Scientific editor: Andriyanov G.Yu., therapist, statistician. December, 2021.
Synonyms: Henoch-Schönlein disease, hemorrhagic vasculitis, anaphylactoid purpura, allergic purpura, Henoch hemorrhagic purpura, capillary toxicosis.
ICD-10 code: D.69.0. Allergic purpura.
Hemorrhagic vasculitis is a disease primarily affecting the capillaries of the skin, joints, gastrointestinal tract and kidneys. Characterized by a symmetrical rash, joint inflammation, and often abdominal pain. Possible kidney damage.
Hemorrhagic vasculitis can begin at any age. However, children under 3 years of age rarely get sick. Up to 90% of cases of hemorrhagic vasculitis occur between the ages of 4-12 years.
The prevalence of hemorrhagic vasculitis according to 2015 data in Russia is 23-25 people per 10,000. Boys aged 7-12 years are most often affected by the disease.
The onset of the disease is possible 1-4 weeks after the following factors:
- infectious diseases, such as tonsillitis, ARVI, chickenpox, scarlet fever, measles.
- vaccination (typhoid fever, measles, yellow fever - amaryllosis, cholera),
- drug intolerance (ampicillin, erythromycin, penicillin, quinidine, quinine, losartan, cytarabine),
- food allergy,
- hypothermia.
Hemorrhagic vasculitis is based on increased production of immune complexes, activation of the complement system, increased vascular permeability, and damage to the capillary wall.
General information
Hemorrhagic vasculitis in adults and children (synonyms - Henoch-Schönlein disease, allergic purpura, capillary toxicosis, Henoch hemorrhagic purpura) refers to systemic diseases affecting predominantly the microvasculature of the skin, gastrointestinal tract, joints, and kidneys.
The most affected part of the vascular bed includes small-caliber vessels - post-capillary venules, capillaries and arterioles with the deposition of immune complexes. The ICD-10 code for hemorrhagic vasculitis is D69.0. In 2012, the nomenclature of vasculitis was revised and Henoch-Schönlein purpura received the name IgA vasculitis, that is, vasculitis with deposition of IgA-dominant immune complexes in the vessel wall, affecting small vessels. The disease occurs in all age groups in adults, but the peak incidence occurs in children (3-8 and 7-11 years), averaging 13-18 cases/100 thousand population. Children under 3 years of age rarely get sick, which is obviously due to low immunological reactivity and the sensitization of their body has not yet taken place. The higher incidence of school-age children is due to an increase in the level of sensitization in this age period and the intensity of allergic reactions. As you get older, the incidence decreases, and after 60 years it is extremely rare. The male gender predominates in the morbidity structure (2:1). In the winter and spring periods, the incidence is higher, which is explained by a decrease in the body's reactivity during this period, an increased incidence of ARVI and intensive contacts in children's organized groups.
The specificity of the disease is the variety of clinical manifestations (skin rashes, abdominal pain, articular syndrome, kidney damage, etc.), which often at the onset of the disease leads to a visit to doctors of various specializations (local pediatrician, dermatologist, nephrologist, surgeon, neurologist), untimely diagnosis and delay of adequate treatment, thereby contributing to the development of complications and worsening prognosis.
Chapter 25. Systemic vasculitis
Systemic vasculitis
Systemic vasculitis (SV) is a heterogeneous group of diseases, the main morphological feature of which is inflammation of the vascular wall, and the range of their clinical manifestations depends on the type, size, location of the affected vessels and the severity of accompanying inflammatory changes. Systemic vasculitis is a relatively rare human pathology. There are no epidemiological studies on the incidence of juvenile forms of SV. In the scientific and scientific-practical literature, SV is considered in the group of rheumatic diseases. The working classifications of systemic vasculitis proposed by experts are based on morphological characteristics: the caliber of affected vessels, the necrotizing or granulomatous nature of inflammation, the presence of giant multinucleated cells in granulomas. In ICD-10, systemic vasculitis was included in the heading XII “Systemic lesions of connective tissue” (M30-M36) with subsections “Polyarteritis nodosa and related conditions” (MZO) and “Other necrotizing vasculopathies” (M31).
Classification of systemic vasculitis ICD-10
• MZO Polyarteritis nodosa and related conditions.
M30.0 Polyarteritis nodosa.
M30.1 Polyarteritis with pulmonary damage (Churgia-Strauss), allergic and granulomatous angiitis.
M30.2 Juvenile polyarteritis.
MZO.Z Mucocutaneous lymphonodular syndrome (Kawasaki).
M30.8 Other conditions associated with polyarteritis nodosa.
• M31 Other necrotizing vasculopathies.
M31.0 Hypersensitivity angiitis, Goodpasture's syndrome.
M31.1 Thrombotic microangiopathy, thrombotic and thrombocytopenic purpura.
M31.2 Fatal median granuloma.
M31.3 Wegener's ceanoulomatosis, necrotizing respiratory granulomatosis.
M31.4 Aortic arch syndrome (Takayasu).
Pathogenesis
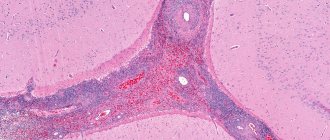
The mechanism of development of hemorrhagic vasculitis (HV) is based on a generalized immunocomplex necrotizing lesion of the blood vessels of the microvasculature of the skin and internal organs with the formation/deposition of granular IgA deposits (antigen-antibody complexes) in the vascular wall and activation of the complement system. As a consequence, a protein membrane attack complex is formed, which underlies the osmotic lysis of endothelial cells.
Also, when the complement system is activated, chemotactic factors are actively released. affecting polymorphonuclear leukocytes, which in turn secrete lysosomal enzymes that aggravate damage to the vascular wall. As a result of damage to the structure of the vascular endothelium, collagen fibers are exposed, which promotes the adhesion of platelets to the surface of the endothelium and the initiation of the blood clotting mechanism. Subsequently, fibrin deposits form in the vessels, blood rheology worsens, aggregation of erythrocytes and platelets , and intravascular disseminated blood coagulation develops.
Against the background of increased vascular permeability and the development of thrombosis with subsequent depletion of the anticoagulant (antithrombin-III) link and thrombocytopenia of consumption, ruptures of blood vessels of the microvasculature of the skin and internal organs occur, which lead to the development of clinical symptoms of hemorrhagic syndrome. The pathogenesis of hemorrhagic vasculitis is schematically presented in the figure below.
Pathogenesis of hemorrhagic vasculitis
How it manifests itself
Symptoms of systemic vasculitis will depend on its type and severity, so manifestations can be very different.
For example, Takayasu arteritis, which usually occurs in women, affects only the large arteries of the body. The main symptoms here will be headaches, a feeling of coldness or numbness in the lower extremities, lack of pulse, vision problems, and increased blood pressure.
Behçet's disease is diagnosed more often in young men. The main symptom is ulcers that appear on the genitals, in the mouth, vision problems, and inflammatory skin diseases.
Buerger's disease is characterized by the appearance of small blood clots in the vessels of the legs. The main manifestations are pain and the appearance of ulcers.
Read also: Renal vasculitis
Giant cell arteritis develops in people over 50 years of age and affects the vessels of the head. Severe headaches and muscle pains, numbness of the tongue, and pain when chewing food appear. The ocular vessels are gradually damaged.
Wegener's granulomatosis affects the capillaries of the nose; the microscopic version affects the capillaries not only of the skin, but also of internal organs, especially the kidneys. When joints become inflamed and purple spots appear on the skin, we should talk about the cryoglobulinemic variant.
Churg-Strauss syndrome is characteristic only of the veins and arteries of the lungs, and the nodular version can develop anywhere in the human body.
Systemic vasculitis practically does not occur in children, and in adults the symptoms can be so different that it is not always possible to make an accurate diagnosis without special examination methods.
Classification
There is no single generally accepted classification of HS. The most commonly used clinical classification of the disease is based on one or another clinical syndrome. Accordingly, cutaneous, articular, renal, abdominal and mixed forms are distinguished.
According to severity they are distinguished:
- mild: few rashes; general condition is satisfactory; arthralgia ;
- moderate: profuse rashes, general condition of moderate severity, arthritis , arthralgia , microhematuria , periodic abdominal pain, slight proteinuria ;
- severe: profuse confluent rashes, severe general condition, angioedema , gross hematuria , persistent abdominal pain, nephrotic syndrome , gastrointestinal bleeding , acute renal failure .
According to the nature of the course: acute form (1-2 months), protracted (up to 6 months), chronic with frequent relapses.
Causes of hemorrhagic vasculitis
The causes of hemorrhagic vasculitis in adults have not yet been fully elucidated, however, in most cases, hemorrhagic vasculitis is of an infectious-allergic nature. Among the leading factors contributing to the development of the disease are:
- Infectious factor. Statistics show that in 60-80% of cases, hepatitis B is preceded by an upper respiratory tract infection. At the same time, the range of infectious agents is quite wide: Yersinia , streptococci , mycoplasmas , legionella , hepatitis viruses, respiratory syncytial virus , adenoviruses , Epstein-Barr , cytomegalovirus and others.
- The presence of foci of chronic infection ( tonsillitis , caries , adenoiditis , sinusitis , etc.).
- Taking medications (sulfonamide drugs, penicillin , ampicillin , erythromycin , antiarrhythmic and other drugs).
- Ingestion of potentially allergenic foods (chocolate, eggs, citrus fruits, dairy products, fish, strawberries, wild strawberries, etc.).
- Vaccination/serum administration.
- Insect bites.
- Excessive insolation/hypothermia.
There is also evidence of a genetic predisposition to hepatitis B, which is caused by deficiency of complement C7, as well as the presence of antigens A1, A2, A10, C3HLA Bw35, B8. Thus, in conditions of sensitization of the body, any etiologically significant factor listed above can be decisive in the development of hemorrhagic vasculitis. However, in a significant number of cases, the causes of capillary toxicosis cannot be determined.
Vasculitis (manifestations, ICD 10 classification, disease and forms of vasculitis)
Vasculitis ICD 10 (vasculitis - lat. Vasculium - small vessel; synonym: angiitis)
- inflammation of the walls of blood vessels of various etiologies. Vasculitis is a group disease and cannot be used as a nosological diagnosis without appropriate clinical, morphological and/or etiological characteristics. Depending on the type and degree of vascular damage, the following types and forms of vasculitis are distinguished:
Often, several types of vessels of different calibers are simultaneously or sequentially involved in the pathological process (in this case they speak of a generalized or systemic form of vasculitis). According to the predominant localization of inflammatory changes in the inner, middle or outer (adventitia) layer of the vascular wall, endo-, meso- and perivasculitis are distinguished (if only the arteries are affected - endo-, meso- and periarteritis, respectively); lesions of all layers of the vascular wall are designated by the term “panvasculitis” (with isolated damage to the arteries - panarteritis). By origin, vasculitis disease can be:
- a) primary, in which systemic vascular damage is the primary independent disease;
- b) secondary manifestations of vasculitis, which arise on the basis of any infectious, infectious-allergic, metabolic-endocrine or tumor disease and is one of the components (sometimes very important) of this disease.
Read also: Brain vasculitis
Secondary forms of vasculitis etiologically related to the underlying disease
, on the basis of which they arise. Usually these are either infectious diseases (typhoid fever, scarlet fever, sepsis in acute or subacute form, including protracted septic endocarditis), or systemic connective tissue diseases (rheumatism, rheumatoid arthritis, systemic scleroderma, dermatomyositis), or toxic-allergic diseases and conditions (hereditary intolerance), or metabolic-endocrine diseases (diabetic microangiopathy). The following are discussed as possible causative factors for primary vasculitis:
- a) acute and chronic infections;
- b) the influence of chemical and biological agents, incl. LP;
- c) the influence of physical factors - cooling, burns, insolation, ionizing radiation, physical trauma as a manifestation of vasculitis
- d) vegetative-neurotrophic disorders and endocrine disorders;
- e) genetic factors of forms of vasculitis (for example, arteritis of small branches of the pulmonary artery in congenital primary pulmonary hypertension).
The allergic theory of the pathogenesis of systemic vasculitis has a solid experimental basis. Clinical observations also confirm the allergic genesis of some forms of systemic diseases (for example, vasculitis as a disease that occurs due to intolerance to drugs, the use of vaccines, serums). Autoimmune disorders are of great importance in the mechanism of development of systemic vasculitis and its manifestations; at the same time, they are based on the possibility established by some authors of the formation of autoantibodies to the cellular and tissue substances of the vascular wall. Among other theories of the pathogenesis of systemic forms of vasculitis, the neurogenic and endocrine ones deserve attention, which are based not so much on experimental data, but on the clinically identified connection between neurovegetative and endocrine disorders and the development of certain diseases. A classic example of neurovegetative and neurotrophic vascular disorders is Raynaud's syndrome, which is often one of the first manifestations of primary or secondary (in collagenosis) diseases. In classifications, the main forms of systemic forms of vasculitis are periarteritis nodosa, thromboangiitis obliterans, hemorrhagic, brachiocephalic arteritis obliterans; forms of temporal arteritis, thrombotic, and thrombocytopenic purpura are less common. A special place among systemic vasculitic manifestations is occupied by generalized damage to small arteries such as necrotizing arteritis, which is combined with necrotizing-granulomatous damage to the upper respiratory tract, lungs, bones of the facial part of the skull, retrobulbar tissues of the eyes, described by Wegener and named after him - Wegener's granulomatosis. Among the secondary causes of vasculitis, generalized vascular lesions in typhus, scarlet fever, prolonged septic endocarditis, rheumatism, rheumatoid arthritis, systemic lupus erythematosus, systemic scleroderma, as well as changes in small vessels in diabetes mellitus - diabetic microangiopathy, are of greatest practical importance.
Treatment of patients with systemic vasculitis
must be carried out individually, taking into account the form of the disease and its stage. General principles of therapy for many manifestations of vasculitis: when an etiological factor is established (for example, drug intolerance), its immediate elimination; the use of anti-inflammatory, desensitizing and immunosuppressive drugs.
Read also: Complication of hemorrhagic vasculitis
Symptoms of hemorrhagic vasculitis
Clinical symptoms of Henoch-Schönlein disease are represented by four typical clinical syndromes: skin, articular, abdominal and renal. The number of organ manifestations of the disease most often varies from 1 to 2 of all classical clinical syndromes, which can develop in various combinations and in any sequence throughout the entire period of the disease. In rare cases, damage to other organs may occur: lungs, central nervous system, heart.
The onset of breastfeeding is often preceded by a prodromal period lasting from 4 to 12 days. In most cases, within 1-4 weeks the patient suffers from a disease, more often a sore throat , acute respiratory viral infection, exacerbation of a chronic disease, or has a history of allergic exposure (taking medications, vaccinations, exacerbation of an allergic disease). Clinical symptoms of this period are not specific and often manifest as general malaise, fever, headache, and loss of appetite.
The onset of hepatitis can develop gradually, when the first symptoms of purpura appear gradually against the background of the patient’s well-being and complete health and the general condition of the patients does not significantly affect. This type of onset of the disease is typical for isolated skin lesions. However, in some cases the disease begins acutely.
Hemorrhagic purpura can begin with any syndrome, but more often the onset of the disease is manifested by cutaneous hemorrhagic syndrome, which is gradually joined by lesions of other systems and organs.
Skin syndrome (form). Skin lesions are observed in all patients with hepatitis B and are a mandatory and most important diagnostic criterion. Typical localization of skin rashes: lower extremities - mainly legs and feet. Less commonly, the rash spreads to the thighs, torso, buttocks, upper limbs, and extremely rarely to the face. Hemorrhagic rash in most cases is represented by purpura , petechiae or a polymorphic rash , less often - urticarial, erythematous-macular elements or a bullous-necrotic form. The photo below of hemorrhagic vasculitis in adults shows various forms of skin syndrome.
Forms of skin syndrome of hepatitis B: a) hemorrhagic, b) urticarial; c) papulo-ulcerative; d) necrotic-ulcerative; e) polymorphic
Cutaneous hemorrhagic syndrome has a number of specific features. The rash is symmetrical, has a small-spotted/petechial character, while the size of the rash elements is 2-5 mm, protrudes above the surface of the skin, does not disappear with pressure, is prone to recurrence and fusion, has a pronounced variegation of rash elements due to the proximity of newly formed ones to old ones, which are at various stages of reverse development, are localized predominantly on the extensor surfaces of the limbs around the joints. Quite often, the onset of the disease is accompanied by various types of allergic rash - urticaria (allergic vasculitis).
In the early period of hepatitis B, the elements of the rash have a reddish color, but in the process of evolution they quickly acquire a characteristic bluish-purple color, then turn pale and within 3-5 days, as they develop back, they acquire a yellowish-brown tint. In severe cases, with high activity of the pathological process, some of the skin elements undergo necrosis, which is caused by microthrombosis and tissue ischemia. The skin syndrome of hepatitis B is characterized by a wave-like course, most often 2-5 episodes are observed. At the same time, newly appearing rashes can be caused by errors in diet, taking medications, or violation of bed rest. In some cases, the rash is accompanied by itching, and in 30-35% of patients hemosiderosis (residual long-term pigmentation) is observed, accompanied by peeling.
A common form of manifestation of skin syndrome can be angioedemalocalized on the hands, feet and face. In boys, swelling of the scrotum occurs. The tissues in the affected areas are bluish in color and pasty.
Articular form (syndrome). Involvement of joints in the pathological process is second in frequency of occurrence after skin syndrome. Quite often it occurs together with skin syndrome or appears several hours/days after it (cutaneous-articular form). Great difficulties in diagnosing hepatitis B are presented by cases in which the articular syndrome appears primarily, proceeds according to the type of migratory polyarthralgia/arthritis and precedes skin manifestations. Its development is based on impaired vascular permeability, which contributes to the development of swelling of the skin/subcutaneous fat in the area of medium/large joints, mainly the wrist and ankle; hemorrhages are less common. Small joints of the hand and foot are practically not involved in the pathological process.
Clinical changes in the joints are manifested by local hyperemia, increased volume, pain and tenderness on palpation, limitation of movements, and increased local temperature. Less commonly, painful contractures develop. Clinical symptoms develop against the background of an increase in body temperature to febrile levels and persist for 2-5 days, after which they disappear without a trace, leaving no deformities. Often articular syndrome occurs against the background of angioedema .
Abdominal syndrome . It occurs in 50-60% of patients and in a third of them it is preceded by skin syndrome, which significantly complicates diagnosis and is a common reason for surgical intervention. The main clinical sign is severe, sudden, cramping pain in the abdomen, without pronounced localization. The nature of the pain is similar to intestinal colic, more often in the navel, less often in the epigastric/right iliac region, often imitating the characteristic picture of a stomach ulcer , appendicitis , pancreatitis and even acute intestinal obstruction . The pain is often extremely intense, causing patients to take a forced position in bed, rushing about and screaming. The pain syndrome is caused by numerous hemorrhages in the intestinal wall, hemorrhages in the mesentery, hemorrhagic impregnation of the mucous membrane and intestinal wall, which can lead to the formation of areas of necrosis and bleeding. At the peak of pain, false urges with frequent bowel movements, vomiting mixed with blood, and the appearance of fresh blood in the stool are possible.
An objective examination reveals pain on palpation of the abdomen, bloating, however, signs of peritoneal irritation are usually absent. The duration of abdominal syndrome varies from several attacks over 2-3 days to 8-10 “waves” over several months. The syndrome is not constant, and the symptoms are unstable. Often, a relapse of abdominal pain is combined with another wave of skin manifestations.
Against the background of abdominal pain, patients may experience pale skin, a sunken face, a dry tongue, sunken eyes, and fever. With heavy bleeding, there is a high risk of developing acute posthemorrhagic anemia and collapse . Serious complications may include intestinal obstruction caused by the closure of its lumen with a hematoma, intestinal perforation , and peritonitis . The development of abdominal syndrome significantly aggravates the process and aggravates its course, requiring intensive therapy.
Kidney syndrome . Develops in approximately 30-50% of patients. This hepatitis syndrome always develops only after the appearance of a hemorrhagic rash, but it can join the symptom complex at different time periods of the disease. Most often, renal syndrome develops 1-2 months into the disease. There are 2 clinical variants of kidney damage:
- Transient urinary syndrome in the form of micro/macrohematuria or hematuria with moderate proteinuria in combination with other manifestations of the disease and with an undulating course.
- Schonlein-Henoch nephritis: occurs more often with a hematuric form, less often with a form of progressive glomerulonephritis and transition in 25-50% of cases to chronic glomerulonephritis, which sharply worsens the prognosis due to the presence of arterial hypertension/nephrotic syndrome and increases the risk of developing chronic renal failure. Therefore, careful monitoring of urine composition and kidney function throughout the disease is necessary.
The severity of clinical manifestations largely depends on the activity of the pathological process, according to which several degrees of severity of the course of hepatitis B are distinguished:
- Mild degree: skin rashes are not abundant, general condition is satisfactory, body temperature is subfebrile/normal, there are no signs of damage to organs/systems, ESR is up to 20 mm/hour.
- Moderate severity: the skin syndrome is clearly defined, the general condition is moderate, intoxication (weakness, headache, myalgia) and articular syndromes are pronounced, fever (hyperthermia over 38°C), abdominal/renal syndromes are moderate. In the blood - an increase in ESR to 40 mm/hour, an increase in eosinophils, leukocytes, neutrophils, dysproteinemia , hypoalbuminemia .
- Severe degree: the general condition is severe, the symptoms of intoxication are very pronounced (weakness, high fever, myalgia, headache). Almost all the main syndromes are expressed - skin, articular, renal, abdominal (paroxysmal abdominal pain, vomiting mixed with blood); there may be damage to the peripheral nervous system and central nervous system. In the blood there is anemia, severe leukocytosis, neutrophilia, ESR more than 40 mm/hour.
Henoch-Schönlein purpura can also occur with the involvement of other systems (cardiovascular, gastrointestinal tract, central nervous system) and organs (liver, lungs) in the pathological process, however, such variants of the disease are much less common.
KAWASAKI DISEASE (SYSTEMIC VASCULITIS) (ICD-10 code - M30.03)
Kawasaki disease is an acute arteritis of unknown etiology with a syndrome of fever, lesions of the skin, mucous membranes, lymph nodes and predominant damage to the coronary arteries. Most cases of the disease (85%) occur before the age of 5 years. Boys get sick 1.5 times more often than girls. The peak incidence occurs in the 1st year of life. There is no evidence of human-to-human transmission of the disease. The disease is considered one of the main causes of acquired heart and vascular diseases in children, and is ahead of rheumatic fever in frequency.
Rice. 1.
Conjunctivitis
Rice. 2.
Dry chapped lips
Rice. 3.
Raspberry tongue
Rice. 4.
Enlarged lymph nodes
tism, the incidence of which continues to decline, while the prevalence of Kawasaki disease increases.
DIAGNOSTICS
The main criteria for diagnosis are (in the absence of other reasons) - fever of 38 °C or higher for 5 days or more in combination with at least 4 of the 5 symptoms listed below: 1) polymorphic exanthema; 2) defeat
Rice. 5.
Kawasaki disease. Exanthema
Rice. 6.
Swelling of the hands (an early symptom of the disease)
Rice. 7.
Desquamation of the epithelium
mucous membranes of the oral cavity (at least one of the symptoms): diffuse erythema, catarrhal tonsillitis and/or pharyngitis, strawberry tongue, dry and cracked lips;
3) bilateral conjunctival hyperemia;
4) enlargement of cervical lymph nodes > 1.5 cm;
5) changes in the skin of the extremities (at least one of the symptoms): hyperemia and/or swelling of the palms and feet, peeling of the skin of the extremities in the 3rd week of the disease. The listed symptoms are observed in the first 2-4 weeks of the disease, which subsequently proceeds as systemic vasculitis. Cardiovascular lesions are observed in 50% of patients; myocarditis and/or coronaryitis are characteristic with the development of multiple aneurysms and occlusions of the coronary arteries, which can subsequently lead to myocardial infarction. 70% of patients have physical and electrocardiographic signs of heart damage. Joints, kidneys, gastrointestinal tract and central nervous system are often affected. Aneurysms form in large vessels, most often they are detected in the coronary arteries.
Tests and diagnostics
The diagnosis of hepatitis B is made by identifying specific clinical syndromes, first of all, the presence at the time of examination/history of skin hemorrhagic bilateral rashes and establishing a connection between the onset of breastfeeding and infectious diseases, an allergic history, and changes in diet. There are no specific laboratory tests. Laboratory research:
- OAC - thrombocytosis and nonspecific changes common to any inflammatory process, accelerated ESR, leukocytosis.
- OAM—hematuria/proteinuria.
- Biochemical blood test - blood for CRP, liver tests, creatinine, urea.
- Coagulogram - hypercoagulation is noted, accompanied by a decrease in the activity of antithrombin III and plasmin, and a decrease in chlorides.
- Immunogram - an increase in the concentration of IgA in the blood serum.
- Fecal occult blood test (positive for gastrointestinal bleeding).
In confirming the clinical diagnosis, a leading role is played by a skin biopsy and an immunohistochemical study to reveal the fixation of IgA-containing immune complexes in the vascular wall. If necessary, an ultrasound of the kidneys and abdominal organs and an ECG are prescribed.
Differential diagnosis is necessary with vasculitis in autoimmune diseases ( rheumatoid arthritis , Crohn's disease , systemic lupus erythematosus , ulcerative colitis ), vasculitis of infectious etiology, infections (hepatitis B and C, infectious subacute endocarditis , tuberculosis ), drug allergies and malignant neoplasms.
Diagnostics
Blood
- Changes in laboratory parameters are nonspecific for hemorrhagic vasculitis. There may be a slight increase in leukocytes and neutrophils in the general blood test. C-reactive protein and IgA also increase.
Urine
- A general urine test is prescribed.
- When the kidneys are damaged, micro- and macrohematuria (blood in the urine) occurs and excess protein is detected.
Ultrasound of the abdominal organs
- is done to exclude intussusception (pressing a section of intestine into another like a telescopic tube) in case of severe abdominal pain.
Diet
Hypoallergenic diet
- Efficacy: therapeutic effect after 21-40 days
- Timing: constantly
- Cost of products: 1300-1400 rubles. in Week
Diet Table No. 1
- Efficacy: therapeutic effect after 3 weeks
- Terms: 2 months or more
- Cost of products: 1500 - 1600 rubles. in Week
Diet 7 table
- Efficacy: therapeutic effect after a week
- Terms: 1 month or more
- Cost of products: 1200-1300 rubles per week
A hypoallergenic diet is prescribed, which involves excluding obligate allergens from the diet: milk, fish, citrus fruits, chocolate, cocoa, orange and red vegetables/fruits, as well as extractive substances. For abdominal syndrome, a modified Table No. 1 according to Pevzner is indicated until it is completely relieved. For nephritis - dietary Table No. 7 with a gradual transition to a hypochloride diet.
Prevention
The main measures to prevent hepatitis B in its relapses include:
- Adequate treatment of acute infectious diseases of the upper respiratory tract and timely sanitation of infectious chronic foci of ENT organs.
- Exclusion/minimization of contacts with allergens (if there is a history of allergic reactions) and control of medications.
- Preventing hypothermia of the body.
- Strengthening the immune system (hardening, rational nutrition).
- Dispensary observation of ill persons for 2 years.
Consequences and complications
The main complications of hepatitis B include: intestinal obstruction , pancreatitis , perforation , peritonitis , posthemorrhagic anemia , thrombosis / infarction in organs, neuritis , cerebral disorders. The lethal outcome develops mainly as a result of abdominal complications (intestinal perforation, peritonitis), the development of chronic renal failure , and hemorrhages in organs (brain).
Forecast
The prognosis is generally favorable and in 75% of cases patients recover within 1-2 years after the disease. In a number of patients with a chronic relapsing course, the disease can continue indefinitely with periodic relapses of one (skin) or several syndromes. The frequency of relapses throughout the entire period can vary from one to monthly, acquiring a monosyndromic character over time: mainly in the form of cutaneous purpura or a skin-articular form, less often - chronic nephritis in the form of a hematuric form with preservation of kidney function over a long period.
The prognosis is less unfavorable with the development of nephritis , especially when the process becomes chronic with manifestations of glomerulonephritis and transition to chronic renal failure. Purpura fulminans has a poor prognosis.
Symptoms and signs of vasculitis
Symptoms of vasculitis vary. They depend on the nature of the lesion, the type of vasculitis, the localization of the inflammatory process, as well as the severity of the underlying disease.
Despite the variety of options, many patients have some of the same symptoms: fever, hemorrhagic skin rash, weakness, exhaustion, joint pain and muscle weakness, lack of appetite, weight loss, numbness in certain parts of the body.
Thromboangiitis obliterans (or Buerger's disease) is associated primarily with damage to the blood vessels of the extremities, manifested by pain in the legs and the appearance of large ulcers on the skin (cutaneous vasculitis on the legs).
Kawasaki disease primarily affects children under five years of age and has typical signs of vasculitis (redness of the skin, fever, and possibly eye inflammation).
Periarteritis nodosa mainly affects the middle blood vessels in various parts of the body, including the kidneys, intestines, heart, nervous and muscular systems, and skin. The skin is pale, and the rash with this type of vasculitis is purple.
Microscopic polyangiitis mainly affects small vessels in the skin, lungs and kidneys. This leads to pathological changes in organs and disruption of their functions. The disease is characterized by significant skin lesions, fever and weight loss in patients, the appearance of glomerulonephritis (immune damage to the glomeruli of the kidneys) and hemoptysis (pulmonary vasculitis)
Cerebral vasculitis (or brain vasculitis) is a serious disease characterized by inflammation of the walls of blood vessels in the brain. May lead to hemorrhage and tissue necrosis. The causes of this type of vascular vasculitis are still being clarified.
Takayasu's disease affects the large arteries of the body, including the aorta. Young women are at risk. Signs of this type are weakness and pain in the arms, weak pulse, headaches and vision problems.
Giant cell arteritis (Horton's disease). The process primarily affects the arteries of the head. Characterized by attacks of headaches, hypersensitivity of the scalp, pain in the jaw muscles when chewing, visual impairment up to blindness.
Scheleyn-Henoch vasculitis (hemorrhagic vasculitis) is a disease that mainly affects children, but also occurs in adults. The first signs of hemorrhagic vasculitis may appear 1-4 weeks after infectious diseases such as scarlet fever, ARVI, tonsillitis, etc. Leads to inflammation of the blood vessels of the skin, joints, intestines and kidneys. It is characterized by pain in the joints and abdomen, blood in the urine, redness of the skin on the buttocks, legs and feet.
Cryoglobulinemic vasculitis may be associated with infection with hepatitis C. The patient feels general weakness, develops arthritis, and purple spots on his legs.
Wegener's granulomatosis causes inflammation of the blood vessels in the nose, sinuses, lungs and kidneys. Typical symptoms of the disease are nasal congestion, as well as frequent nosebleeds, middle ear infections, glomerulonephritis and pneumonia.
List of sources
- Lyskina G. A. Systemic vasculitis. In the book: Pediatric rheumatology. Guide for doctors / Ed. A. A. Baranova, L. K. Bazhenova. M.: Medicine, 2002. pp. 221–270.
- Kulaga V.V., Romanenko I.M., Afonin S.L. Allergic diseases of the blood vessels of the skin. Lugansk: “Etalon-2”, 2006. 168 p.
- A practical guide to childhood diseases, edited by prof. Kokolina V.F. and prof. A.G. Rumyantsev, volume IV. Hematology/oncology of childhood (edited by Rumyantsev A.G. and E.V. Samochatova). Medical practice – M. Moscow 2004 Zinovieva G.A., Frolkova E.V. Hemorrhagic vasculitis. Clinic and treatment // ros. pediatrician, journal — 1998. -N12. P.24-26.
- Krivosheev O.G., Gulyaev CB, Semenovykh A.G. Modern principles of treatment of Henoch-Schönlein purpura // Doctor. 2007. No. 4. -P.54-55.
Causes of diagnostic errors in vasculitis
Unfortunately, diagnostic errors in situations involving systemic vasculitis are not uncommon. There are several reasons for such errors.
- Firstly, primary systemic vasculitis is a rare (orphan) disease, and doctors working in regular medical institutions, and not in specialized centers, simply cannot accumulate the necessary experience in recognizing and treating these diseases. Although in recent years there has been a trend towards an increase in systemic vasculitis throughout the world.
- Secondly, for a long time, the clinical picture of most primary systemic vasculitis is nonspecific and includes only such common symptoms as fever, general weakness, loss of appetite and body weight, skin rashes, joint pain, etc., which are inherent in addition to vasculitis , and many other diseases.
- Thirdly, situations are possible when systemic vasculitis resembles in its course an infectious disease, tumor or other disease. For example, granulomatosis with polyangiitis (Wegener's) with damage to the tissues of the orbit of the eye is almost universally interpreted in the first stages of examination as a malignant tumor of the orbit. The same Wegener's granulomatosis with a predominant lesion of the sinuses or middle ear resembles ordinary sinusitis and otitis media. Wegener's granulomatosis, which primarily affects the lungs, mimics tuberculosis or lung cancer. Eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome) often, during the first few months or even years, manifests itself only in attacks of suffocation, indistinguishable from asthmatic ones.
Giant cell (temporal) arteritis is a disease that develops in people over 50 years of age and usually manifests itself as headache in the temple, crown or back of the head, as well as blurred vision, is often mistakenly interpreted as “cerebral atherosclerosis”, “migraine”, “neuritis” trigeminal nerve", "glaucoma", etc. Such diagnostic errors are typical for all rare diseases: a rare disease is initially mistaken for an atypical form of a more common disease.