Perineal varicose veins are varicose veins in the perineal area (varicose veins of the labia, varicose veins of the perineum), developing due to obstruction of venous outflow. Varicose veins of the labia are a manifestation of impaired outflow through the system of internal iliac veins due to their blockage or compression. The mere presence of signs of varicose veins of the labia does not pose a threat to the patient’s life, but is aesthetically unacceptable for young women, complicates sexual life and may indicate serious circulatory disorders in the pelvis.
Predisposing factors in the development of genital varicose veins in women
Varicose veins on the labia have a genetic predisposition - the mechanism of the disease is similar to varicose veins of the lower extremities. The basis is dysfunction of the valves of the gonadal veins. Physical activity, frequent pregnancies, engorgement of the genital organs during prolonged sexual intercourse contribute to vascular stretching with the development of venous stagnation. The appearance of varicose veins of the labia during pregnancy usually occurs in the second trimester and reaches a maximum closer to childbirth. After childbirth, these varicose veins, which developed during pregnancy on the labia, most often regress, but sometimes remain for life due to changes in the structure of the vascular walls.
Diagnosis of uterine varicose veins
If uterine varicose veins are suspected, the doctor should refer the woman for examination. In modern medicine, various diagnostic methods are used for this:
- radiography;
- Ultrasound using a transvaginal sensor (echography);
- laparoscopy;
- Doppler ultrasound;
- CT scan.
Progressive diagnostic methods used in well-equipped clinics eliminate inaccurate diagnoses.
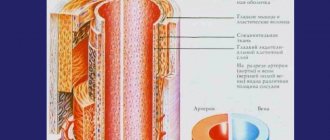
Arteriovenous compression
- Aorto-mesenteric compression of the left renal vein
Aorto-mesenteric compression of the left renal vein (aorto-mesenteric “tweezers”, nutcracker syndrome, mesoaortic compression syndrome of the left renal vein) is a situation in which the left renal vein is compressed between the aorta and the superior mesenteric artery. This leads to disturbances in the outflow of blood in the left renal vein, expansion and formation of “reverse” blood flow through the left gonadal vein with the formation of symptoms of varicose veins of the female genital organs.
- May-Turner syndrome
May-Turner syndrome is a situation in which the left common iliac vein is compressed by the right common iliac artery, leading to expansion of the common iliac vein below the site of compression and overflow of the pelvic vessels with venous blood. We also often observe the development of varicose veins - expansion of the left lower limb, the formation of persistent swelling of the soft tissues of the left lower limb and even trophic disorders (pigmentation). Most often, with May-Turner syndrome, varicose veins on the outer labia develop during pregnancy and remain forever after pregnancy (photo).
- Postthrombotic disease
Quite often one can observe the development of pelvic varicose veins in patients who have previously suffered deep vein thrombosis (especially proximal thrombosis) when there is a residual narrowing of the lumen or complete occlusion of the lumen of the common iliac vein. In this case, the outflow of blood from the pelvic organs is sharply hampered and, as a consequence, the expansion of the lumen of blood vessels and the development of pelvic varicose veins.
- Venous dysplasia
This is a malformation of the superficial or deep veins that occurs in the early phases of the formation of the vascular system of the embryo in the period from 4 to 8 weeks of intrauterine development. Venous dysplasia leads to the appearance of varicose veins of the minor lips. The diagnosis of dysplasia can be established provided that other causes of dilation of the genital vessels are excluded. Dysplasias look like dense vascular spots that are difficult to empty when squeezed. They resemble tumor-like formations more than dilated varicose veins.
Vulvar and perineal varicose veins in pregnant women
Journal "Outpatient Surgery" No. 1-2, 2019
DOI: https://doi.org/10.21518/1995-1477-2019-1-2-14-18
Jenina O.V.
1, Ph.D., phlebologist, leading specialist,
Bogachev V.Yu.
1,2, Doctor of Medical Sciences, Professor of the Department of Faculty Surgery No. 2,
Bodanskaya A.L.
1, phlebologist, lymphologist
1 Limited Liability Company "First Phlebological Center"
2
Federal State Budgetary Educational Institution of Higher Education “Russian National Research Medical University named after N.I.
Pirogov" Pregnancy is an important specific risk factor for the development of chronic venous diseases in women. In addition to the superficial veins of the lower extremities, the transformation often affects the veins of the small pelvis. The tactics of managing pregnant women with dilated veins of the perineum and genitals is currently one of the pressing problems at the intersection of phlebology and obstetrics-gynecology. The article discusses possible options for conservative treatment of women with vulvar and perineal varicose veins during pregnancy, including a discussion of the possibility and feasibility of using systemic pharmacotherapy with venoactive drugs.
Vulvar and perineal varicose veins in pregnant women
Olga V. Dzhenina
1,
Vadim YU. Bogachev
1,2,
Antonina L. Bodanskaya
1
1 First Phlebological Center, Limited Liability Company, 2 Federal State Budgetary Educational Institution of Higher Education “Russian National Research Medical University named after NI Pirogov” of the Ministry of Health of the Russian Federation
Pregnancy is an important specific risk factor for the development of chronic vein diseases in women. In addition to the superficial veins of the lower limbs, transformation often affects the pelvic veins. The management of pregnant women with vulvar and perineal varicose veins is one of the urgent problems of nowadays at the intersection of phlebology and obstetrics-gynecology. The article discusses possible options for conservative treatment of women with vulvar and perineal varicose veins during pregnancy, including the possibility and feasibility of using systemic venoactive drugs.
One of the most significant risk factors for the development of chronic venous diseases (CVD) in women is pregnancy. The cause is physiological changes that occur in absolutely all pregnant women, begin to act from the earliest gestational stages and gradually increase their influence in parallel with the progression of pregnancy.
Among the prerequisites currently being considered are:
— hormonal
in the form of a progressive increase in the level of progesterone, which provokes the destruction of collagen and elastin fibers, leading to disruption of the architectonics of the venous wall and a decrease in the ability to maintain a constant diameter of the vessel; are implemented throughout the entire gestational period;
— mechanical
– an increase in the volume of circulating blood, intra-abdominal pressure and direct compression of the main veins of the small pelvis by the pregnant uterus, which together leads to an increase in intravenous pressure; become important in the II–III trimesters [1–3].
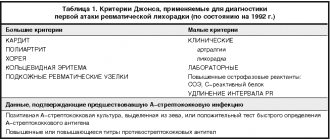
These predictors lead to the fact that even the first, uncomplicated pregnancy itself gives an odds ratio of at least 1.3 for varicose transformation, and with each subsequent pregnancy this indicator increases (Table 1). In cases where, in addition to pregnancy, a woman has additional risk factors for CVD - heredity, excess body weight, etc. - an additional increase in the odds ratio should be expected [4].
Table. The relationship between the number of pregnancies and varicose transformation [4]
| Number of pregnancies (B) | B = 1 | B = 2 | B = 3 | B = 4 | B ≥5 |
| Odds ratio | 1,3 | 1,4 | 1,6 | 1,9 | 2,2 |
The venous bed of both the pelvis and the lower extremities is affected, while at first glance, varicose transformation of the superficial veins of the lower extremities is more common. The incidence of pelvic varicose veins during pregnancy has not yet been fully assessed. According to the literature, isolated dilatation of the veins of the perineum and genitals occurs in only 10–12% of pregnant women. At the same time, a number of experts suggest that a certain number of patients are not taken into account due to the lack of complaints from the women themselves: due to mild or absent subjective symptoms, shyness of patients, etc. [5–7].
The prevalence of gestation-related dilatation of intrapelvic veins is also not taken into account. First of all, this can be explained by the absence of any external manifestations that the patient could notice and eventually see a doctor. Secondly, there is a certain difficulty in assessing the clinical probability of pelvic congestion syndrome in such patients, since the most common manifestations - bursting pain in the lower abdomen, dysuric disorders - may be due to the peculiarities of the course of pregnancy.
Varicose veins of the perineum and genitals have objective manifestations that make it possible to diagnose this variant of venous pathology already during the initial examination, often without requiring mandatory instrumental confirmation. First of all, there is a direct expansion of the superficial veins with the appearance of aneurysmal protrusions-varixes on the labia, in the perineum. With a small volume, this is most often the woman’s only complaint. Subsequently, symptoms appear that can be regarded as similar to chronic venous insufficiency of the lower extremities: patients note bursting, pulling and pressing sensations in the perineum, bursting pain directly in the projection of varix. Many pregnant women note an increase in pain not only in situations standard for CVD - at the end of the day, under static loads - but also when changing body position (lying down/sitting down, sitting/standing up), tension in the muscles of the abdominal wall and pelvic floor. Also, the pain syndrome may be accompanied by dysuric symptoms, itching, and rarely, swelling of the perineum.
In cases where the source of reflux is not only the intrapelvic veins, but also v.saphena magna, dilatation of the veins in the inguinal areas is observed (with a small size of the varix, if it manifests itself only in orthostasis, this can be mistakenly regarded as an inguinal hernia), and also in the area of suprapubic flow [7].
Is instrumental examination required?
In most cases, examination is sufficient to make a diagnosis. An instrumental examination - angioscanning - is required if there is a clinical suspicion of thrombosis of the dilated superficial vein of the perineum/genitals, namely: a palpable painful compaction along the vein with a change in the color of the skin or mucous membrane above it. Ultrasound angioscanning is necessary to confirm a more dangerous condition - thrombosis - which requires completely different tactical approaches.
The second clinical situation in which it is advisable to conduct angioscanning, as well as ultrasound examination of soft tissues, is the differential diagnosis between a single varix in the groin area and an inguinal hernia.
What can we offer today to a pregnant woman who has been diagnosed with vulvar or perineal varicose veins?
The expert community currently considers pelvic varicose veins as one of the forms of CVD; accordingly, the basic principles of treatment apply to this pathology, although they require certain restrictions taking into account the location of the problem vein, and in pregnant women, taking into account the potential effects on the developing fetus.
Conservative treatment of CVD is based on elastic compression, systemic pharmacotherapy with venoactive drugs, local pharmacotherapy using topical heparin-based agents and venotonics, as well as lifestyle modification [8].
Elastic compression has long been a fundamental component of the conservative treatment of CVD. Thanks to medical compression hosiery and special bandages, pathological venous capacity is reduced, venous blood reflux and interstitial edema are eliminated, microcirculation in soft tissues is improved, etc. [9–11]. Thanks to this, even compression class 1 knitwear is effective in eliminating the subjective symptoms of CVD and venous edema [13–15].
However, all these therapeutic effects cannot be realized with isolated vulvar or perineal varicose veins, since not a single ready-made compression product, even special tights for pregnant women, puts pressure on the perineal area. The use of special compression garments, which are used after plastic surgery (such as abdominoplasty, liposuction, etc.), is contraindicated in pregnant women due to high pressure on the anterior abdominal wall, which can negatively affect the course of pregnancy itself.
The only situation in which regular wearing of compression products is justified is the simultaneous presence of CVD of the lower extremities.
The second main direction in the conservative treatment of chronic venous disease is systemic pharmacotherapy with phlebotropic drugs, the main goal of which is to reduce subjective manifestations and venous edema. Venotonics act through norepinephrine-dependent mechanisms and can additionally reduce leukocyte-endothelial adhesion and capillary permeability, stimulate lymphatic drainage, and reduce specific venous pain [8, 9, 16, 17]. One of the indications for the use of venotonics is varicose veins of the small pelvis with pain. But until recently, pregnancy was considered as a condition that limited the possibility of such pharmacotherapy.
There are several reasons for this:
- a small number of studies on the safety and effectiveness of venotonics during pregnancy; - reluctance to use essentially symptomatic treatment for a non-life-threatening condition in pregnant women, when it is necessary to take into account the potential effect of the active substance on the fetus; — underestimation of the prevalence of the problem and its impact on the quality of life of pregnant women.
Despite periodic reports of the use of venotonics for gestational dilatation of the vulvar veins [7], the opportunity to reconsider approaches to the use of phlebotropes in pregnant women was provided by the EFEMERIS epidemiological study, which assessed the possible direct and indirect effects of various pharmaceuticals not only on the development of the fetus, but also the course of pregnancy and delivery itself. [18]. The main group consisted of 8998 women who took diosmin, troxerutin and hesperdin during pregnancy, and some of them used repeated courses of venotonics. The control group included 27,962 pregnant women who did not take such drugs. Analysis of the course and outcomes of pregnancies showed the absence of a negative effect of the above venotonics on the course of pregnancy, delivery and the postpartum period, as well as fetal development.
Considering the encouraging results of EFEMERIS, the ineffectiveness of the routine use of elastic compression, the specific analgesic effect of modern phlebotropes, the use of diosmin-containing drugs in pregnant women with pain due to perineal/vulvar varicose veins seems justified and appropriate.
We have our own experience with the use of venoactive drugs: we observed 192 women with vulvar and perineal varicose veins during the second and third trimesters of pregnancy. Due to bursting pain in the perineum and along the varicose veins with an intensity ranging from 5 to 8 points on a ten-point numerical rating scale (Numeral Rating Scale, NRS), the patients received diosmin 600 mg/day. The duration of continuous use of diosmin ranged from 2 to 10 weeks, 11 patients underwent two courses of therapy (8 weeks each with an interval of 4 weeks between courses). Among 129 women with pain of moderate intensity (5-6 points according to NRS), 47.29% noted complete relief of pain, in other cases - a decrease in intensity by 2 points or more. In almost a third (27%) of 63 women with severe pain (5-6 points on NRS) while taking diosmin 600 mg/day, a decrease in its intensity by 2 points or more was recorded, but complete relief of pain in this subgroup was not achieved. None of the 192 patients had any complications of pregnancy, childbirth or the postpartum period that could be associated with taking venotonics. During vaginal birth, spontaneous rupture of varixes was not observed. There were no births of children with congenital malformations in these women who took diosmin at a dosage of 600 mg/day during pregnancy.
Russian guidelines for the treatment of CVD recommend an individual approach when prescribing venotonics in pregnant women, with an assessment of the ratio of expected benefits for the mother and potential effects on the fetus [8].
In contrast to systemic pharmacotherapy, the use of topical heparin-based agents or venotonics for vulvar or perineal varicose veins does not seem appropriate to us:
- distraction therapy, - short duration of effect, - peculiarity of the localization of problem veins, high probability of gel or ointment getting into the vaginal mucosa with a potential adverse reaction.
Lifestyle modification remains relevant for this category of patients.
It seems to us that the following emphasis is appropriate:
1.
prevention of additional increase in intra-abdominal pressure, i.e.
prevention of constipation: physical activity, balanced diet with vegetables, cereals, fiber, sufficient fluid intake; 2.
prevention of pathological weight gain;
3.
use of support bandages in consultation with an obstetrician-gynecologist.
What other features does the management of pregnant women with vulvar and perineal varicose veins have? Both the women themselves and the obstetrician-gynecologists observing them can contact a phlebologist to assess the possibility of vaginal birth. In the vast majority of cases, such localization of varicose veins does not affect delivery tactics. The risk of spontaneous rupture of varixes and, accordingly, the risk of bleeding during childbirth can only be represented by very large, tense (not compressed upon palpation) varixes that extend to the vaginal walls. In this case, delivery tactics are determined together with an obstetrician-gynecologist; when determining the high risk of large perinatal blood loss, one can think about the advantages of a planned cesarean section. It should be taken into account that in the prenatal period, even with a slight change in the position of the fetus in the uterus, varix can become relaxed and the risk of hemorrhagic complications will decrease [19].
In the early postpartum period, varicose veins of the perineum and genitals quickly regress in the vast majority of patients. Recurrences of this condition are usually associated only with repeat pregnancies. Even if complete regression does not occur, the volume of dilated veins and the associated discomfort are significantly reduced. In the future, residual vulvar/perineal varicose veins can be eliminated using miniphlebectomy or scleroobliteration.
conclusions
Isolated vulvar and perineal varicose veins are not a life-threatening condition, but the associated pain syndrome worries pregnant patients and leads to a certain decrease in quality of life. Yes, none of the forms of CVD can be completely eliminated with the help of conservative treatment, but the use of systemic pharmacotherapy can reduce subjective manifestations, including venous pain. This leads to an improvement in the quality of life of patients, which is especially significant in cases where radical surgical intervention is impossible for a number of reasons, including pregnancy. We see the advisability of more active use of modern diosmin-containing phlebotropes, which have proven the absence of negative effects on the course of pregnancy and fetal development, in pregnant women with varicose veins of the small pelvis in the event of the formation of a specific pain syndrome. Also, in our opinion, there is a need for further monitoring of such patients outside of pregnancy with planned elimination of residual dilated veins using minimally invasive methods (sclerotherapy, miniphlebectomy, laser thermoobliteration).
Sources
- International research program VEIN CONSULT. http:www.veinconsult.com.
- Savelyev V.S., Kirienko A.I., Bogachev V.Yu. Chronic venous diseases in the Russian Federation. Results of the international research program VEIN CONSULT. Phlebology. 2010;4(3):9-12.
- Krajcar Dz., Radaković B., Stefanić L. Acta Med Croatica. 1998;52(1):65-69.
- Bromen K., Pannier-Fischer F., Stang A., Rabe E., Bock E., Jöckel K.-H. Should sex specific differences in venous diseases be explained by pregnancies and hormone intake? Gesundheitswesen. 2004;66(3):170-174.
- Dodd H., Wright HP Vulval varicose veins in pregnancy. BMJ. 1959;1:831-832.
- Van Cleef J.-F. Treatment of vulvar and perineal varicose veins. Phlebolymphology. 2011;18(1):38.
- Marhic S. Rev FR Gynecol Obstet. 1991;86(2/2):184-186.
- Russian clinical guidelines for the diagnosis and treatment of chronic venous diseases. Phlebology. 2013;7(2):2-47.
- Nicolaides A., Kakkos S., Eklof B. et al. Management of chronic venous disorders of the lower limbs. Guidelines according to scientific evidence. Int Angiol. 2014;33(2):87-208.
- Gloviczki P., Comerota AJ, Dalsing MC et al. The care of patients with varicose veins and associated chronic venous diseases: Clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2011; 53:2-48.
- Mariani F. (ed.). Compression. Consensus document based on scientific evidence and clinical experiences. Minerva Medica (Torino), 2009.
- Rybak Z. Management of lower-limb venous symptoms: what the guidelines tell us. MEDICOGRAPHIA. 2015;37:50-55.
- Partsch H., Flour M., Smith PC International Compression Club. Indications for compression therapy in venous and lymphatic disease consensus based on experimental data and scientific evidence. Under the auspices of the IUP. Int Angiol. 2008;27(3):193-219.
- Palfreyman SJ, Michaels JA A systematic review of compression hosiery for uncomplicated varicose veins. Phlebology. 2009;24(1):13-33.
- Flour M., Clark M., Partsch H., Mosti G., Uhl J.-F., Chauveau M. et al. Dogmas and controversies in compression therapy: report of an International Compression Club (ICC) meeting, Brussels, May 2011. Int Wound J. 2012;10(5):516-526.
- Nicolaides A., Allegra C., Bergan J. et al. Management of Chronic Venous Disorders of the Lower Limbs: Guidelines According to Scientific Evidence. Int Angiol. 2008;27(1):1-59.
- Perrin M., Ramelet A.A. Pharmacological treatment of primary chronic venous disease: rationale, results and unanswered questions. Eur J Vasc Endovasc Surg. 2011;41:117-125.
- Lacroix I., Beau AB, Hurault-Delarue C. et al. First epidemiological data for venotonics in pregnancy from the EFEMERIS database. Phlebology. 2016;31:344-348.
- Pratilas G., Dinas K. Severe Vulvovaginal Varicosities in Pregnancy. N Engl J Med. 2021 May;378(22):2123
Symptoms and complaints of perineal varicose veins
In the classic version, there is a triad of symptoms:
- Pelvic pain.
- Varicose veins of the labia and perineum.
- Dysmenorrhea is a cyclical process, when during menstruation severe pain in the lower abdomen, heavy menstrual bleeding, and menstrual irregularities may appear.
- With a long course of the disease, the development of dyspareunia is possible - painful sensations in the lower abdomen that occur during or after sexual intercourse. A peculiarity of this symptom is the persistence of pain for at least 30 minutes and up to a day after sexual intercourse.
Causes of development of varicose veins of the pelvis
Today, the main cause of varicose veins is considered to be a history of pregnancy. The situation arises due to the fact that the growing fetus puts pressure on nearby organs and vessels, disrupting blood circulation. A healthy female body after childbirth is able to restore blood circulation on its own and no problems arise. However, under the influence of certain provoking factors, the tone in the vessels is not restored, leading to vascular pathology.
Factors contributing to the occurrence of the disease:
- excessive physical activity;
- sedentary lifestyle;
- diseases of the reproductive system (tumors, polycystic disease, endometriosis, etc.).
It is worth noting that varicose veins of the venous vessels of the pelvis can occur not only during pregnancy. Recently, scientists have been actively discussing the effect of hormonal contraceptives and hormone-containing drugs on the development of venous pathology. This assumption is based on the fact that the disease occurs much more often in women of childbearing age, which means hormones play a major role in this process.
Disease prognosis
Varicose veins of the uterus and perineum are not a life-threatening disease. But it is important to note that the quality of life of patients is significantly reduced. In addition to aesthetic discomfort, large perineal phleboectasis can cause painful symptoms during menstruation and complicate sexual life. Sometimes varicose veins become inflamed, causing a lot of physical suffering to patients. You should not count on the therapeutic effect of ointments and tablets - such therapy is not effective, but only eliminating the causes of varicose veins and the venous nodes themselves using sclerotherapy or miniphlebectomy allows one to achieve excellent therapeutic and aesthetic results in all patients. At the Innovative Vascular Center, complete treatment of this disease is possible. We successfully perform endovascular correction of deep vein pathology, eliminate varicose veins of the small pelvis and venous vessels on the genitals.
Treatment of varicose veins of the uterus
Uterine varicose veins are treated in several ways. In the early stages of the disease, it is enough to undergo a course of medication, combining it with wearing compression garments and performing a set of physical exercises to improve blood circulation. Varicose veins during pregnancy sometimes go away after childbirth on their own without much effort.
In an advanced stage, when treatment does not bring results, surgery will be required. In particularly severe cases, the uterus must be amputated, but usually the disease can be cured simply by removing the problematic veins. The operation is carried out using various methods - it can be a conventional surgical or laser phlebectomy. The main thing is that healthy veins are not affected.
Diagnostics
Timely detection of the process of vascular dilatation increases the likelihood of its cure and prevention of relapses.
To diagnose pelvic varicose veins, doctors at our clinic use instrumental research methods. One of the most effective ways to detect the disease is ultrasonography. This method is carried out in conjunction with transvaginal and abdominal ultrasound, which allows specialists to obtain the necessary data for diagnosis. During ultrasonography, vascular dilation can be identified by multi-colored spots of irregular shape.
Another research method is laparoscopy. In this case, the presence of pathology is signaled by bluish-colored formations that have a thin, tense wall in the area of the uterine ligament or ovaries.
Recently, a modern diagnostic method – selective oophorography – has been gaining popularity. During the study, a contrast is performed on the patient's blood vessels, thanks to which the doctor is able to see any deviations in their structure.
A CT scan may also be performed. The method helps to see the vessels in the woman’s internal genital organs.
Pronounced discomfort during sexual intercourse and other unpleasant manifestations of the disease contribute to the deterioration of the psychosomatics of patients, which often causes diagnostic errors. The presence of a clear pathognomonic symptom, combined with the absence of signs of pathology of the pelvic organs during a traditional examination and manifestations of clear psychosomatic disorders, often leads specialists to think about the psychoneurological nature of the disease. As a result, instead of treating varicose veins, patients are prescribed consultations with sex therapists and psychotherapists.