According to statistics, 10% of all people show signs of thrombophlebitis. The disease is fraught with serious damage to the deep veins, which leads to life-threatening consequences, in particular, blockage of the pulmonary artery. Many people also develop chronic venous insufficiency, which can lead to blood poisoning and blockage of large veins. Thrombophlebitis can appear at a fairly early age, so it is advisable to know how this disease manifests itself. At the first suspicion and symptoms, you should consult a doctor. In turn, the CBCP Center for Circulatory Pathology offers qualified diagnosis and treatment of this disease.
What is thrombophlebitis
The formation of blood clots in the body is a fairly common process. Thrombophlebitis of the extremities is especially common. Most of them are absorbed, but the largest ones can partially or completely block the vessel or break off and migrate through the circulatory system until they clog a smaller vessel. It may turn out to be a vital vein, and then the patient will face serious consequences. Thromboembolism in the pulmonary artery can cause severe circulatory and respiratory disorders, which can only be treated in an outpatient setting. Fatalities are also common.
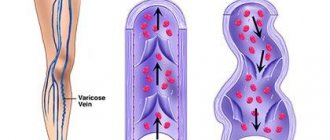
The disease occurs as an inflammatory process on the venous wall and is accompanied by the formation of a blood clot on it - a thrombus. In most cases, thrombophlebitis of the lower extremities is diagnosed.
The main signs and symptoms of thrombophlebitis are quite obvious: redness occurs in the area of the vein, a compaction is felt under the skin, and pain appears when pressed. If the inflammation spreads, the temperature may rise.
If a blood clot significantly disrupts the blood flow in a vein, the skin at the site of its appearance becomes blue. Also among the symptoms of a blood clot in the deep veins of the leg are heaviness in the legs and swelling.
Deep vein thrombosis
For the development of the disease, a combination of several factors is necessary:
- damage to the internal lining of the venous wall as a result of exposure to a mechanical, chemical, allergic or infectious agent;
- violation of the blood coagulation system;
- slowing down blood flow.
Under certain circumstances, blood viscosity increases. If there are obstacles to the normal flow of blood on the walls of the vein, the risk of blood clots increases. A small blood clot that forms on the venous wall causes inflammation and further damage to the vein wall, which causes the formation of other blood clots.
The occurrence of deep vein thrombosis is facilitated by congestion in the veins of the lower extremities. The cause of stagnation is immobility or inactivity of a person for a long time. Triggering factors for deep vein thrombosis:
- injury, surgery, excessive physical stress;
- infection;
- prolonged immobility in conditions after surgery, neurological and therapeutic diseases;
- period after childbirth;
- taking oral hormonal contraceptives;
- malignant tumors (especially cancer of the stomach, lungs and pancreas);
- DIC syndrome.
The risk of developing the disease increases with prolonged immobile position with legs down. Thus, in the West there are the terms “economy class syndrome” and “television thrombophlebitis”. In the first case, we are talking about people who developed deep vein thrombosis after a long flight. The second is about elderly patients who developed the disease after sitting in front of the TV for a long time. In both cases, the trigger factor was a long stay in a sitting position with bent legs, which creates obstacles to normal venous outflow.
The return of blood through the veins is largely ensured by muscle contraction. After operations and with some chronic diseases, the patient remains practically motionless for a long time. As a result, congestion develops in the lower extremities, leading to deep vein thrombosis.
When taking oral contraceptives, blood diseases, and malignant tumors, thrombosis is largely due to hypercoagulation (increased blood clotting). In some cases, impaired blood flow in the deep veins may indicate Buerger's disease (thromboangiitis obliterans of allergic origin).
As a rule, deep vein thrombosis develops in the lower extremities. However, deep vein thrombosis in the arm area is sometimes observed, which occurs when exposed to the following triggering factors:
- catheterization of veins of the upper extremities. A catheter located in a vein for a long time causes irritation of the venous wall and leads to the formation of a blood clot;
- implanted cardiac fibrillator or pacemaker;
- malignant neoplasm in the vein area;
- excessive load on the upper limbs in athletes (baseball players, swimmers, weightlifters). The disease develops due to compression of the deep veins of the upper extremities by trained muscles of the shoulder girdle.
Causes
- Thrombophlebitis can develop even due to minor trauma to the vessel , for example, after using a catheter.
- Some patients are prone to the formation of blood clots , increased blood clotting, which is hereditary or acquired.
- The disease causes an inflammatory process that develops locally or in the body as a whole.
- The cause is venous congestion , accompanied by a slowdown in blood flow due to varicose veins, prolonged bed rest, and paralysis of the limbs.
- Thrombophlebitis can occur due to the body or limb being stationary , for example, when traveling.
- Pregnancy, childbirth, gynecological operations, and abortions provoke the formation of blood clots .
Virchow's triad
Medicine identified the basic principles of thrombosis back in the nineteenth century. This was done by the famous German doctor Rudolf Virchow.
- The first principle is that for thrombosis to start, damage to the inner wall of the vessel (endothelium) is required.
- The second principle is that blood clots form in areas of blood vessels where blood flow is uneven (vortices) or where blood flow is slow.
- The last principle is that the rate of blood clot formation is influenced by blood viscosity. The higher it is, the faster the blood clots grow.
Development of thrombophlebitis of the lower and upper extremities
The disease most often develops in the lower extremities, since they bear twice the pressure and the heart has difficulty pumping blood upward. Therefore, thrombophlebitis of the legs is a very common phenomenon. Thrombophlebitis of the upper extremities develops less frequently, but is no less dangerous.
A thrombus on the wall of a vein occurs as follows. Due to an inflammatory or pathological process, the vessel narrows, its permeability decreases - blood stagnation and a clot occur, which grows due to platelets, fibrin and leukocytes. Eventually it either blocks the vein or breaks off when pressure in the bloodstream increases (for example, during exercise).
According to the main classification, the disease is usually divided into thrombophlebitis of deep veins (cause - disturbance of venous blood flow) and thrombophlebitis of superficial veins (cause - varicose veins).
Acute venous thrombosis of the subclavian veins
Acute venous thrombosis of the subclavian veins (Paget-Schrötter syndrome) Paget-Schrötter syndrome is acute thrombosis of the subclavian vein
The syndrome is named after James Paget, who first proposed venous thrombosis causing pain and swelling of the upper extremities, and Leopold von Schrötter, who later associated the clinical syndrome with thrombosis of the subclavian and axillary veins (synonym: force thrombosis).
The incidence of this disease is 13.6-18.6% of the total number of patients with acute thrombosis of the vena cava and their main tributaries. Paget-Schretter syndrome most often occurs at a young age, mainly between 20 and 30 years. This pathology is more common in men. Right-sided localization of the process is observed much more often (2-2.5 times). Thrombosis of the subclavian vein in Paget-Schroetter syndrome is caused by chronic trauma to the vein and its tributaries in the area of the costoclavicular space (Fig. 1). The disease often occurs due to physical exertion in the shoulder girdle. Symptoms of the disease can appear both during normal work and after sleep.
Figure 1. Anatomy of the costoclavicular space.
Symptoms of Paget-Schroetter syndrome
The main symptom is swelling of the affected upper limb and, to a lesser extent, of the upper chest on the affected side.
One of the features of the disease is an acute onset and rapid progression, without any visible causes or warning signs, literally before our eyes, the entire limb swells and becomes cyanotic. Less commonly, clinical manifestations of the disease continue for 2-3 days. A characteristic feature of edema in Paget-Schroetter syndrome is the absence of a fossa after finger pressure.
Most often, patients are bothered by pain of varying nature and intensity in the limb, in the shoulder girdle, which intensifies with physical activity, as well as weakness, a feeling of heaviness and tension.
Dilatation and tension of the saphenous veins in the early stages of the disease are usually observed in the area of the cubital fossa. Subsequently, with a decrease in swelling, dilated veins are most pronounced in the area of the shoulder and forearm, shoulder girdle, and anterosuperior chest.
In most cases, the color of the skin of the upper extremities is cyanotic, less often pink-cyanotic. When you raise your hand up, the cyanosis decreases, and when you lower it, it increases.
A very important sign of Paget-Schretter syndrome is the discrepancy between pronounced local changes and the general condition of the patients. The body temperature is usually normal, the general condition of the patients does not suffer.
Diagnostics
The sudden onset of edema, cyanosis and numbness of the upper limb associated with exercise are the fundamental symptoms of this disease.
Today, the priority in diagnostics are ultrasound research methods: Dopplerography, ultrasound duplex scanning (USDS), ultrasound triplex scanning (UTS). The accuracy of the methods exceeds 90%. Non-invasiveness and safety allow it to be used repeatedly without causing harm to the patient.
A phlebographic study provides detailed information about the localization and extent of thrombosis of the axillary and subclavian veins, the compensatory capabilities of colateral blood outflow, and the etiology of the pathological process.
Treatment
In the acute stage, in severe cases, hospitalization of patients is indicated. Mild cases of the disease are treated on an outpatient basis.
The hand is fixed on a scarf, compression sleeves are used, and the hand is given an elevated position.
Drug treatment includes the prescription of antithrombotic agents, anti-inflammatory and analgesic drugs.
Various topical agents and physiotherapeutic procedures (short-wave diathermy, UHF currents, electrophoresis) are used locally.
Forecast
The prognosis for Paget-Schretter syndrome is favorable for life, but complete recovery does not occur. Complications of the disease in the form of pulmonary embolism and venous gangrene are extremely rare. Most of them retain residual effects of venous insufficiency of the limb, and only some patients return to their previous physical work. Most patients need to be transferred to easier work, and some of them need to be declared disabled.
In order to receive diagnostic and therapeutic assistance, patients with various diseases of the vascular system, including thrombosis of veins of various locations, can contact the Medical Clinical Center "Health" for an appointment with cardiovascular surgeons.
The arsenal of diagnostic capabilities includes ultrasonic triplex scanning (UTS), spiral computed tomography, modern x-ray surgical research methods (SCT, venography, etc.).
If indications are identified, the patient may be hospitalized in the inpatient department of the Moscow Clinical and Clinical Center "Zdorovye", in the department of cardiovascular surgery.
Acute thrombophlebitis
This pathology can develop in the deep veins suddenly and against the background of an infectious disease, for example, mild flu, which was poorly treated. In such cases, deterioration can occur within a few hours: the leg quickly swells, the skin becomes tense, and the pain becomes unbearable.
Among the complications is the development of purulent thrombophlebitis, the main symptoms of which are numerous abscesses along the vein. In most cases, this type of disease can be successfully treated, but if the process is neglected, chronic venous insufficiency can persist for life.
Acute superficial thrombophlebitis affects veins located close to the surface of the skin . More often than others, the great saphenous and small saphenous veins in the legs are affected. The disease manifests itself in the form of small seals on the skin, pain during exercise, and an increase in temperature to 37.5-38 degrees.
This type of pathology is not so dangerous and is treated mainly with drugs that inhibit blood clotting - anticoagulants. Hirudotherapy is also used as prescribed by a doctor.
Chronic thrombophlebitis of the extremities
The most common cause of the development of this form is varicose veins of the saphenous veins, accompanied by an inflammatory process. Chronic thrombophlebitis of the superficial veins of the lower extremities has the following symptoms and signs: pain along the vein, swelling, redness at the site of the affected vessel, fever.
When the blood clot grows and the flow of blood from the limb is disrupted, the skin tone may change towards bluish. The structure of the skin itself changes, ulcers and abscesses form on the legs, accompanied by unbearable itching.
Chronic disease has a long lifespan: the formation of a blood clot can take several months or even more than a year. At the first symptoms, you should consult a doctor. At an early stage, treatment is especially effective: physiotherapeutic procedures are sufficient.
Treatment
In the early stages of the disease, thrombosis is treated with medications.
When a blood clot has formed, for example, after using a catheter on the arm, effective treatment is possible by administering drugs that dissolve the blood clot (streptokinase, urokinase, etc.).
To relieve pain, non-steroidal painkillers (diclofenac, ibuprofen and others) are used.
If the patient has increased blood viscosity, which is prone to thrombosis, anticoagulants are used. As a rule, heparin is prescribed first, and then drugs with a milder effect (warfarin).
Specific therapy is complemented by antibacterial treatment (sulfonamide and tetracycline groups of antibiotics).
In the later stages, there is nothing more effective than surgery to remove the blood clot (thrombectomy).
The classic version of thrombectomy consists of making an incision over the blood clot, injecting saline solution to soften the blood clot, after which it is removed with a special clamp.
In endovascular surgery, an incision is made along the edge of the blood clot, a catheter is inserted, filled with saline, and pulled back out along with the blood clot.
Postpartum thrombophlebitis
Signs and symptoms of this disease can even occur in young women who had no health problems before pregnancy. In addition to the superficial and deep veins of the extremities, the veins of the uterus and pelvic veins can be affected.
The cause is stagnation of blood in the pelvic organs during pregnancy. Blood clotting increases, which means the risk of blood clots. There is a high risk of developing the disease in pregnant women suffering from anemia, obesity, and late toxicosis. The formation of a blood clot can provoke difficult childbirth and cardiovascular diseases.
Postpartum deep vein thrombophlebitis is usually acute: severe pain, swelling, chills occur in the leg, and the pulse increases sharply due to increased pressure in the circulatory system. When the veins of the uterus are damaged, heavy bleeding is observed for a long time. In this case, you should immediately consult a doctor, and treatment will take several weeks.
Superficial thrombophlebitis of the upper and lower extremities can last up to 30 days, and in the absence of proper treatment, become chronic. That is why you cannot delay visiting a doctor.
Causes and risk factors for varicose veins of the hands
There are several risk factors that cause the development of bulging nodes on the arms: Age-related loss of elasticity and thinning of the skin is the main and most common reason why arm veins become more and more visible. These are age-related changes that are not a disease, but cause aesthetic troubles.
- Active physical activity in the heat
During exercise, blood pressure in the arteries increases, which causes the muscles to swell and put pressure on the saphenous and internal veins. This causes them to swell and protrude above the skin. Over time, the walls of the blood vessels stretch and they remain visible even without physical activity. Hot weather leads to heating of the skin and an increase in blood circulation in peripheral vessels. A larger volume of blood leads to relative overflow of the subcutaneous vessels and their bulging.
- Vascular diseases
Often, bulging veins in the arms are caused by vascular diseases. Arteriovenous malformations and subclavian vein thrombosis are common. Despite the fact that varicose veins in the arms are rarely a serious medical problem, eliminating this cosmetic defect requires the attention of a phlebologist. The presence of pathological causes for varicose veins of the hands makes it necessary to conduct a full diagnosis.
At-risk groups
Certain groups of people are at greatest risk of developing symptoms and signs of this disease, including:
- bedridden patients who are forced to spend a long time with immobile limbs (for example, with fractures, after operations);
- making long trips in cars, airplanes;
- stroke survivors and those suffering from paralysis;
- pregnant or recently given birth women;
- undergoing treatment with a catheter;
- having a genetic predisposition to the formation of blood clots;
- those over 55 years of age.
Prevention
Preventive actions:
- Using elastic bandages and compression garments
- To give up smoking
- Rational and proper nutrition
- Vitamin therapy
- Physical activity
- Timely treatment of concomitant diseases
- Monitor cholesterol and blood glucose levels
- Reducing body weight.
If symptoms of the disease appear, you can seek advice and examination in Moscow from specialists from the Central Clinical Hospital of the Russian Academy of Sciences. Registration is made by phone...
Diagnostics
Modern methods for diagnosing thrombophlebitis of the lower and upper extremities include:
- ultrasound examinations in the form of Dopplerography, duplex scanning;
- MRI and CT in vascular mode;
- X-ray examinations using a contrast agent;
- blood tests: clinical blood test, coagulogram, D-dimer.
For superficial thrombophlebitis of the upper and lower extremities, special tests are performed to determine the extent of its prevalence. Also during the examination it will be necessary to identify the causes of blood clot formation, pathological process, and inflammation. This means the diagnostic program can be adjusted by a doctor.
Diagnosis of pathology
Which doctor should I contact?
Emergency surgery is often required, and it can only be performed in a hospital setting.
Due to the possibility of severe complications, it is necessary to call an ambulance without wasting time.
You can also contact the vascular surgery department yourself. If it is absent, go to the general surgery department.
In mild cases, treatment can be prescribed on an outpatient basis by a phlebologist or vascular surgeon.
Examination methods
Differential diagnosis allows you to identify a blood clot in the arm. This is usually not a problem. A dense cord of the affected vessel and a thrombus in it can be determined by palpation.
Laboratory tests - CBC, blood biochemistry and coagulogram - help determine the tactics of further treatment.
Without the results of these tests, surgical treatment is impossible.
Instrumental studies:
- Reasons why your arm hurts from shoulder to elbow. How to treat muscle pain? Character of pain on the right and left sides
- contrast phlebography. After the contrast enters the blood, both a standard X-ray examination and a CT or MRI examination can be performed. It can be carried out to clarify the scope of the upcoming surgical intervention;
- Duplex scanning – helps determine the composition and size of a blood clot, the condition of the walls of blood vessels, and the degree of blood flow disturbance.
What is the danger of thrombophlebitis of the upper and lower extremities?
The first signs and symptoms of this disease should alert you. You should not trust traditional methods of treatment or hope that the disease will go away on its own. Its complications are extremely serious, and some are even incompatible with life. That is why it is extremely important to undergo a timely examination and begin treatment as early as possible. Thrombophlebitis is curable, and you can get rid of the unpleasant consequences. Qualified treatment will significantly improve your quality of life and relieve unbearable pain in your limbs.