progressive pulmonary pneumonia, when the pleura is involved in the pathological process. This disease is very dangerous; Along with pain when inhaling, a person notes the inability to take a deep breath and general weakness.
Pleurisy
Inflammation of the serous membrane of the lungs is called pleurisy and may be accompanied by pain when inhaling. In this case, a person not only has pain in the chest area when inhaling, but also shortness of breath, cough, pulmonologist
notes pleural friction noise when listening to breathing, and the temperature also rises.
Lungs' cancer
Pain in the middle of the chest when inhaling can occur if a malignant neoplasm has developed in the lungs. Pain syndrome is a consequence of tissue proliferation and compression of neighboring structures. To determine why your chest begins to hurt when you inhale and move, first consult a neurologist
, who, after a survey and examination, will refer you to a specialist.
Non-cardiac causes of heart pain and numbness in limbs
Most often, the patient’s left arm and heart hurt, in the case of a disease not of the heart, but of neighboring organs. We are talking about pathologies of the lungs, kidneys, and musculoskeletal system. Among them:
- Osteochondrosis. With the development of osteochondrosis, the load also goes on the cardiac system. In addition to unpleasant sensations in the spine, there is severe pain in the heart and numbness in the limbs. Requires special attention from medical professionals to prevent the development of the disease.
- Consequences of injuries. After injuries, disturbances occur throughout the body.
- Duodenal ulcer. With a duodenal ulcer, the limbs often become numb. You should consult a doctor as soon as possible.
- Pancreatitis. Associated symptoms include nausea, vomiting, dizziness, pale face, and fever.
- Gastrointestinal tract disorders. With gastrointestinal disorders, the patient feels unbearable pain not only in the stomach, but also in the heart. A lot of stress is placed on the heart.
- Neuralgia.
- Hormonal disorders. Most often the heart hurts and radiates to the arm in women. In some cases, symptoms are associated with hormonal imbalances.
- Pregnancy. During pregnancy, the functionality of a woman’s body completely changes. The load occurs on all organs, especially the heart. As a result, the pregnant woman feels unwell and has numbness in her limbs.
- Pathologies of the mammary glands.
- Benign and malignant tumors.
- Tuberculosis.
- Bronchial asthma.
- Dry pleurisy.
Treatment
Help before diagnosis
For moderate chest pain on the right side caused by a bruise, it is enough to rest for several days, apply dry compresses and ointments with anti-inflammatory drugs to relieve discomfort. If the pain does not subside and is accompanied by swelling and bluishness of the skin, you should visit a specialist to promptly identify a rib fracture as the probable cause of the symptom. Pain syndrome that occurs against the background of coughing and shortness of breath is an indication to consult a doctor - independent treatment of diseases of the respiratory system is fraught with serious complications.
Conservative therapy
In most cases, it is enough to treat the underlying cause of pain, but for severe and unbearable pain in the right chest, analgesics (both NSAIDs and narcotic drugs) are indicated. To eliminate pain, physiotherapy methods are used: electrophoresis, compresses on the affected area with dimexide, corticosteroids, and anti-inflammatory drugs. The following medications are prescribed as etiotropic therapy:
- Antibiotics
. Medicines are used to destroy bacterial microorganisms that cause pneumonia or purulent bronchitis. Beta-lactam antibiotics and macrolides are often taken or administered. Fluoroquinolones and interferon are effective for the treatment of atypical pneumonia. - Nonsteroidal anti-inflammatory drugs
. NSAIDs reduce the production of cytokines and active mediators, reduce local manifestations of the inflammatory process, and reduce febrile fever. For chest injuries, they relieve pain well. The products are used both orally and externally in the form of ointments. - Expectorants
. Medicines thin the mucus, which clears the airways and speeds up recovery time. Mucolytics and reflex herbal remedies are used. To sanitize the upper respiratory tract, gargling with antiseptics is recommended. - Derivatives of ursodeoxycholic acid
. The drugs reduce the concentration of toxic acids and reduce the rate of stone formation in the gallbladder by normalizing the chemical composition of bile. UDCA also has hypolipidemic and hypocholesterolemic effects and protects hepatocyte membranes. - Vitamins.
Thiamine, pyridoxine and other B vitamins improve the nutrition of nerve fibers and accelerate the regeneration of the myelin sheath. For better absorption, they can be combined with ascorbic acid. Tocopherol is prescribed as an antioxidant.
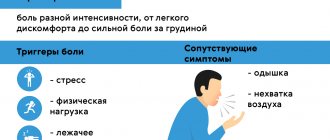
Chest pain is any pain or discomfort in the chest area. It can be caused by various diseases, including pathology of the heart, blood vessels, pericardium, lungs, pleura, trachea, esophagus, muscles, ribs, and nerves. In some cases, chest pain is a sign of damage to organs outside the chest, such as the stomach, gallbladder, or pancreas.
Chest pain is very diverse: sharp, dull, aching, cutting, stabbing, pulling, bursting, burning or pressure. Painful sensations vary among different diseases, but pain is not a specific symptom of a particular disease. The characteristics of pain may vary depending on the age, gender of the patient, concomitant diseases, and psychological characteristics. Identifying the immediate cause of chest pain is often difficult and requires a number of diagnostic procedures.
It is one of the most alarming symptoms, as it can be a manifestation of severe, life-threatening conditions that require emergency medical care, in particular myocardial infarction.
Synonyms Russian
Thoracalgia, chest pain, chest pain
English synonyms
Chest pain, pain in the chest, thoracalgia.
Symptoms
Chest pain can be of different types. Sometimes it radiates to the arm, shoulder, shoulder blade, back, neck. The patient may complain not only of pain, but also of tightness, burning, and discomfort in the chest area.
Unpleasant sensations may intensify when coughing, deep breathing, swallowing, pressing on the chest, changing body position (constant or periodic). Chest pain and discomfort may be accompanied by a number of additional symptoms, depending on the underlying disease: belching or bitterness in the mouth, nausea, vomiting, difficulty swallowing.
General information about the disease
Chest pain can be a manifestation of various diseases, each of which requires a specific medical approach.
- Acute myocardial infarction (heart attack). Acute chest pain in people over 40 years of age is most often associated with this disease. Myocardial infarction occurs when a section of the myocardium is damaged and killed as a result of impaired circulation in the coronary vessels. Most often it manifests itself as acute pain behind the sternum or to the left of the sternum, which radiates to the back, neck, shoulder, arm and does not decrease when taking nitroglycerin or at rest. Symptoms vary from patient to patient. Elderly women are characterized by atypical symptoms: severe weakness, nausea and vomiting, rapid breathing, abdominal pain.
- Angina pectoris. A condition in which, as a result of atherosclerosis and narrowing of the coronary vessels, the blood supply to the heart muscle is disrupted. Pain during angina pectoris resembles that during myocardial infarction, but occurs during physical activity, decreases with rest and is relieved by nitroglycerin.
- Dissecting aortic aneurysm. The aorta is a large vessel that carries blood from the left ventricle of the heart to organs and tissues. With a dissecting aneurysm, a rupture of the intima (inner lining) of the aorta occurs with penetration of blood into other layers of the aortic wall and subsequent dissection of the wall, which most often leads to complete rupture of the aorta and massive internal bleeding. The disease in most cases ends in death within a few hours or days, even with timely diagnosis and timely treatment.
Dissecting aortic aneurysm is most often a consequence of long-term arterial hypertension, and can also occur with Marfan syndrome, as a result of chest trauma, during pregnancy, or as a later complication of heart surgery.
Pain with dissecting aortic aneurysm is similar to pain with myocardial infarction and angina pectoris, can last for several hours or days, and does not decrease with rest or with nitroglycerin.
- Pulmonary embolism. Blockage of the pulmonary artery or its branches by a thrombus, through which venous blood flows from the right ventricle to the lungs for oxygen saturation. As a result, gas exchange is disrupted, hypoxia occurs, and pressure in the pulmonary arteries increases. Chest pain occurs suddenly, intensifies with deep inspiration, is accompanied by rapid breathing and, in some cases, hemoptysis. The risk of thromboembolism increases after surgery, prolonged forced immobility, pregnancy, taking oral contraceptives, especially in combination with smoking, and cancer.
- Pneumothorax. The accumulation of air or other gas in the pleural cavity, a slit-like space between the membranes lining the surface of the lungs and the inner surface of the chest. Accompanied by acute chest pain, rapid breathing, anxiety, loss of consciousness.
- Pericarditis. Inflammation of the heart sac (pericardium), that is, the serous membrane of the heart. Pain occurs due to friction of the inflamed pericardial layers. Pericarditis can be a consequence of a viral infection, rheumatoid arthritis, systemic lupus erythematosus, or renal failure. Idiopathic pericarditis, that is, pericarditis of unknown etiology, is common. The pain is acute, occurs only in the initial stages of the disease, and may be accompanied by rapid breathing, fever, and malaise.
- Mitral valve prolapse. Pathology of the valve, which is located between the left atrium and the left ventricle of the heart. In some people, when the left ventricle contracts, the mitral valve bends into the atrium and some of the blood from the left ventricle flows back into the left atrium. For most patients, this does not cause discomfort, but some experience increased heart rate and chest pain that does not depend on physical activity and does not radiate, unlike angina.
- Pneumonia. Inflammation of the lung tissue. Chest pain with pneumonia is usually one-sided, worsens with coughing, and is accompanied by fever, malaise, and cough.
- Esophagitis. Inflammation of the esophagus. Accompanied by chest pain and difficulty swallowing. Symptoms do not improve with antacids.
- Gastroesophageal reflux disease. A chronic disease in which acidic stomach contents reflux into the esophagus, leading to damage to the lower esophagus. In this case, acute, cutting pain in the chest along the esophagus, heaviness, discomfort in the chest, belching, bitterness in the mouth, difficulty swallowing, and dry cough may occur.
- Pleurisy. Inflammation of the pleura. Friction of the inflamed pleura causes pain. Pleurisy can be the result of a viral or bacterial infection, cancer, chemotherapy or radiation therapy, or rheumatoid arthritis.
- Fractured ribs. In this case, the pain intensifies with deep breathing and movement.
- Other causes: pancreatitis, cholelithiasis, depression.
Who is at risk?
- People over 40 years old.
- Obese people.
- Patients with arterial hypertension.
- People with high levels of cholesterol in the blood.
- Have recently undergone surgery.
- Those suffering from alcoholism.
- Smokers.
- Pregnant women.
- Suffering from cardiac arrhythmia.
- People with cancer.
- Taking certain medications.
- People with chronic lung diseases.
Diagnostics
Chest pain is not a specific symptom and can clearly indicate a particular disease. However, when this sign appears, the doctor must first of all exclude a number of life-threatening conditions that require immediate help. Sometimes only additional laboratory and instrumental studies can accurately determine the cause of chest pain.
Laboratory research
- General blood analysis. Leukocytosis (with pleurisy, pneumonia), anemia (with dissecting aortic aneurysm), thrombocytosis and erythremia (with pulmonary embolism) can be detected.
- Erythrocyte sedimentation rate (ESR). Nonspecific indicator of inflammation. ESR can be increased with pleurisy, pericarditis, pneumonia and other diseases.
- C-reactive protein. Increased in inflammatory diseases, as well as in myocardial infarction. With angina, the level of C-reactive protein does not change.
- NT-proBNP (brain sodium uretic propeptide). A protein, the main part of which is found in myocardial cells. It is a precursor of natriuretic peptide, responsible for the excretion of sodium in the urine. This indicator is used to assess the risk of heart failure, identify the initial stages of heart failure, and evaluate therapy. Is highly specific. May be elevated during myocardial infarction.
- Troponin I. Troponin is a protein involved in muscle contraction. The cardiac form of troponin is found in the heart muscle and is released when the myocardium is damaged. It may be increased in myocardial infarction and other diseases accompanied by the destruction of cardiomyocytes.
- Myoglobin. A protein similar in structure to hemoglobin and responsible for the deposition of oxygen in muscle tissue, including the heart muscle. It increases when muscle tissue is damaged, in the first hours after myocardial infarction.
- Alanine aminotransferase (ALT). An enzyme that is found primarily in the liver, as well as in skeletal muscles, kidneys and myocardium. An increase in ALT indicates liver damage, but may also indicate myocardial infarction and serves as an indicator of the extent of damage to the heart muscle.
- Aspartate aminotransferase (AST). This enzyme is found mainly in the myocardium, skeletal muscles, and liver. An increase in AST levels is a sign of myocardial infarction. The AST value corresponds to the degree of damage to the heart muscle.
- Generic creatine kinase. An enzyme involved in energy metabolism reactions. Its different isoforms are found in different tissues of the human body. An increase in the level of total creatine kinase is observed in myocardial infarction and myopathies.
- Creatine kinase MB. An isoform of creatine kinase, which is found mainly in the myocardium and tissues of the nervous system. Its level corresponds to the extent of myocardial damage.
- Lactate dehydrogenase (LDH) total. An enzyme that is involved in energy metabolism and is found in almost all tissues of the body. Different types of LDH are present in different organs. Total lactate dehydrogenase may be elevated in myocardial infarction and liver disease.
- Lactate dehydrogenase 1, 2 (LDH 1, 2 fractions). These are types of lactate dehydrogenase, the increase of which is a more specific indicator of myocardial and kidney damage.
- Lipase. Pancreatic enzyme. Increased lipase levels are specific to pancreatic diseases.
- Total cholesterol. This is the main indicator of fat metabolism in the body. Used to diagnose atherosclerosis and liver diseases.
- D-dimer. Fibrin breakdown product. It is an indicator of fibrinolytic activity of the blood. The level of D-dimer may change with pulmonary embolism, dissecting aortic aneurysm.
- The main blood electrolytes are potassium, sodium, chlorine, calcium. Changes in the level of blood electrolytes may indicate pathology of the kidneys, adrenal glands, endocrine diseases, and malignant neoplasms.
- Urea, serum creatinine. These are the end products of nitrogen metabolism, which are excreted from the body by the kidneys. Their increase may indicate kidney pathology.
Instrumental research methods
- Electrocardiography (ECG). Changes in the ECG are detected during myocardial infarction, angina pectoris, and pericarditis. Helps determine the location and extent of myocardial damage.
- X-ray, computed tomography (CT), magnetic resonance imaging (MRI), ultrasound examination of the chest organs. These are imaging methods that allow you to assess the condition of the chest organs, identify injuries, neoplasms, signs of internal bleeding and other pathological changes.
- Transesophageal echocardiography. An ultrasound examination in which a probe is inserted into the esophagus. With its help, the condition of the heart, its valves, and large vessels is assessed. It has great diagnostic value for pulmonary embolism and aortic aneurysm.
- Angiography. X-ray examination of blood vessels using a non-toxic contrast agent, clearly visible on the images. Allows you to assess the condition and patency of blood vessels, including coronary ones.
Treatment
Treatment depends on the underlying disease, the symptom of which is chest pain. Therapy can consist of both the use of appropriate medications and surgical procedures.
Prevention
There is no specific prevention for most diseases accompanied by chest pain. However, to reduce the risk of their development, quitting smoking and alcohol, sufficient physical activity, a healthy diet, and timely preventive medical examinations are useful.
Recommended tests
- General blood analysis
- Erythrocyte sedimentation rate (ESR)
- C-reactive protein (quantitative)
- NT-proBNP (quantitative)
- Troponin I
- Myoglobin
- Alanine aminotransferase (ALT)
- Aspartate aminotransferase (AST)
- Creatine kinase total
- Creatine kinase MB
- Lactate dehydrogenase (LDH) total
- Lactate dehydrogenase 1, 2 (LDH 1, 2 fractions)
- Lipase
- Total cholesterol
- D-dimer
- Serum potassium
- Serum sodium
- Chlorine in serum
- Serum calcium
- Urea in serum
- Serum creatinine
- Laboratory diagnosis of acute coronary syndrome and myocardial infarction (optimal)
Prevention recommendations
- Warm up more often, do physical exercise, swimming, yoga or fitness;
- Try to keep your back straight while walking and sitting;
- Avoid drafts, hypothermia, do not swim for a long time even in warm water;
- Avoid excessive physical exertion and lift heavy objects;
- Avoid sharp turns and bends;
- Avoid stressful situations, overwork;
- Monitor your diet and weight;
- Give up bad habits: smoking and alcohol;
- Get a preventative checkup every year.
How to relieve pain. First aid
Often a person who has pain in the middle of the chest does not know what to do in such a situation. Some people experience so much pain that they faint. In this case, severe fear is observed, the pulse rate increases, and the skin turns pale. The first thing to do if a person suddenly experiences severe pain in the sternum, internal organs and spine:
- call an ambulance;
- put the person in bed, slightly raising his legs;
- remove clothes that constrict the chest and interfere with breathing, give a nitroglycerin tablet, which will dilate the blood vessels and improve the condition of the victim.
Also, if a person has pain in the middle of the chest, it is best to ask everyone present to leave the room and ensure complete rest for the patient until the ambulance arrives.