Causes of high blood pressure
High blood pressure is divided into 2 types:
- primary (essential) hypertension (or hypertension) is the most common type of high blood pressure, often has no cause, develops over many years, the risk increases with age;
- secondary hypertension occurs against the background of the development of any disease (kidneys, endocrine system organs, sleep apnea) or taking certain medications.
Causes of high blood pressure include:
- old age (the older a person is, the higher the likelihood of developing hypertension);
- family history of the disease (high blood pressure in parents or other close relatives);
- unhealthy diet - diet high in salt and fat;
- lack of physical activity;
- overweight, obesity;
- sleep disorders;
- chronic diseases (chronic kidney disease, endocrine disorders, diabetes, high cholesterol);
- race (eg, African Americans have a higher risk);
- gender (in middle age, high blood pressure develops more often in men, in old age - in women; women who had high blood pressure during pregnancy are more prone to arterial hypertension in old age);
- certain medications (contraceptives, decongestants, NSAIDs, antidepressants);
- stress;
- smoking;
- alcohol abuse;
- non-compliance with sleep schedule, night shift work.
High blood pressure is often called the “silent killer” due to its lack of noticeable symptoms. In some cases (especially when blood pressure levels reach dangerously high levels), a person may complain of headache, nosebleeds, and shortness of breath. Many people do not associate these symptoms with abnormal blood pressure readings because they are not in the habit of periodically monitoring their blood pressure with a doctor or at home.
Treatment of the disorder
At the first stage of hypertension, normal blood pressure can be returned with the help of modern medications that reduce low blood pressure, for example, diuretics. Alternative techniques are also used - acupuncture, massage of biologically active points, therapeutic baths, electrophoresis and other techniques.
The treatment regimen for arterial hypertension also includes a diet that limits the consumption of salt, fatty and high-calorie foods. Animal fats are replaced with vegetable fats, baked goods and sweets with dried fruits, sugar with honey, fatty pork with lean poultry and fish.
Medicinal plants such as rosehip, an infusion of which can successfully replace your usual morning coffee, will help correct blood pressure.
What cannot be done at the early stage of diastolic hypertension? The list of absolute contraindications includes:
- smoking;
- alcohol abuse;
- lack of physical activity;
- stress;
- lack of sleep;
- binge eating;
- excessive physical and nervous overload.
Important! Even if there are no symptoms and you feel well with a blood pressure of 133 over 88 or 137 over 90, you should not refuse regular blood pressure monitoring at home and visits to your doctor. Monitoring the potential development of hypertension allows timely recognition of deviations from the norm and taking measures to correct the condition.
Blood pressure readings
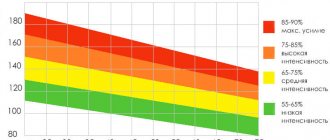
- Normal pressure is from 90/60 mm Hg. Art. up to <120/80 mmHg Art.
- Prehypertension (risk factor for the development of arterial hypertension) - 120–129 mm Hg. Art. / <80 mmHg Art.
- Arterial hypertension 1st degree - 130–139 mm Hg. Art. or 80–89 mm Hg. Art.
- Arterial hypertension 2 degrees - ≥140 mm Hg. Art. or ≥90 mm Hg. Art.*
*American Heart Association classification.
Online blood pressure calculator on the NHS website.
American College of Cardiology online cardiovascular risk (stroke, heart attack and other diseases) calculator (risk of complications for patients with high blood pressure over the next 10 years and beyond).
Consequences of secondary hypertension
Even if a blood pressure of 135 over 90 or 138 over 90 does not affect your well-being, it can gradually worsen the blood supply to tissues and cells. As a result, a cerebral stroke, sclerotic changes in the kidneys, hypertrophy of the left cardiac ventricle, and microinfarction may develop. And even though, according to statistics, this probability is only 15%, it is not worth risking your own health.
The pressure should be reduced if the increase in values causes a deterioration in health and does not return to normal within a few days. The use of potent drugs prescribed to chronic hypertensive patients is not recommended.
How often should you check your blood pressure readings?
Blood pressure is usually measured when visiting a doctor (for example, a therapist). There is no need to specifically visit a specialist for this; it is enough to ensure that the pressure is measured at least once every 2 to 5 years, starting from the age of 18 (with normal blood pressure and no increased risk of cardiovascular diseases).
People over 40 years of age, and people 18–40 years of age at risk of high blood pressure, should have their blood pressure checked at a healthcare facility at least once a year. If a diagnosis of arterial hypertension has been established or a person has other risk factors for developing cardiovascular diseases, it is recommended to measure blood pressure more often and not neglect monitoring at home. Your doctor will help you choose a device for measuring blood pressure (tonometer).
For children 3 years of age and older, blood pressure is measured regularly during annual routine examinations.
Caution: The American Heart Association does not recommend the use of wrist- or finger-worn blood pressure monitors, which are less accurate.
If recommended, measure blood pressure at home twice a day on the left and right arm: in the morning before breakfast (but not immediately after waking up) and before taking any medications, and in the evening, preferably at the same time. In each case, you need to measure the pressure 2-3 times (at short intervals, 1-3 minutes) for a confident, accurate result. 30 minutes before, do not smoke, do not eat, do not drink coffee (and alcohol), do not exercise, and empty your bladder. During the measurement, you must sit in a comfortable position, leaning back in a chair or armchair, do not cross your legs and ankles, and do not talk. The arm on which the cuff is worn must be freed from clothing and held at heart level; it is most convenient to place it on a table or armrest of a chair. Don't forget to write down your measurement results.
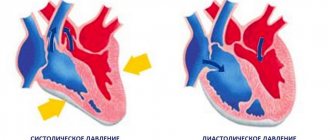
Upper, lower, pulse pressure
The upper, systolic, cardiac pressure indicates the work of the heart at the moment of pushing out blood. An increase in the upper indicator is accompanied by a rapid pulse, discomfort in the chest area, and shortness of breath. High systolic pressure accelerates wear and tear of the heart and leads to structural changes in the myocardium. Long-term hypertension may develop:
- Coronary heart disease is a decrease in blood circulation in myocardial tissues.
- Heart failure is incomplete filling and emptying of the ventricles.
- Infarction is the formation of a necrotic focus in the myocardium.
- Left ventricular myocardial hypertrophy is the growth and thickening of muscle tissue, which leads to impaired contractile function, up to sudden cardiac arrest.
Lower, diastolic, renal pressure depends on the condition of the blood vessels. Manifestations of high diastolic pressure are muscle weakness, visual disturbances, and dizziness. Also, the need to control blood pressure is indicated by kidney disease, swelling, difficult diuresis during the day and excessive urination at night.
Consequences of hypertension with high renal pressure:
- Stroke is an acute disorder of cerebral circulation, which may be accompanied by hemorrhage.
- Renal failure - due to tissue nutritional disturbances, the kidneys cannot work normally, intoxication begins with damage to all organs and systems.
- Deterioration in the elasticity of blood vessels - fragility, microhemorrhages, and hematomas appear on the skin.
- Malnutrition of the limbs - peripheral blood circulation is hampered with the possible formation of ulcers and the development of gangrene.
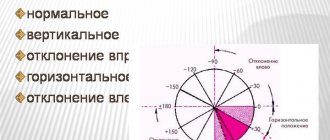
Also important is the difference between the upper and lower indicators - pulse pressure. Normally it is 30-50 mmHg. When it decreases, lethargy occurs, throbbing headaches in the frontal and occipital regions, cognitive function is impaired, and the ability to concentrate decreases. A decrease in the indicator may occur due to:
- Atherosclerosis, aortic aneurysm.
- Kidney nutritional disorders.
- Aneurysms with different localizations, including cerebral vessels.
- Inflammation of the serous membrane of the heart.
- Hemorrhages.
With increased pulse pressure, the myocardium regulates blood circulation with great tension, which provokes disturbances in the functioning of the heart, characteristic of high systolic pressure.
Is it possible to normalize high blood pressure and what to do?
Yes, with the help of lifestyle modification (influencing modifiable factors), treating the underlying disease, taking medications that normalize blood pressure.
Lifestyle modifications include proper nutrition, including avoiding fatty foods and reducing salt intake (the DASH (Dietary Approaches to Stop Hypertension) eating plan recommended by the US National Heart, Lung, and Blood Institute is preferred); weight normalization; quitting smoking and alcohol; regular physical activity; stress management (for example, mastering relaxation techniques).
If you have persistently high blood pressure due to a medical condition (such as diabetes) or caused by taking certain medications, it is recommended that you consult your doctor. Control of the underlying disease, refusal of drugs (or their replacement) that increase blood pressure, make it possible to stabilize the patient’s blood pressure and condition.
Nonmodifiable risk factors associated with high blood pressure include age and family history.
Features of headaches in hypertension
Pressure headaches are the result of impaired vascular ability to adapt to external and internal changes. Blood presses on the inner walls of blood vessels, irritating the receptors. These signals travel to the brain, where they are converted and cause pain. In advanced stages of the disease, this condition is accompanied by increased fluid pressure inside the skull, which also causes severe headaches.
Chronic hypertension manifests itself as alternating periods of rest and increased blood pressure. During attacks, the patient has a very headache, the pressure in the arteries rises sharply. This can be caused by a number of factors:
- physical or mental fatigue - in this case, to normalize blood pressure indicators, it is enough to pay attention to proper rest;
- changes in weather conditions - a sharp increase in atmospheric pressure often provokes attacks of hypertension, which can be eliminated with rest and medications;
- abnormal physical activity – causes acceleration of blood flow and heart rate, which is dangerous if the elasticity of the blood vessels is insufficient;
- pregnancy – hormonal changes cause attacks of hypertension;
- unhealthy diet – consuming excess amounts of salt and spices leads to impaired removal of fluid from the body, swelling and an increase in the volume of circulating blood.
Headache with high blood pressure has its own characteristics. It can be caused by various reasons, so it is usually classified into vascular, liquor, ischemic and neuralgic. In most patients, it spreads to the temples and back of the head. It is sharp, pressing, and leads to impaired concentration. With a sharp increase in pressure, hearing and vision deterioration and fainting may occur.
Vascular pain
The main cause of vascular syndrome is a violation of the outflow of fluid from the brain. Arteries and veins fill with blood, tissue swelling is observed. This leads to irritation of nerve receptors and an increase in pain. The pain in the head with pressure is pressing, the pulsation of blood vessels is felt. It intensifies if you lower your head down, as well as with sudden movements, coughing and sneezing.
Liquor syndrome
Another reason why headaches occur with pressure is a violation of the movement of cerebrospinal fluid. This is a special fluid that is found in the brain and spinal cord. It performs a shock-absorbing function, protects soft tissues from compression and regulates pressure in the skull. Normally, it circulates constantly, but in case of vascular pathologies, heart disease and chronic hypertension, it is retained in the brain. This process is accompanied by aching, bursting pain, which intensifies during sudden movements of the head. The process is dangerous because the cerebrospinal fluid also contains nutrients for nerve cells. If fluid circulation is not stimulated, this can lead to cerebral ischemia and trigger a stroke.
Ischemic pain syndrome
The cause of headaches and pressure can be spasm of blood vessels. This leads to insufficient oxygen and nutrients reaching certain areas of the brain. The patient also experiences hearing and vision impairment, dizziness, a sharp increase in blood pressure and weakness. Attacks are relieved by using antispasmodics; rest and means to normalize the functioning of the nervous system are also useful.
Neuralgic pain
Increased pressure inside the skull affects all nerve structures. Excess cerebrospinal fluid leads to compression of the trigeminal nerve, which is responsible for the innervation of the skin and muscles of the face. The pain in this case is sharp, throbbing, concentrated in the facial part. It worsens during movement, bending and turning the head.
Additional symptoms
It is important for a patient with chronic hypertension to know how a headache occurs with high blood pressure. It has several features that indicate a simultaneous increase in blood pressure:
- headache spreads to the back of the head and temporal parts of the head;
- the nature of the pain is pressing, there is a feeling of expansion of the contents of the skull;
- filling of blood vessels leads to redness of the skin and mucous membranes, minor hemorrhages are possible due to damage to the walls of the capillaries;
- ringing or noise in the ears is a typical sign of high blood pressure;
- blurred vision, the appearance of various hallucinations in the form of black dots or circles before the eyes;
- weakness, fatigue, decreased performance;
- dizziness, nausea;
- a sharp increase in blood pressure is the cause of fainting.
If your head starts to hurt severely, you need to measure your blood pressure. The procedure can be carried out independently, using a tonometer. This device should be in every home medicine cabinet, even if there are no patients with chronic hypertension in the family. Headaches go away after blood flow is restored and pressure is normalized, including with individually selected medications.
Treatment of high blood pressure
Treatment of arterial hypertension is based on lifestyle modification, constant monitoring of blood pressure, and the use of antihypertensive drugs (medicines that lower blood pressure) - one or more, based on the patient's individual situation.
Medicines prescribed for high blood pressure include: ACE inhibitors, angiotensin II receptor inhibitors, calcium channel blockers, diuretics, beta blockers, alpha blockers, alpha beta blockers. In most cases, these medications do not cause side effects. However, you should not self-medicate; you should consult a doctor who will select an effective drug and prescribe a regimen for its administration. It is important to follow all recommendations, observe the dosage and not skip taking the drug(s).
When diagnosing arterial hypertension, 24-hour blood pressure monitoring (ABPM) provides an accurate idea of the patient’s blood pressure levels. ABPM also excludes the factor of chance, distortion of real blood pressure readings (the so-called “white coat” syndrome or “white coat” hypertension), and registers imperceptible changes in blood pressure (for example, during sleep). This test is recommended by the American Heart Association to confirm the diagnosis of hypertension.
Diagnostic methods
You can diagnose hypertension at home, if you have a working tonometer. However, the disease may have its own characteristics and occurs for various reasons. It is important to undergo a full examination to determine why your blood pressure is rising. This information will help you choose an effective treatment regimen, as well as prevent further development of the disease. After examining and measuring blood pressure, the doctor may prescribe the following diagnostic methods:
- MRI of the head is one of the most effective methods, which is used when there is a suspicion of increased intracranial pressure, the presence of neoplasms and foci of ischemia;
- Dopplerography of the vessels of the neck and head is an informative technique that involves studying blood flow using a contrast agent;
- clinical and biochemical blood tests - allow you to evaluate the chemical composition of the fluid and determine protein metabolism disorders;
- X-ray of the cervical spine - spondylosis, osteochondrosis and other diseases that lead to compression of blood vessels and increased blood pressure in them will be visible in the pictures.
The Clinical Brain Institute has all the conditions to undergo a complete examination for headaches and high blood pressure. To confirm the diagnosis, the patient will be offered consultations with specialists of a narrow and broad profile. This will allow you to comprehensively consider the disease and select treatment that will affect not only the symptoms, but also the cause of the disease.
Blood pressure 130 over 90 during pregnancy
Blood pressure can increase noticeably during pregnancy. Therefore, indicators of 130 over 90, 132 over 86 are the norm, but it is worth knowing that the maximum acceptable blood pressure value during pregnancy is 140 (upper) over 90 (lower, cardiac).
Before the examination, a woman needs to be more attentive to her own feelings and write down the results of the tonometer in the morning.
If all measurements are in perfect order, and no discomfort or other problems are observed with an increase, this is the body’s reaction to changes in the amount of hormones .
However, if high blood pressure is observed frequently and symptoms of hypertension are present, then consultation with your doctor is necessary .
Symptoms of hypertension
When prescribing medications, the doctor needs to know :
- Number of weeks of pregnancy.
- age .
- Any impact on the baby.
It is best to use healthy herbs and drink other folk remedies.
First aid measures
If a sudden feeling of dizziness is caused by high blood pressure, the patient's condition can quickly worsen. When the tonometer readings reach 180/140, hemorrhagic convulsions may begin, many patients lose consciousness, at such moments the risk of developing cerebral hemorrhage and rupture of the heart muscle increases significantly.
Therefore, the patient urgently needs first aid:
- put the person in a horizontal position, if he is conscious, raise his legs above head level;
- unbutton your clothes, loosen your belt, free your neck and wrists;
- ensure the flow of oxygen by opening the windows in the room;
- give the patient an antihypertensive tablet if you have a tonometer at hand and it is possible to accurately determine that your health has worsened due to increased blood pressure;
- after reducing pressure and eliminating dizziness, pain in the temples, nausea and vomiting, monitor the patient, measuring blood pressure every half hour.
If a person loses consciousness during an attack of dizziness and a surge in blood pressure, you should not put him on the bed, you need to put him on a chair. Also, ensuring there is an influx of fresh air into the room, wash your face with cold water and call an ambulance.