Headache can be a symptom of many serious diseases. Intracranial hypertension is an increase in intracranial pressure due to head injuries, hemorrhages, inflammation of brain tissue and the development of tumors.
To avoid complications, you need to promptly seek help from the Yusupov Hospital, where the pathology will be diagnosed and treated.
The quality of services provided in the hospital is at the European level. All diagnostic and treatment procedures are performed using the latest medical equipment. The rooms are equipped with maximum comfort for patients.
Do not put off going to the doctor and for any manifestations of increased intracranial pressure, seek help from highly qualified doctors at the Yusupov Hospital.
general information
In recent years, the frequency of cases of ICP in childhood has increased sharply, but this is due to the development of examination methods, which has led to overdiagnosis based on indirect symptoms. It is important to understand that intracranial hypertension cannot be an independent diagnosis and is only one of the signs.
In children, due to the structural features of the cranium, pressure inside the skull is a relative concept, and even the identification of signs of pathology on ultrasound without the presence of other symptoms does not indicate the presence of the disease. Any deviations in the structure inside the head may be normal if there are no complaints or signals of brain damage.
Intracranial hypertension
Intracranial hypertension, or increased intracranial pressure, is a dangerous syndrome that can be fatal. A syndromic diagnosis is established by a neurologist using examination and additional research methods. Increased intracranial pressure requires immediate and adequate treatment.
Unfortunately, in our country, this diagnosis is often made without any reason by everyone who is in any way connected with the examination of the head: ophthalmologists, therapists, radiologists. Intracranial hypertension is diagnosed both in adults and children, right and left. In this case, treatment is prescribed (mainly vascular drugs), which, naturally, does not lead to a cure. Often at an appointment you can hear that the patient has been treated for intracranial hypertension unsuccessfully since childhood and has been taking courses of vascular medications all his life.
What is intracranial hypertension really?
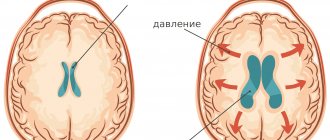
The skull is a closed space in which the brain, blood vessels, as well as cerebrospinal fluid (cerebrospinal fluid) and other structures are located. All these organs create a certain pressure inside the skull, which can fluctuate normally. Due to the fact that the bones of the skull in an adult are normally motionlessly connected, any increase in volume in the cranial cavity leads to an increase in pressure inside it. For example, intracranial pressure increases slightly when straining, then returns to normal values.
Certain medical conditions can cause blood pressure to rise or fall significantly, causing damage to structures inside the skull. For example, intracranial pressure slowly and steadily increases as a brain tumor grows. Since the bones of the skull are motionless and the tumor continues to grow, the volume of the contents of the skull increases, the pressure inside increases, the brain and blood vessels are displaced or compressed. All this leads to irreversible consequences and even death.
Intracranial pressure can rise very quickly with a cerebral hemorrhage or severe meningitis. In this case, emergency measures are required. A sudden decrease in intracranial pressure is also dangerous, as it can cause the brain to wedge into the bony openings of the skull and cause rapid death.
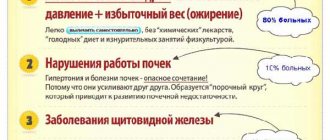
There is another type of hypertension - benign intracranial hypertension. The peculiarity is that the cause of the increase in pressure cannot be found; the disease may go away on its own. However, benign intracranial hypertension is a fairly rare disease. It is known that women are more likely to suffer from it, especially during pregnancy or if they are overweight.
What symptoms may bother you?
If the pressure changes smoothly, the patient may have various complaints. Among them, the most common are headache and vomiting in the morning or after being in a horizontal position. Sometimes blurred vision and double vision occur. Infants may have a bulging or retracted fontanel. The remaining symptoms are nonspecific: weakness, irritability, in children - a sharp cry, etc.
If the pressure inside has changed sharply, then most likely the person will be unconscious in a serious condition.
Research methods
First of all, I would like to say that intracranial pressure can only be measured by opening the skull. To date, there are no other methods for accurately measuring intracranial pressure. A stable change in pressure (mostly an increase) can be assumed using the following methods:
- Examination by a doctor to assess the movements of the eyeballs
- the patient may have strabismus due to compression of the abducens nerve, double vision while checking the range of movements of the eyeballs. In children, head circumference may increase. Pathological neurological symptoms, associated, for example, with a tumor, may be observed. - Fundus examination
- there may be blurred optic disc, vascular congestion and other nonspecific signs. - X-ray of the skull
- so-called “finger impressions” and other nonspecific signs may be visible. - MRI and CT of the head
- “empty sella” syndrome, dilatation of the ventricles of the brain and other nonspecific signs. - Ultrasound of the vessels of the head and neck
- there may be a violation of the venous outflow from the cranial cavity.
All these data must be assessed in combination, because each of them separately does not allow establishing the syndrome of intracranial hypertension. To make a diagnosis, you must also visit at least a neurologist and an ophthalmologist.
Unfortunately, there are often cases when, based on an examination by one specialist or based on the results of a single study, intracranial hypertension syndrome is established and treatment is prescribed. In most cases, headaches and visual disturbances are caused by completely different reasons (tension headaches, migraines, cervicocranialgia, etc.).
Treatment of intracranial hypertension
Treatment of intracranial hypertension depends on the cause of the syndrome.
And remember that real intracranial hypertension cannot be treated with vascular, nootropic drugs, physiotherapy and massage! This is a serious condition. This often requires hospitalization in the intensive care unit and emergency assistance from a neurosurgeon.
Be healthy!
Maria Meshcherina
Photo istockphoto.com
Signs of ICP in a child
Visible symptoms of increased intracranial pressure in children under one year of age may include:
- constant monotonous crying;
- swelling of the fontanelle;
- vomiting like a fountain;
- persistent anxiety of the baby;
- sleep disorder;
- decreased appetite;
- convulsions;
- the appearance of convergent strabismus;
- an increase in head circumference against the background of divergence of the skull bones.
Individually, these signs cannot indicate the presence of ICP, but in combination, especially with neurosonography data, which can illustrate the systematic growth of the ventricles of the brain, they indicate obvious hypertension.
Symptoms of high intracranial pressure in children over one year of age may include:
- bouts of vomiting, which brings temporary relief;
- constant nausea not associated with eating;
- confusion and even loss of consciousness;
- unmotivated irritability;
- lethargy, general weakness;
- dizziness;
- severe headaches without clear localization that do not go away after taking painkillers or subside for a short time;
- convulsive conditions;
- decreased visual acuity;
- lethargy;
- papilledema during ophthalmological examination;
- feeling of fog before the eyes after bending over.
In adolescents, additional symptoms of increased intracranial pressure may include unmotivated aggression, deterioration of memory and attention, excessive emotionality, and moodiness. Children may complain of difficulty falling asleep and waking up in the morning, attacks of apathy, and paroxysmal pain in the head at night.
Symptoms
The basis of the clinical picture of intracranial hypertension is headache, pressing on the eyes. In an acute course, its intensity quickly increases; in a chronic process, unpleasant symptoms are not so pronounced, pain occurs periodically.
Patients also complain of nausea, which with severe pain can turn into vomiting, and discomfort when moving the eyes. Acutely increasing intracranial hypertension can lead to loss of consciousness and even coma.
In a chronic course, the general condition of a person suffers. Sleep is disturbed and irritability appears. Patients note fatigue and weather dependence. They periodically experience liquor-hypertensive crises, characterized by intense headaches, nausea, vomiting and even loss of consciousness.
Idiopathic intracranial hypertension most often causes transient visual disturbances (double vision, blurring, decreased sharpness).
In children whose intracranial pressure increases, their behavior changes. They become restless, whiny, often burp and refuse to eat. One of the specific symptoms is bulging fontanel. The chronic course of the pathology can lead to mental retardation, even mental retardation.
Causes of pathology
In the first months of life, the main role in the formation of ICP is played by infections suffered by the baby during intrauterine development. These include rubella, herpes, syphilis, as well as malformations of the central nervous system. In some cases, the cause of changes in intracranial pressure in children under one year of age is birth trauma. Experts also associate ICP with prematurity and oxygen starvation of the baby during childbirth.
Common factors that can cause ICP are:
- various non-infectious brain lesions;
- acute neuroinfections;
- hydrocephalus;
- benign and malignant neoplasms (tumors, cysts);
- cerebrovascular accident due to thrombosis, hematopoietic diseases;
- traumatic brain injury;
- acute poisoning;
- abnormalities of brain development;
- hormonal pathologies;
- pathologically early closure of the fontanel;
- obesity;
- long-term use of certain medications;
- abrupt cessation of treatment with certain medications.
Uncontrolled increased intracranial pressure can lead to irreversible changes in the child’s nervous system, depression of cognitive functions, disorders of the respiratory and cardiovascular systems, mental retardation, asthenic syndrome and death.
Pediatric hypertension: signs and treatment
Pediatric hypertension: signs and treatment
Arterial hypertension
- a pathology manifested by an increase in blood pressure. The increase is permanent. It can be constant or have a crisis course. In children, blood pressure depends on age, gender, weight and height. Recently, cases of hypertension in children and adolescents have been increasingly recorded. There are many factors influencing the development of pathology. The risk of developing hypertension in a child increases if close relatives have similar problems. Such pressure is a reason for dispensary monitoring of children and inclusion of them in the risk group for the hypertensive process.
Arterial hypertension in children occurs in every tenth preschooler and every 6th schoolchild. Children in the first years of life rarely suffer from arterial hypertension. Typically, such hypertension develops as a secondary symptom of other diseases. Most often, arterial hypertension develops in adolescents during puberty. This is explained by the vegetative and hormonal disruptions that occur during this period.
There are two forms of arterial hypertension in children and adolescents:
- Primary hypertension in children:
- Secondary form of pathology:
Primary hypertension
occurs in the absence of a clear cause of the disease, develops due to many reasons:
- heredity;
- chronic stress, emotional tension;
- child's temperament;
- increased weight;
- metabolic failures;
- excess salt in food;
- dysregulation of homeostasis systems in the brain
Secondary hypertension
: the disease develops against the background of concomitant diseases of the cardiovascular system, abnormalities of the thyroid gland, adrenal function and other diseases. Rare pathologies that can cause arterial hypertension: systemic vasculitis, connective tissue diseases, brain pathologies; hypertensive-hydrocephalic syndrome.
Moderate arterial hypertension in children is characterized by the following symptoms:
- Weak symptoms or absence of external symptoms. Parents may not be aware of their child’s illness.
- Increased blood pressure (systolic component). In children of the first year of life, up to 110 mm Hg. Art., at 10 years old up to 125 mm Hg. Art., in adolescents more than 135-140 mm Hg. Art.
- Headache, fatigue.
- Often these children have increased weight.
- Vegetative failures.
- Congenital microanomalies of the heart and kidneys.
The main risk factors for arterial hypertension in children and adolescents include:
- impressionability, emotional and psychological excitability;
- overweight, tendency to obesity, unhealthy diet;
- excessive salt intake;
- inactive lifestyle, frequent watching of TV and computer.
Diagnosis and treatment methods
The final diagnosis of arterial hypertension in children and adolescents is made after a threefold increase in blood pressure is detected. The first symptoms and signs of the disease can be detected during a regular medical examination with a doctor. Pathological changes are confirmed after daily monitoring of pressure and taking tests with physical and psycho-emotional stress.
Self-prescribing medications for children is strictly prohibited.
. The dosage and type of medicine can only be prescribed by a doctor, based on examination, test results and examinations.
Preventive measures
Prevention of arterial hypertension due to its significant prevalence should be carried out by everyone, regardless of age. The main activity in this case is the formation of the habit of leading a healthy lifestyle in children and adolescents. Parents should maintain a proper daily routine, provide a healthy and nutritious diet, good, restful sleep, an adequate work and rest schedule, and a healthy diet help avoid the occurrence of arterial hypertension. At older ages, it is necessary to exclude risk factors that influence the development of the disease. A favorable and calm emotional environment should be maintained in the family. Children and teenagers should be taught from an early age to walk in the fresh air and have an active lifestyle. Adults should supervise television viewing and computer gaming time. If there is a hereditary predisposition to the development of hypertension, it is recommended to regularly measure blood pressure in children and adolescents using a special device - a tonometer. If deviations from the norm are detected in a timely manner, the likelihood of recovery increases.
The appearance of the first symptoms of increased blood pressure in children and adolescents should not go unnoticed. Excessive nervousness, moodiness, and fatigue indicate the presence of certain health problems. If treatment is started on time, the risk of developing chronic hypertension and serious complications in older age is significantly reduced . A healthy lifestyle, proper nutrition and the absence of bad habits serve as preventive measures for the development of diseases of the cardiovascular system in children and adolescents.
Monitoring blood pressure and regular examinations with a doctor will help identify problems at an early stage and successfully treat the child.
Treatment
There is no such thing as treatment for intracranial pressure in either children or adults. The goal of therapy is to eliminate the pathology that provoked hypertension, relieve symptoms and eliminate predisposing factors. Treatment directly depends on the cause of the condition and can be conservative or surgical.
The complex of conservative therapy includes various medications:
- antibacterial, anti-inflammatory, antiviral and antiparasitic drugs to eliminate neuroinfections;
- diuretics, the action of which is aimed at preventing cerebral edema;
- nootropics that help preserve cognitive functions;
- sedatives that help reduce the manifestations of psychoneurological disorders;
- injectable vitamins that improve the functioning of the central nervous system.
In cases where conservative tactics do not bring the expected results or the disease cannot be eliminated with medications, surgical treatment is indicated. Depending on the urgency and purpose of the intervention, bypass surgery, external ventricular drainage and decompressive craniotomy are performed.
The prognosis for diseases that provoke ICP depends on the nature of the pathology and the speed of diagnosis. In general, with timely and adequate complex therapy, the likelihood of an unfavorable outcome is greatly reduced.
Causes of the disease
The internal cavity of the skull is a closed space. If cerebrospinal fluid accumulates excessively in this area, there is nowhere for the tissue to move. Areas of the brain are compressed, displaced relative to their original position, and blood vessels are compressed, which leads to critical changes in living fibers and cessation of normal blood flow. Internal pressure is considered normal from 7.5 to 15 mmHg. Exceeding the specified values by up to 30 mm RS can lead to death.
The following factors lead to the development of ICH:
- congenital developmental anomalies;
- extensive infection, previous meningitis;
- tumor formations in the brain;
- stroke;
- delay in normal fluid outflow (hydrocephalus);
- penetration of the encephalitis virus into tissue;
- post-traumatic hematomas;
- internal hemorrhages;
- high level of blood clotting;
- diseases in the cervical spine;
- large body weight;
- intoxication with alcohol or medications.
Prevention of increased intracranial pressure in children
Careful planning of pregnancy, delivery and regular monitoring of the expectant mother, including fetal monitoring, help to significantly reduce the risk of developing diseases associated with intracranial hypertension. Prevention of dangerous infectious diseases through vaccination plays an important role.
Parents also need to ensure that their children follow a daily routine, get enough sleep, and are not exposed to nervous or physical exhaustion. It is important to explain to children the danger that bruises and falls pose, to provide them with the necessary equipment for riding a bicycle or scooter, and not to leave them unsupervised in places where they can get injured. Specialists at the SM-Doctor clinic will conduct a comprehensive examination of the child at the slightest suspicion of increased intracranial pressure and prescribe the most effective treatment and rehabilitation measures if necessary.
Diagnostics
Because intracranial pressure can fluctuate, there is no consensus on what is normal. It is quite difficult to make a diagnosis. The patient is prescribed a special examination, during which he undergoes:
- echo-encephalography;
- examination by an ophthalmologist, who reveals swelling of the optic nerves during ophthalmoscopy;
- X-ray of the skull, where “finger impressions” that arise during chronic conditions are visible.
However, the most reliable methods for diagnosing intracranial hypertension are lumbar puncture and puncture of the cerebral ventricles.
To identify the causes of increased intracranial pressure, MRI, CT, MSCT of the brain are prescribed, as well as vascular ultrasound and stereotactic biopsy of identified tumors.
Treatment options
Treatment tactics are structured as follows: eliminating the root cause of the disease, accelerating the natural outflow of cerebrospinal fluid, relieving symptoms. If hypertension is a temporary complication of any other disease, manual therapy is prescribed to help restore normal blood circulation. At the same time, the drinking regime is regulated and a set of exercises is prescribed to relieve pressure inside the head.
More complex anomalies require a course of medications aimed at accelerating the absorption of fluid and its removal to the outside. The basis of drug therapy is diuretics. In some cases, long-term or permanent (lifelong) use of such drugs is required.
In critical cases, when the disease poses a direct threat to life, surgical treatment is performed. If there is a tumor blocking the outflow of cerebrospinal fluid, the possibility of its removal is considered. To urgently reduce pressure, shunts are inserted into the skull to drain excess fluid.