Stroke is a very dangerous disease and is becoming more and more “youthful”: if previously it was mainly older people who suffered from it, now it is not uncommon for young people to be hospitalized with this diagnosis. This happens most often due to overwork.
But older people with chronic diseases still need to take special care - some contribute to stroke, and also make it more difficult to recover.
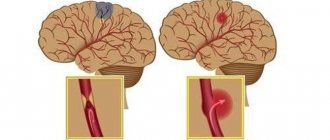
There are ischemic and hemorrhagic strokes. They differ in many respects and are treated differently, but it is not always easy to distinguish them - many of the symptoms are similar, because in both cases the problem is a violation of blood flow in the head, although its causes are different.
Causes and risk factors
Ischemic stroke can have a variety of causes:
- stress, which provokes the release of catecholamines into the blood - when there is an excess of them, the blood vessels narrow and the blood supply to the brain suffers;
- heart pathology;
- diabetes;
- spasm of the carotid arteries;
- smoking – it damages the endothelium of the arteries;
- other.
Hemorrhagic stroke has its own set of causes, which are very different. Among them:
- amyloid angiopathy;
- inflammation of blood vessels;
- stress;
- constant overwork;
- poor blood clotting;
- incorrect use of certain medications;
- drug use.
Risk factors include:
- overwork leading to chronic fatigue;
- frequent stress;
- obesity;
- bad habits;
- hemophilia;
- a number of other diseases.
Each of these factors increases the likelihood of a stroke, and if several are combined, you should take special care of your health, since otherwise problems are inevitable.
A transient ischemic attack indicates that an ischemic stroke may soon occur. It may cause some part of the body to become numb for a short time and may also cause nausea. a feeling of disorientation, blurred vision and other symptoms.
Usually last no more than 15 minutes (mild) to several hours (moderate), or up to a day (severe).
Other warning signs of stroke:
- excessive excitement or lethargy;
- noise in ears;
- fainting;
- sleep problems;
- decreased performance and inability to concentrate;
- headaches without localization, aggravated by fatigue or changes in weather;
- dizziness, especially severe when walking.
If such signs recur, they cannot be ignored. With timely treatment and initiation of treatment, ischemic stroke can be avoided. Another thing is hemorrhagic. It often develops suddenly, without any warning at all. But sometimes they still exist:
- numbness of half the face;
- sharp pain in the eyes and partial loss of vision;
- difficulty understanding speech;
- inability to maintain balance.
They appear shortly before the onset of a stroke, so measures must be taken immediately.
Briefly about the main thing - features of ischemia and hemorrhage
{banner_banstat0}
There are two main types of stroke:
- Ischemic
. Leads to contraction of blood vessels in the head, which clogs their walls, causing hypoxia. - Hemorrhagic
. The process of bleeding into the brain, often fatal.
According to statistics, the ratio between the two species is 80% to 20% (Consilium Medicum No. 02 2000).
Ischemic stroke can develop at any age - in children, adolescents, middle-aged people and the elderly. The severity of the consequences is also individual, depending on the speed of decision-making after the attack, the correct diagnosis, and the prescribed treatment.
Hemorrhagic stroke can happen to a person of any age. It occurs suddenly and is accompanied by a serious condition of the patient, constant gag reflexes and severe headache. At the first signs, a person often loses consciousness.
Causes:
- sudden movements, change of position;
- food with a lot of fat and other harmful ingredients;
- bad habits - smoking, alcohol addiction, drug addiction;
- high water temperature during water procedures or outdoors;
- excessive physical or psychological load on the human body;
- cardiac arrhythmia;
- blood pressure problems.
Information about stroke - clickable
When the first symptoms of a stroke appear, you should be careful and prompt; minutes count. On average, 3-4 hours after the first signs appear, the condition of the blood vessels in the brain deteriorates, and the consequences may become irreversible. The first 3-4 hours are the most important in the fight against the disease.
If the signs and pain go away within 24 hours, the person most likely had a mini-stroke.
Symptoms of left-sided and right-sided strokes differ
Algorithm of actions when symptoms appear:
- Place the patient on a horizontal surface, holding his head at an angle of 30 degrees.
- If the victim feels sharp gag reflexes, you need to turn his head to the side.
- You should carefully monitor changes in blood pressure and pulse. It is recommended to measure them and monitor fluctuations.
- When emergency doctors appear, you should fully describe the picture of what happened. Tell what actions were taken before the doctors arrived.
Symptoms
Following the warning signs, the first symptoms appear. Feeling can deteriorate very quickly after this, so the speed of response is one of the main factors that can ensure survival.
The first symptoms may appear several hours before an ischemic stroke: weakness, headaches and dizziness, fainting. Limbs may be lost on one side or vision may be impaired - in some cases only affecting one eye.
Other signs that can help identify ischemic stroke:
- the patient perceives reality incorrectly;
- his speech becomes unclear;
- pulse quickens;
- the pressure rises and falls;
- auditory perception deteriorates;
- he has difficulty swallowing;
- there is noise in the head;
- movements are not coordinated;
- nausea;
- heat;
- the face is distorted;
- pain appears that a person has not experienced before, for example, the chest or half of the face begins to ache.
The following symptoms indicate a hemorrhagic stroke:
- the head begins to hurt very badly;
- arrhythmia or tachycardia occurs;
- pressure rises;
- breathing becomes loud and hoarse;
- the patient may faint;
- photosensitivity increases;
- the face becomes asymmetrical, turns red or pale;
- convulsions begin;
- the gaze loses its meaning;
- nausea or even vomiting begins;
- limbs or the whole body are paralyzed;
- bowel movements involuntarily.
Diagnostics
If warning signs appear, you should consult a doctor as soon as possible. He will conduct a simple test to make a preliminary diagnosis. The patient will need:
- Smile - if the lips on one side do not obey, the smile will turn out crooked.
- Extend your arms - they should be kept at the same level.
- Say something meaningful - for example, your full name.
- Stick out your tongue - it should not deviate to the side or sink.
By how these exercises are performed, it will be possible to determine whether the patient has suffered a stroke or whether the cause should be sought elsewhere. If signs indicate a stroke, the diagnosis is clarified using tomography and other procedures.
First aid and treatment
An ambulance should be called immediately at the first suspicion. Until she arrives, you will need to provide assistance yourself:
- lay the victim down and raise his head;
- make sure that his clothing does not restrict breathing;
- make sure that your tongue does not sink;
- do not give anything to drink or eat;
- ventilate the room;
- cool your head with compresses;
- when vomiting, make sure that he does not suffocate; his head should be turned to the side;
- If necessary, perform chest compressions or artificial respiration.
Please note: no medications should be used without consulting a doctor; in this condition, taking them can be extremely dangerous.
There are several stages in the treatment of stroke:
- first aid;
- hospital treatment;
- rehabilitation.
It is very important to provide first aid correctly, because it is the first hours of a stroke that are most often decisive: if time is lost, death is very likely. If everything went well, then intensive therapy is carried out in the hospital, with the help of which they try to ensure that the brain is damaged as little as possible, and also to prevent a recurrent stroke.
Gradually, the intensity of therapy decreases, but it continues for several weeks and sometimes months - the patient’s health must be carefully monitored during this time.
COMPLICATIONS AND CONSEQUENCES OF STROKE
Consequences after a stroke are an integral part of the disease. During an attack, the brain is affected, and the severity of the consequences depends on the size of the lesion. Complications can be either directly caused by the disease or related to the patient’s condition after a stroke.
Main complications of stroke:
- paralysis and sensory impairment;
- difficulty speaking and swallowing;
- deterioration of mental abilities;
- complete or partial memory loss;
- emotional disturbances;
- changes in behavior;
- pain and other unpleasant sensations.
Blood pressure measurement is carried out to make a decision about the need for antihypertensive therapy in a patient with a stroke. BP B3 AFIB is a model with the ability to detect atrial fibrillation during home blood pressure measurement. BP B3 AFIB is clinically validated for many special patient groups and therefore provides accurate blood pressure measurements for everyone. The device is also equipped with MAM technology - the average value of three consecutive measurements is automatically determined.
Basic principles of rehabilitation
The basic principles are the same for all areas of rehabilitation - the earliest possible start of rehabilitation therapy after a stroke, an individual approach taking into account the characteristics of the clinical picture and anamnesis (medical information about the patient), as well as the systematicity and consistency of all therapeutic, medicinal and psychotherapeutic measures.
What does early start of stroke rehabilitation mean?
Activities aimed at restoring lost functions should begin while still in hospital
e, immediately after the patient is transferred from the intensive care unit to the general ward.
You need to understand that a stroke cannot be “cured” in a month
, so it is necessary to adhere to a strict schedule for a long time.
Restoration of motor functions
The main task is the maximum restoration of impaired motor skills. When complete return of motor skills is impossible, the main goal is to develop compensatory skills
. In parallel with the development of compensatory movements, in case of stroke the patient should be adapted to the changing motor pattern, taking into account the remaining neurological deficit and limitation of motor activity.
At the hospital stage, motor rehabilitation of patients after a stroke, as a rule, comes down to performing passive movements in the joints of the affected limbs. Moreover, in case of hemiparesis or hemiplegia (i.e., with a unilateral lesion), the movement in the healthy limb must be performed by the patient himself, otherwise motor skills may be impaired even in unaffected skeletal muscles, which will subsequently have an extremely negative impact on the processes of everyday adaptation.
In patients with severe leg paresis, this stage is preceded by an imitation of walking while lying in bed or sitting in a chair. The patient learns to stand first with the support of an instructor-methodologist, then independently, holding on to the bedside frame or headboard. It is important to try to evenly distribute body weight on the affected and healthy legs. Subsequently, the patient learns to walk: first, walking in place, then around the ward, supported by a bedside frame, then independently, supported by a four- or three-legged cane.
The patient can begin to walk independently without outside support only with good balance and moderate or mild leg paresis. The distance and volume of movement must be gradually increased: walking around the ward (or apartment), then walking along the hospital corridor, up the stairs, going outside and, finally, using transport.
The restoration of self-care and other everyday skills also occurs in stages.
Speech rehabilitation
Impaired speech function after a stroke can take many forms: in some cases, the patient does not understand oral and written speech (sensory aphasia), in others, he perfectly understands the interlocutor, but cannot say anything due to damage to the speech centers (motor aphasia). Any form of speech disorder during a stroke is a factor that causes enormous damage to the emotional state of the sick person. Helping the patient cope with the loss of the ability to communicate with the outside world is one of the priority tasks of relatives and representatives of the patronage service.
Normalization of psycho-emotional background
Psychotherapeutic rehabilitation of patients after a stroke is of great importance. We should not forget that a stroke is a disease that always takes you by surprise and leads to severe psychological maladjustment. Until recently, an active and full of energy person suddenly finds himself in social isolation, without his favorite job, without his usual way of life, without the right to control his life, and sometimes without the ability to independently satisfy basic needs (food, physiological functions, hygiene procedures).
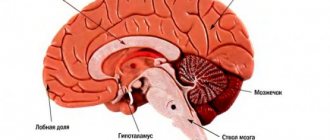
Consequences of ischemic stroke of the right and left side
The consequences of an ischemic stroke will vary depending on the damaged hemisphere. If it is the left one (it is affected much more often), then the right side of the body may be lost. This hemisphere is responsible for logic and speech, hence the other consequences:
- speech is disrupted;
- I have to learn to read and write again;
- loss of speech memory occurs - the patient immediately forgets what he was talking about;
- if help is provided late or incorrectly, he will withdraw into himself and stop communicating.
Restoring memory and speech is difficult in such cases; the patient may not even understand speech. Physical activity is restored much faster.
If the right hemisphere is damaged, then the symptoms clearly appear later, so more time usually passes before seeking help, and the consequences are more serious:
- the patient seems to be completely paralyzed, although this is not the case;
- he forgets what he just did, while he can well remember long-ago events;
- The perception of reality and sense of space are disrupted, depression is observed, and the patient becomes very passive.
Recovery takes a very long time.
Prognosis for patients
With ischemic stroke, complete recovery occurs in only 10–15% of patients. Up to a quarter may return to work. Survival rate is about 50% (one year after stroke). In addition, those who have suffered a stroke are at risk - within 5 years, approximately 55% have a relapse, and the prognosis is even less favorable.
It depends on a number of factors, such as the size of the ischemic lesion and its location, the age of the person and his chronic diseases.
With a hemorrhagic stroke, the prognosis is usually even worse: if a cerebral hemorrhage occurs, in more than 60% of cases it ends in death in the first month. There is a high risk of recurrent cerebral hemorrhage. Of those who managed to survive, about a third become disabled.
In each specific case, the prognosis depends on many factors: the condition of the body as a whole, the location and volume of hematomas, and the promptness of assistance.
With subarachnoid hemorrhage, the prognosis is more favorable, quite often even complete recovery occurs, but the mortality rate is still very high - about 40%.
Types of stroke
All types of stroke occur with an acute decrease or cessation of blood supply to brain tissue. As a result, necrosis (death) of nerve cells is observed, which, as a result of hypoxia, lose the ability to perform their functions. A stroke leads to an acute cessation of innervation of the limbs and internal organs and a decrease in brain activity. The patient may partially or completely lose previously acquired skills, which are then slowly restored as new neural connections are created. Stroke is classified into ischemic and hemorrhagic; subarachnoid hemorrhage in the brain is also distinguished separately. These types differ in their causes, but present with a similar clinical picture.
Ischemic stroke
According to statistics, ischemic strokes take first place and account for up to 80% of all cases. However, they are considered less dangerous and more often occur with a favorable outcome and complete recovery. The cause of ischemic stroke is an acute decrease in blood circulation without compromising the integrity of blood vessels. Depending on the cause, it is customary to classify this pathology into 5 more varieties.
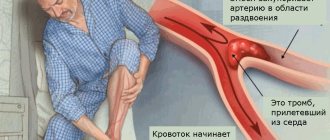
- Atherothrombic stroke is one of the complications of atherosclerosis. In this disease, the vascular walls become less strong and elastic due to deposits of cholesterol and other harmful substances. The formation of atherosclerotic plaques (thrombi) is dangerous due to complete or partial blockage of the vessel, which leads to cerebral ischemia. Symptoms of this type of stroke often begin at night and develop gradually over several hours or days.
- Cardioembolic stroke is a consequence of diseases and heart defects, which are characterized by the formation of wall thrombi. This type is considered life-threatening because it often includes a hemorrhagic component (bleeding in the brain) and occurs with significant damage to brain tissue.
- Hemodynamic stroke is a pathology that develops as a result of circulatory disorders. Its cause can be any disease of the arteries that carry blood to the brain, including atherosclerosis, stenosis (narrowing of the lumen), as well as congenital or acquired anomalies of their structure. Risk factors may include insufficient physical activity, decreased blood pressure, and ischemic myocardial disease.
- Lacunar stroke - develops when blood circulation in small arteries is impaired. The area of the lesions does not exceed 1.5 cm, so the consequences of the attack are minimal. Such strokes are most often located in subcortical structures and do not affect the cerebral cortex.
- Strokes that develop according to the type of hemorheological microocclusion - during such attacks, significant circulatory disorders are not diagnosed. Its causes are various changes in the properties of blood, disorders of its coagulation and fibrin production processes. The neurological picture is weak, but there are additional signs associated with a violation of the composition and properties of the blood.
Ischemic stroke can have varying degrees of severity, depending on its cause and the size of the lesions. More often, the pathology manifests itself in old age, as well as against the background of diseases of the cardiovascular system. Doctors at the Clinical Brain Institute say that most cases of ischemic stroke progress at night, and its manifestations should be a reason to call an ambulance. During the rehabilitation process, repeated circulatory disorders and a relapse of the attack may occur.
Hemorrhagic stroke
Hemorrhagic stroke is diagnosed less frequently - no more than 25% of cases. The mechanism of its development is a violation of the integrity of the cerebral arteries and the development of hemorrhage into the membranes of the brain. As a result, hematomas of different sizes are formed, which put pressure on neurons and can cause their death. This leads to disruption of neural connections and loss of vital functions. If qualified assistance is not provided in a timely manner, there is a high probability of death.
It is often difficult to determine the cause of hemorrhagic stroke. The attack develops abruptly, without increasing symptoms, at any time of the day. In some patients, it is associated with various diseases of the cardiovascular system, if there is a history of them. Detailed diagnostics make it possible to determine the location of the damaged vessel and the size of the hematoma, but doctors will try to determine predisposing factors in order to avoid relapse.
Hemorrhagic strokes are distinguished by the location of the hemorrhage. Modern classification identifies several varieties:
- parenchymal - the place of its localization is brain tissue;
- intraventricular - hematomas are located in the lumen of the ventricles;
- subdural - the fluid is under the hard shell;
- epidural - blood enters the lumen above the hard shell;
- subarachnoid - hematomas between the arachnoid and soft membranes.
It is worth understanding that at least 15% of cases of hemorrhagic stroke occur for no apparent reason, and it cannot be determined even during instrumental diagnostics. Immediate medical attention and stopping bleeding is important - every minute of self-medication increases the likelihood of death. Despite the fact that hemorrhagic strokes occur less frequently, they pose a great danger to the patient’s life, and the presence of hematomas worsens the rehabilitation process after an attack.
Prevention
To never have a stroke, you need to take care of your health. To prevent it you need:
- to refuse from bad habits;
- eat right, in particular, do not eat fatty foods;
- watch your weight and do exercises.
Nothing complicated, but if you systematically follow these recommendations year after year - preferably from a very young age, the risk of not only a stroke, but also the occurrence of many other diseases will significantly decrease. A healthy lifestyle not only significantly prolongs it, but also allows you to stay in good shape for many years.
It is worth emphasizing several important nuances. The fight against excess weight is very important: every kilogram in excess of the norm leads to stress on the heart and blood vessels, and to the development of related diseases. Eating vegetables and fruits will help make blood vessels more elastic and get rid of high blood pressure.
Among physical activities, aerobic training is especially useful: swimming, cycling, running and walking. They will also help you get rid of excess weight. You need to exercise at least half an hour a day, but if your physical condition is advanced, you should first consult a doctor and monitor your blood pressure.
Interestingly, quitting drinking completely is not necessary. Of course, you should not abuse it, but small portions of alcohol can even be useful in preventing stroke, as they prevent the formation of blood clots. The daily portion is 17 ml of pure alcohol - this is, for example, about 150 ml of wine.
But in case of chronic diseases, drinking alcohol even in such moderate quantities should be discussed with your doctor.
STROKE PREVENTION
Stroke Prevention
is a set of measures aimed at preventing it by identifying and correcting possible risk factors for its development.
Primary prevention
includes a system of educational, hygienic and social measures that are implemented among the healthy population and people with risk factors and are aimed at preventing the development of the first stroke.
Primary prevention
involves two main directions:
mass (population) strategy
and
high-risk strategy
.
Population strategy
involves the prevention of stroke in large populations, regardless of a history of stroke or other vascular diseases. It is aimed at creating a healthy lifestyle, proper nutrition, and reducing average blood pressure in a large population of organized people. Such a strategy requires the development and funding of national programs for primary stroke prevention and is the subject of activities by educational bodies and general practitioners.
High Risk Strategy
provides for the identification by medical workers of persons with the highest risk of developing vascular diseases and the implementation of appropriate individual treatment and preventive measures for them.
Recommendations for primary prevention of stroke.
- Lifestyle modification.
- Low-calorie, salt-free diet
(recommended amount of salt no more than 2-3 grams). - Weight loss
for overweight and obese individuals to reduce the risk of stroke. - Smoking cessation for smokers and abstinence for non-smokers is recommended
to reduce the risk of stroke. - Correction of arterial hypertension
. Clinical guidelines for stroke prevention indicate that arterial hypertension is an important, well-studied and correctable risk factor for ischemic and especially hemorrhagic stroke, transient ischemic attack and vascular dementia. Regular blood pressure monitoring is necessary for patients with arterial hypertension.
The use of automatic devices is allowed; the patient or his relatives can measure blood pressure independently using automatic blood pressure meters at home. This method, which has become widespread in recent years, is referred to as the method of self-monitoring of blood pressure (SCAD). Microlife A2 Standard provides convenient and accurate blood pressure measurement at home. The threshold signal allows easy classification of measurement values. A2 Standard stores up to 30 measurement values and is equipped with PAD technology for early detection of cardiac arrhythmias. Additionally, the device comes with a wide range of ML cuffs that fit all common shoulder sizes.
- Diabetes.
It is very important to control your blood glucose levels. You can teach the patient to carry out regular monitoring at home using a glucometer. - Atrial fibrillation.
Effective prevention of stroke in patients with atrial fibrillation is a major challenge.
To ensure timely detection of AF in all patients aged >65 years, periodic screening for the presence of AF using BP A6 PLUS is recommended. AFIB (Atrial Fibrillation Detection) diagnostic function for atrial fibrillation - detects atrial fibrillation. Hypertension and atrial fibrillation are the most common risk factors for heart disease and stroke.
- Clinical examination of persons at high risk of developing CVD.
Secondary prevention of stroke
Should be carried out among patients who have suffered TIAs and strokes.
For targeted implementation of preventive measures, it is necessary to take into account the risk factors in each individual patient (presence of hypertension, AF, diabetes, and others), as well as the results of additional examination.
Based on the examination and clarification of the type of violation, an individual program for the prevention of repeated violations is developed. In most cases, measures begin with non-medicinal ones, and if necessary, medicinal ones are added. The role of drug therapy is just as important for primary prevention, but to a greater extent for secondary prevention, i.e. with a history of previous TIAs and strokes.
Preventing the development of situations that provoke a recurrent stroke
In addition to using effective and surgical methods for secondary prevention of strokes, it is necessary to prevent the development of situations that provoke a recurrent stroke. Such as hypoxia and low blood pressure during surgical operations, a sharp decrease in blood pressure during antihypertensive therapy, taking large doses of sedatives that induce deep sleep, anemia, systemic arterial hypotension, etc. Effective treatment is necessary for concomitant somatic diseases, including diabetes.
In addition, regular courses of vascular, neurotrophic, and metabolic therapy improve the well-being of patients and reduce the risk of exacerbations of cerebrovascular insufficiency. It should be remembered that the choice of vasoactive drugs is made taking into account the examination performed, the state of the cardiovascular system, and cerebral vessels. Most nootropic (improves mental activity), neurotrophic (stimulates recovery processes in the brain) drugs are dose-dependent and their best effectiveness is achieved if the recommended doses and timing of treatment are followed.