With high blood pressure, the patient requires emergency care to avoid a hypertensive crisis. Doctors treat high blood pressure with medications. Monopril is considered one of the effective drugs for hypertension. This is a drug belonging to the pharmacological group of angiotensin-converting enzyme inhibitors. Monopril lowers blood pressure, rarely causes side effects and is well tolerated by patients. In order for the drug to work effectively, you must follow the instructions for use and doctor's instructions.
Release form
Monopril is a white, round, biconvex, odorless tablet, scored on one edge and engraved “609” or “158” on the other.
Available according to:
- 14 such tablets of 20 mg in a blister, two blisters in a paper pack;
- 10 such tablets of 10 mg each in a blister made of plastic and aluminum foil, one or two blisters in a paper pack;
- 14 such tablets of 10 mg each in a blister made of plastic and aluminum foil, one or two blisters in a paper pack.
Use in old age
Elderly patients do not require dosage adjustment. the drug is well tolerated at any age, the hypotensive effect does not decrease. In elderly patients, individual susceptibility to the components of the tablets may increase due to slower elimination, which threatens overdose.
In old age there is a danger of drug overdose
Pharmacodynamics and pharmacokinetics
Pharmacodynamics
Angiotensin-converting enzyme inhibitor. Chemically, fosinopril sodium is the sodium salt of fosinoprilat ester. Fosinoprilat is a selective competitive angiotensin-converting enzyme . After inhibiting ACE, it prevents the transformation of angiotensin type 1 into angiotensin type 2, which has a vasopressor effect. This leads to a decrease in the content angiotensin in the blood - this causes a decrease in its vasoconstrictor activity and a weakening of aldosterone .
Fosinoprilat inhibits the metabolism of bradykinin and therefore its antihypertensive effect is enhanced. The decrease in pressure is not accompanied by a decrease or increase in circulating blood volume, renal and cerebral blood flow, or blood supply to organs. After internal administration, the antihypertensive effect occurs within one hour, becomes maximum after 2-5 hours and lasts up to a day. Several weeks are necessary to achieve the greatest therapeutic effect.
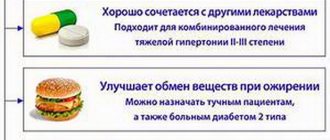
The antihypertensive effects of thiazide diuretics and fosinopril are complementary.
The drug helps reduce sensitivity to physical activity and reduce the severity of heart failure.
Pharmacokinetics
After oral administration, absorption from the intestine reaches 30-40% and does not depend on food intake. Maximum plasma concentration occurs after three hours. Interaction with blood proteins reaches 95%.
Enzymatic hydrolysis of the drug occurs in the liver and intestinal mucosa. Fosinoprilat is excreted equally through the digestive tract and kidneys. The half-life is close to 11 hours.
Pharmacological properties
Pharmacodynamics - increases or decreases blood pressure
The main active ingredient of the drug is fosinopril sodium. This is the sodium salt of fosinoprilat. In the body, the substance undergoes hydrolysis, breaking down into enzymes, fosinoprilat is released, which is an angiotensin-converting enzyme inhibitor. The action is aimed at blocking the conversion of the hormone angiotensin 1 into the enzyme angiotensin 2. The amount of the enzyme angiotensin 2 in the blood decreases, reducing the secretion of aldosterone. Angiotensin 2 is produced by the body and has an effect on the walls of blood vessels, which narrow. ACE inhibitor drugs prevent the enzyme from being produced, so the blood vessels remain dilated and the pressure decreases. Decreased aldosterone production leads to a slight increase in the number of sodium ions and a decrease in fluid volume.
Fosinoprilat reduces blood pressure by slowing down the metabolic processes of bradycardin, which is a strong vasodilator. This enhances the hypotensive effect.
When pressure levels decrease, the level of blood supply to the kidneys and brain does not change, the volume of circulating blood remains the same. A decrease in blood pressure does not entail a reduction in the reflex capacity of the myocardium, blood flow to the internal organs, skeleton and skin.
Monopril belongs to the group of ACE inhibitors
In order for Monopril to act faster against pressure, it is necessary to lay the patient down or ask him to stand for a while. The drug begins to act 60 minutes after use. The maximum effect is observed after 2-6 hours. The effect of one tablet lasts for a day. To stabilize the condition, it is necessary to take Monopril for several weeks.
If there is insufficient circulating blood volume or a salt-free diet while taking the drug, the heart rate sometimes increases or orthostatic collapse occurs.
To enhance the antihypertensive effect, the doctor may prescribe thiazide diuretics in combination with Monopril.
The medication helps with blood pressure at any age, regardless of the patient’s gender or weight.
Monopril blood pressure tablets do not cause a withdrawal reaction, so it is allowed to immediately stop using the tablets without gradually reducing the dosage.
The drug inhibits the active activity of the renin-angiotensin system, which has a positive effect on the course of chronic heart failure. The drug reduces the load on the heart and myocardium.
Pharmacokinetics of the drug
The drug is taken orally. When it enters the stomach, the tablet breaks down into enzymes under the action of gastric juice. Absorption is 30-40%. Eating does not affect the degree of absorption, but reduces the rate of enzyme breakdown. The maximum concentration of the active substance is reached 3 hours after application. The tablets bind well to the blood, binding to plasma proteins is 95%.
Metabolism occurs in the stomach and partly in the liver. Metabolites are excreted through the intestines and kidneys.
With normal liver and kidney function, the elimination time of the components is 11.5 hours; if heart failure is detected in the chronicle, the elimination period increases to 14 hours.
In case of renal failure, the rate of cleansing the body of metabolites is reduced by half. Impaired renal function does not affect absorption, bioavailability or blood binding. Metabolites are excreted through the intestines with bile.
With hemodialysis, the rate of cleansing the body of drug metabolites is 2 and 7 percent.
In liver failure and cirrhosis, the rate of breakdown of fosinoprilat into metabolites decreases. The rate of cleansing the body of metabolites is reduced by half.
Monopril is a fast-acting drug
Contraindications
- Quincke's edema.
- Hypersensitivity to any of the components of the drug.
- Age up to 18 years.
- Pregnancy or lactation.
Use with caution when:
- hyponatremia;
- bipolar renal artery stenosis ;
- desensitization;
- aortic stenosis;
- condition after kidney transplantation;
- renal failure;
- systemic connective tissue lesions;
- hemodialysis;
- cerebrovascular diseases;
- coronary heart disease ; heart failure of the chronic type 3–4 degrees;
- diabetes mellitus;
- hyperkalemia;
- inhibition of hematopoiesis in the bone marrow;
- gout;
- in old age;
- conditions accompanied by a decrease in circulating blood volume.
Monopril
Arterial hypotension
In patients with uncomplicated arterial hypertension, arterial hypotension may develop due to the use of fosinopril. Symptomatic arterial hypotension when using ACE inhibitors more often develops in patients during intensive treatment with diuretics, a diet associated with limiting sodium chloride, or during dialysis. Transient arterial hypotension is not a contraindication for the use of fosinopril after measures to restore blood volume.
In patients with chronic heart failure, treatment with ACE inhibitors may cause excessive antihypertensive effects, which can lead to oliguria or azotemia and, in rare cases, fatal acute renal failure. Therefore, when treating chronic heart failure with fosinopril, patients should be closely monitored, especially during the first 2 weeks of treatment, as well as with any increase in the dose of fosinopril or diuretic.
It may be necessary to reduce the diuretic dose in patients with normal or low blood pressure, who have previously received diuretic therapy, or who have hyponatremia. Arterial hypotension as such is not a contraindication for further use of fosinopril in chronic heart failure. Some reduction in systemic blood pressure is a common and desirable effect when initiated in chronic heart failure. The extent of this reduction is greatest early in treatment and stabilizes within one or two weeks of starting treatment. Blood pressure usually returns to baseline levels without a decrease in therapeutic efficacy.
Before starting treatment, it is necessary to analyze previous antihypertensive therapy, the degree of increase in blood pressure, dietary restrictions on salt and/or liquid, and other clinical circumstances. If possible, previous antihypertensive therapy should be discontinued several days before starting treatment. To reduce the likelihood of arterial hypotension, diuretics should be discontinued 2-3 days before starting treatment. Before and during treatment, it is necessary to monitor blood pressure, renal function, the content of potassium ions, creatinine, urea, electrolyte concentrations and the activity of liver enzymes in the blood.
Aortic or mitral stenosis/hypertrophic obstructive cardiomyopathy
Like all drugs that have a vasodilating effect, ACE inhibitors should be used with extreme caution in patients with left ventricular outflow tract obstruction.
Renal dysfunction
In patients with arterial hypertension with unilateral or bilateral renal artery stenosis or stenosis of the artery of a solitary kidney, the concentration of blood urea nitrogen and serum creatinine may increase during treatment with ACE inhibitors. These effects are usually reversible and disappear after treatment is stopped. It is necessary to monitor renal function in such patients in the first weeks of treatment. In some patients, increases in blood urea nitrogen and serum creatinine concentrations (usually small and transient) may be observed even without obvious renal impairment during concomitant use of fosinopril and diuretics. A dose reduction of fosinopril may be required.
In patients with severe chronic heart failure, renal function may be dependent on the activity of the renin-angiotensin-aldosterone system, so treatment with ACE inhibitors may be accompanied by oliguria and/or progressive azotemia, and in rare cases, acute renal failure and death.
Kidney transplant
There is no experience with the use of fosinopril in patients who have recently undergone kidney transplantation.
Liver dysfunction
In rare cases, when using ACE inhibitors, a syndrome is observed, the first manifestation of which is cholestatic jaundice. This is followed by fulminant liver necrosis, sometimes fatal. The mechanism of development of this syndrome has not been studied. If noticeable icterus and a marked increase in liver enzyme activity occur, fosinopril treatment should be discontinued and appropriate treatment should be prescribed.
In patients with impaired liver function, increased plasma concentrations of fosinopril may be observed. In liver cirrhosis (including alcoholic cirrhosis), the apparent total clearance of fosinoprilat is reduced, and the AUC is approximately 2 times higher than in patients without liver dysfunction.
Neutropenia / agranulocytosis / thrombocytopenia / anemia
It is possible to develop agranulocytosis and suppression of bone marrow function during treatment with ACE inhibitors. These cases occur more often in patients with impaired renal function, especially in the presence of systemic connective tissue diseases (SLE or scleroderma). Before starting therapy with ACE inhibitors and during treatment, leukocytes and leukocyte formula are determined (once a month in the first 3-6 months of treatment and in the first year of fosinopril use in patients with an increased risk of neutropenia).
Hypersensitivity reactions/angioedema
The development of angioedema of the extremities, face, lips, mucous membranes, tongue, pharynx or larynx has been reported in patients receiving fosinopril. Swelling of the tongue, pharynx, or larynx can cause airway obstruction, which can be fatal. In such cases, it is necessary to stop taking fosinopril and take emergency measures, including subcutaneous injection of epinephrine (adrenaline) solution (1:1000), as well as other emergency treatment measures. In most cases of swelling of the face, oral mucosa, lips and extremities, stopping fosinopril resulted in normalization of the condition; however, appropriate therapy was sometimes required.
Swelling of the intestinal mucosa
Swelling of the intestinal mucosa has rarely been observed while taking ACE inhibitors. Patients complained of abdominal pain (there may have been no nausea and vomiting); in some cases, swelling of the intestinal mucosa occurred without swelling of the face; C1-esterase activity was normal. Symptoms disappeared after stopping the use of ACE inhibitors. Edema of the intestinal mucosa should be included in the differential diagnosis of patients taking ACE inhibitors who complain of abdominal pain.
Patients with a history of angioedema not associated with ACE inhibitors may be at greater risk of developing angioedema during ACE inhibitor therapy.
In representatives of the Negroid race, cases of the development of angioedema when using ACE inhibitors were observed with a higher frequency compared to representatives of other races.
An increased risk of angioedema was observed in patients concomitantly taking ACE inhibitors and drugs such as mTOR inhibitors (temsirolimus, sirolimus, everolimus), dipeptidyl peptidase type IV inhibitors (sitagliptin, saxagliptin, vildagliptin, linagliptin), estramustine, neutral endopeptidase inhibitors (racecadotril). , sacubitril) and tissue plasminogen activators.
Anaphylactic reactions during desensitization
In two patients, during desensitization with hymenoptera venom while taking the ACE inhibitor enalapril, life-threatening anaphylactoid reactions were noted. In the same patients, these reactions were avoided by timely interruption of the ACE inhibitor; however, they reappeared after inadvertent resumption of an ACE inhibitor. Particular care should be taken when desensitizing patients taking ACE inhibitors.
Anaphylactoid reactions during low-density lipoprotein apheresis (LDL apheresis)
Life-threatening anaphylactoid reactions have rarely been observed in patients taking ACE inhibitors during LDL apheresis using dextran sulfate. The development of these reactions can be prevented by temporarily discontinuing the ACE inhibitor before each LDL apheresis procedure.
Hemodialysis using high-flow membranes
When performing hemodialysis in patients receiving ACE inhibitors, the use of high-flow polyacrylonitrile dialysis membranes (for example, AN69) should be avoided, since in such cases the risk of developing anaphylactoid reactions increases. In such cases, it is necessary to use a different type of dialysis membrane or use antihypertensive drugs of other classes.
Cough
When using ACE inhibitors, including fosinopril, a non-productive, persistent cough was observed, which disappeared after discontinuation of therapy. When cough occurs in patients taking ACE inhibitors, this therapy should be considered as a possible cause in the differential diagnosis.
Surgical interventions / general anesthesia
ACE inhibitors may enhance the antihypertensive effect of drugs used for general anesthesia. Before surgery (including dentistry), you must warn your doctor/anesthesiologist about the use of ACE inhibitors. Caution should be exercised when performing physical exercise or in hot weather due to the risk of dehydration and hypotension due to a decrease in blood volume.
Hyperkalemia
There have been cases of increased levels of potassium ions in the blood serum of patients taking ACE inhibitors, incl. fosinopril At risk in this regard are patients with renal failure, type 1 diabetes mellitus, as well as those taking potassium-sparing diuretics (such as spironolactone, eplerenone, triamterene or amiloride), potassium supplements, potassium-containing nutritional supplements or other drugs that increase the level of potassium ions in the serum blood. If necessary, simultaneous use of fosinopril and the above potassium-containing or increasing potassium levels in the blood plasma drugs should be used with caution and regularly monitor the potassium level in the blood serum.
Dual blockade of the renin-angiotensin-aldosterone system (RAAS)
The simultaneous use of drugs from different groups that act on the RAAS is not recommended (double blockade of the RAAS), since it has been associated with an increased incidence of side effects such as arterial hypotension, hyperkalemia, and decreased renal function (including acute renal failure).
The simultaneous use of ACE inhibitors with drugs containing aliskiren is contraindicated in patients with diabetes mellitus and/or with moderate or severe renal impairment (GFR less than 60 ml/min/1.73 m2 body surface area) and is not recommended in other patients.
Concomitant use of ACE inhibitors with angiotensin II receptor antagonists is contraindicated in patients with diabetic nephropathy and is not recommended in other patients.
Ethnic differences
ACE inhibitors are less effective in blacks than in Caucasians, which may be due to the higher prevalence of low renin activity in blacks.
Side effects
The most likely side effects of Monopril.
- From the circulatory system: chest pain, fainting, orthostatic hypotension , hot flashes, arrhythmia .
- Digestive disorders: vomiting, dyspepsia, pancreatitis ALT and AST levels , hepatitis .
- From the nervous system: sensory disturbances, feeling of fatigue.
- From the genitourinary system: oliguria, proteinuria , increased concentrations of creatinine and urea .
- From the respiratory system: sinusitis, pharyngitis , cough, bronchospasm .
- From the musculoskeletal system: pain in joints and muscles.
- Allergic reactions: photosensitivity , itching , rash , Quincke's edema .
Possible side effects
While taking the blood pressure drug Monopril, the body may experience adverse reactions:
- heart and blood vessels: strong heartbeat, sharp decrease in pressure to critical levels, facial hyperemia, tachycardia, orthostatic collapse, fainting, angina pectoris, cardiac arrhythmia, heart block, swelling, heart attack, increased blood pressure, cardiac arrest, death;
- digestive system: loss of appetite, vomiting, bloating, loose stools, difficulty defecating, acute abdominal pain, intestinal obstruction, bleeding, hepatitis, inflammation of the pancreas, cholestasis, damage to the oral mucosa, impaired swallowing, inflammation of the tongue, weight fluctuations , complete refusal to eat, dry mouth;
- respiratory organs: dyspnea, dry cough, narrowing of the bronchial lumen, pneumonia, infiltration in the lungs, nasal congestion, voice disorder, inflammation of the mucous membranes of the larynx, rhinosinusitis, pharyngitis, inflammation of the large bronchi and trachea, nosebleeds;
- urinary system: kidney failure, enlarged prostate gland, the appearance of protein in the urine, insufficient or increased urine formation;
- organs of perception: ear ringing, ear pain, auditory and visual disorders, impaired taste perception;
- nervous system: dizziness, headaches, cerebral ischemia, acute disturbance of cerebral blood supply, impaired coordination of movements, memory disorders, lethargy, insomnia, drowsiness, depression, increased anxiety, clouding of consciousness, sensitivity disorder;
- lymphatic system: inflammation of the lymph nodes;
- metabolism: gout;
- musculoskeletal system: muscle weakness, muscle pain, arthritis, musculoskeletal pain;
- allergic reactions: rashes, itching, skin inflammation, Quincke's edema;
- laboratory data: increased venous blood level, increased blood creatinine level, increased liver alanine aminotransferase, increased bilirubin level, decreased sodium level, increased potassium level, decreased hematocrit, decreased hemoglobin level, increased ESR, low neutrophil, low white blood cell count, increased number of eosinophils;
- influence on the child in the womb: limited mobility of the limbs, hypoplasia of the skull, underdevelopment of all structural elements of the lungs, congenital underdevelopment of the kidneys, low blood pressure, oligohydramnios, excess potassium;
- other reactions: increased sweating, increased temperature, decreased libido or impotence.
Dry cough may be one of the side effects
Instructions for use of Monopril (Method and dosage)
Instructions for use of Monopril recommend taking the drug orally. The dosage is selected individually.
Arterial hypertension . The initial dose is 10 mg once a day. It is necessary to select the dose by observing the dynamics of pressure reduction. The standard dose ranges from 11-40 mg once daily. If there is no sufficient hypotensive effect, additional diuretics .
Heart failure . The initial dose is 5 mg up to two times a day. Over time, the dose can be increased to 40 mg per day.
Brief information about the drug
Release form
The drug Monopril is produced in the form of tablets. These are round, biconvex tablets of white color without a characteristic odor. On one side there is a risk, which helps you choose the right dosage. On the reverse side there is an engraving “609”.
Each tablet is packaged in an individual blister cell. One blister contains 14 tablets. Blisters are packed in a cardboard box (28 tablets). The kit includes instructions for using Monopril.
Composition of tablets
The main active ingredient of the drug is fosinopril sodium. Each tablet contains 20 mg of the substance.
Other components of the medicine:
- polyvinylpyrrolidone;
- microcrystalline cellulose;
- lactobiose;
- sodium stearyl fumarate;
- crospovidone.
Monopril tablets
Terms and conditions of storage
The drug should be stored out of the reach of children at a temperature of 15 to 25 degrees. The shelf life of the medicine is 2 years from the date of production. After the expiration date, any remaining drug must be disposed of in accordance with sanitary standards.
Terms of sale
The drug is sold in pharmacies with a doctor's prescription.
Price
The price of Monopril starts from 400 rubles.
Overdose
Signs: severe decrease in blood pressure, bradycardia, shock , water-mineral imbalance, acute renal failure, stupor.
Therapy: stop taking Monopril, gastric lavage, use of sorbents, vasopressors , intravenous saline, then symptomatic and supportive therapy. Hemodialysis is ineffective.
Monopril overdose
In case of an overdose, the patient develops characteristic symptoms:
- disturbance of water-electrolyte metabolism;
- a sharp decrease in pressure indicators to critical values;
- sinus rhythm disturbance;
- mental depression;
- kidney failure;
- state of shock.
In case of overdose, it is necessary to stop using Monopril, rinse the stomach, drink an adsorbent, a vasopressor, and administer a sodium chloride solution drip. Hemodialysis will not bring any effect. The rest of the treatment is carried out by the attending physician based on symptoms.
Interaction
Concomitant use with antacids reduces the absorption of fosinopril , so they should be taken at intervals of 2 hours.
When used together with lithium salts, lithium intoxication increases .
Nonsteroidal anti-inflammatory drugs suppress the antihypertensive effect of Monopril and similar drugs.
When using the drug simultaneously with diuretics, an excessive decrease in blood pressure may develop.
Drugs containing potassium and potassium-sparing diuretics increase the likelihood of developing hyperkalemia .
Fosinopril activates the hypoglycemic effect of insulin and sulfonylurea ; increases the risk of leukopenia when used with cytostatic agents, immunosuppressants, Allopurinol, Procainamide.
Estrogens suppress the antihypertensive effect of Monopril.
Pregnancy and breastfeeding period
Monopril for hypertension should not be taken during pregnancy. In the second or third trimester, taking the medication can lead to severe internal pathologies or fetal death.
If a woman finds out she is pregnant while undergoing treatment with Monopril, she must immediately stop taking the drug. The doctor should warn the pregnant woman about possible pathologies and the negative effects of the pills on the fetus. After discontinuation of the drug, an additional examination of the pregnant woman is carried out to exclude a negative effect on the intrauterine development of the fetus.
If oligohydramnios is detected, Monopril is discontinued. The doctor may leave the pills during pregnancy or during oligohydramnios, if the risk to the health and life of the mother outweighs the possible negative consequences for the child.
If a pregnant woman took an ACE inhibitor during gestation, the child may have congenital pathologies: excess potassium in the blood, a decrease in the amount of urine excreted by the kidneys, low blood pressure. Infants should be under special supervision by a doctor during the first days of life. If oliguria is detected, the doctor monitors blood pressure readings and performs renal perfusion. To normalize blood pressure, your doctor may give blood transfusions and dialysis. Hemodialysis is not performed on newborns.
The components of Monopril pass into breast milk, so the tablets should not be taken while breastfeeding a baby. If Monopril therapy cannot be excluded, the woman should stop breastfeeding.
Analogues of Monopril
Level 4 ATC code matches:
Dilaprel
Prenesa
Enap
Diroton
Lipril
Renipril
Parnavel
Fozinap
Tritace
Enam
Zokardis
Fosinopril
Lisinopril
Captopril
Renitek
Hartil
Phosicard
Amprilan
Ramipril
Perindopril
The most common analogues of Monopril: Fosicard , Fosinap, Fozinotec, Fosinopril-Teva.
Monopril price, where to buy
The price of Monopril 20 mg No. 28 in Russia fluctuates around 309-430 rubles, in Ukraine – 173-273 hryvnia.
- Online pharmacies in RussiaRussia
ZdravCity
- Monopril tablets 20 mg 28 pcs. Bristol Myers Squibb CpL/ICN Polfa Rzeszow SA
492 rub. order
Pharmacodynamics
Fosinopril is an ester that is hydrolyzed in the body by enzymes into the active compound fosinoprilate. Due to the specific connection of the phosphinate group with ACE, it prevents the conversion of angiotensin I into the vasoconstrictor substance angiotensin II, which leads to vasodilation and a decrease in aldosterone secretion. The latter effect may lead to a slight increase in serum potassium ion concentration (average 0.1 mEq/L) and a decrease in sodium ion concentration and fluid volume. Fosinopril inhibits the metabolism of the bradykinin peptide, which has a powerful vasodilating effect, due to which the antihypertensive effect of the drug may be enhanced.
A decrease in blood pressure is not accompanied by changes in blood volume, cerebral and renal blood flow, blood supply to internal organs, skeletal muscles, skin, or reflex activity of the myocardium. After oral administration, the hypotensive effect develops within 1 hour, reaches a maximum after 3–6 hours and persists for 24 hours.
In heart failure, the positive effects of Monopril® are achieved mainly through inhibition of the renin-aldosterone system. Suppression of ACE leads to a decrease in both preload and afterload on the myocardium.
The drug helps to increase tolerance to physical activity and reduce the severity of heart failure.