Myocardial infarction is a heart emergency that is most often caused by a sudden blockage of a coronary artery by a blood clot. Cardiologists call suspected myocardial infarction acute coronary syndrome (ACS). According to electrocardiography (ECG), ACS with damage to the heart muscle, or the initial phase without death of the heart muscle, which is called unstable angina, is distinguished. Restoring blood circulation in the coronary artery during myocardial infarction within the next 6 hours eliminates the consequences and this approach is very effective because it gives hope for a complete recovery. The first signs of myocardial infarction should be a reason for emergency hospitalization in a specialized center.
Treatment approach at the Innovative Vascular Center
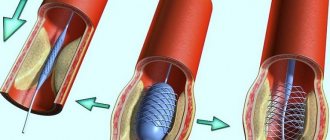
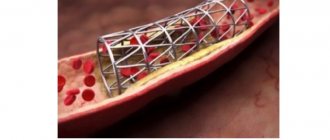
Modern technology for the treatment of ACS and unstable angina involves coronary angiography, angioplasty and stenting of the affected artery. This tactic is successfully used in our clinic. In our clinic there is a clear understanding that saving a life during a heart attack depends on the time when the coronary blood supply was restored. Therefore, receiving ambulances, we organize express diagnostics and prepare the patient for coronary angiography within 5 minutes. The average time to restore coronary blood flow after a patient’s admission to the clinic is less than 20 minutes. Distinctive features, the training of our specialists and the organization of the clinic’s work allow us to maintain a very low mortality rate for myocardial infarction.
USING COOKIES
Our website uses cookies. Below you can find out more about how we work with them and how they can be controlled.
When you visit this website, you consent to the use of cookies in accordance with this cookie notice. If you do not agree to these terms, please disable cookies by following the instructions in this cookie notice to prevent cookies from being stored on your device by this website.
What are cookies?
Cookies are small text files that are sent to your device when you visit a website. The cookies are then returned to the original website on each subsequent visit, or to another website that recognizes the cookies. Cookies act as memory for a website, allowing the website to recognize your device when you visit it. Cookies can also remember your preferences, improve your user experience, and tailor the advertising you see to suit your needs.
You can find more information about downloaded cookies, including how to set cookies on your device, as well as how to manage and delete them, at: www.aboutcookies.org
Types of cookies:
Sessional and permanent
We may use session cookies: these only last until you close your browser. But we also use persistent cookies, which are stored for a longer, specified period of time.
Third Party Cookies
Our website may allow providers to load third party cookies on the services we offer. These files are not under our control. For more information about how a third party provider uses cookies, please visit the website of the relevant third party provider. Detailed information about the third-party cookies running on this website, including their purpose, is provided in the table below.
Cookies used on this website
Below is a brief description of the cookies that work on this website. You should check other AstraZeneca websites as their use of cookies may vary.
Necessary cookies
These files are essential to the basic operation of the website, supporting important functionality such as shopping carts, and the technical operation of the website to ensure its proper functioning.
Website visit cookies
These files allow the website to remember your choices (for example, language or region) and provide other, more comprehensive user adaptation capabilities. Typically, these types of cookies do not collect personal data.
Cookies by service level
These cookies are used to operate the website and include customer surveys, recording visitor numbers and other web analytics. They may also collect limited personal data.
Marketing, anonymous, tracking, cross-site cookies
These cookies are used to track our visitors through our websites. They collect information about how visitors use a website, such as which pages they look at most often and whether they receive web page error messages. These cookies may be used to track individual visitors through our websites: for example, by storing a unique visitor ID so that the visitor can be identified by the websites.
Cookies for marketing, targeted advertising
These files are used to track browsing habits and activities. We use this information to be able to show you targeted/personalized marketing materials. With these types of cookies, we may collect personal data and use it to show targeted content.
How to control and delete cookies
Most web browsers accept cookies, but you can change your browser settings to refuse new cookies, disable existing ones, or simply notify you when new cookies are sent to your device.
To set up your browser and refuse cookies, please read its instructions (usually located in the “Help”, “Tools” or “Edit” menu). More detailed guidance can be found at www.aboutcookies.org
Please note that if you refuse or disable cookies, some functionality of the website may be lost. Additionally, disabling cookies or a category of cookies does not remove cookies from your browser. You will need to do this yourself.
Changes to how our cookies work
Notice of any changes to the operation of cookies for this website will be posted here and, if necessary, identified on our web pages highlighting any changes.
Contact Information
If you have any questions regarding cookies, please contact us at
Causes of myocardial infarction
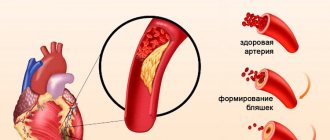
The heart requires its constant supply of oxygen and nutrients, like any muscle in the body. To meet this need, good patency of two large arteries and their branches is necessary, which deliver oxygen-enriched blood to the heart muscle. This is the system of the right and left coronary arteries. If one of these arteries or branches suddenly becomes blocked, part of the heart becomes starved of oxygen. This condition is called "myocardial ischemia." If ischemia continues for a long time, death of the muscle tissue of the heart may occur. This is a heart attack known as myocardial infarction—literally “death of the heart muscle.”
Atherosclerosis of the coronary arteries (coronary artery disease) is the underlying condition for most myocardial infarctions. The immediate cause of myocardial infarction is usually a blood clot that forms in a narrowed area of the vessel and completely blocks the blood flow.
What is the prognosis of a patient with a heart attack and how to influence it
The general prognosis in the post-infarction period is calculated separately for each patient, since additional data from the comorbid background and individual characteristics are taken into account.
Modern methods of diagnosis and emergency care increase survival after a heart attack to 90% during the first year.
To improve the prognosis on their own, patients are recommended to:
- monitoring the course of the disease with regular examinations and additional studies;
- Seeing a doctor if new symptoms appear;
- lifestyle changes;
- systemic medication (for the treatment of hypertension, arrhythmia, prevention of lipid disorders and thrombus formation).
After an MI, lifelong treatment and rehabilitation are required to prevent complications and the development of pathologies in other organs and systems.
Correction of risk factors
The death of a patient in the early or late post-infarction period is largely determined by risk factors for the development of complications or recurrent MI.
In order to prevent and increase life expectancy, it is recommended:
- lifestyle modification: adequate physical activity, giving up bad habits and balanced nutrition;
- weight normalization using non-drug methods. If ineffective, pharmacological agents are prescribed;
- control of blood pressure indicators;
- avoidance of stressful situations;
- systemic intake of prescribed drugs.
Treatment of concomitant pathologies
Injuries, infectious and endocrine diseases aggravate the course of coronary heart disease, so control and adequate treatment of concomitant pathologies affects the prognosis for the patient. Mandatory correction is required:
- diabetes mellitus - glucose level monitoring is carried out in a cardiology hospital to take into account the risk of complications and prescribe treatment;
- myocarditis – inflammation of the muscle mass of the heart worsens the course of the post-infarction period with the development of rhythm disturbances and decreased contractile function;
- kidney disease - impaired excretion of fluid from the body, disorders of hormone synthesis lead to damage to the vascular wall, increased blood pressure;
- pathologies of the thyroid gland (Hashimoto's goiter, diffuse toxic goiter and others).
Traumatic brain injuries with damage to the medulla oblongata (this is where the center for regulating vascular tone and cardiac activity is located) worsens the prognosis for rehabilitation after a heart attack.
Myocardial infarction - classification of causes:
Type 1 – spontaneous, due to a primary coronary event such as rupture, cracking or dissection of an atherosclerotic plaque
Type 2 - a heart attack develops due to a decrease in blood circulation to the heart due to secondary causes, such as coronary artery spasm, coronary embolism, anemia, arrhythmia, hypertension or hypotension.
Type 3 is sudden unexpected cardiac death, including cardiac arrest, often with symptoms of myocardial ischemia. Only a pathologist can answer the question of how and why the development of massive myocardial infarction occurs during sudden death.
Type 4 – associated with coronary angioplasty or stenting:
Type 4a – development of myocardial infarction due to percutaneous coronary intervention.
Type 4b – infarction associated with stent thrombosis.
Type 5 – development of myocardial infarction associated with coronary artery bypass grafting.
Expert advice
I recommend to all my patients who have suffered a major heart attack to reconsider their diet, give up spicy and salty foods, fried and fatty foods. During the rehabilitation period, you need to perform physical exercises, which are shown by a physical therapy specialist. It is also necessary to monitor your weight and stop drinking alcohol and smoking. Hypertensive patients and diabetics who have had a heart attack should be under constant medical supervision and do everything to normalize blood sugar and pressure.
Atypical forms of heart attack
In addition to the compressive pain behind the sternum characteristic of a heart attack, there are several other forms of heart attack that may resemble other diseases or be asymptomatic. These include:
- Gastritis infarction. It begins with pain in the upper abdomen, similar to an exacerbation of gastritis. Often, when palpating the abdomen, pain and tension in the muscles of the anterior abdominal wall are noted. Sometimes the symptoms resemble a perforated ulcer.
- Asthmatic heart attack. The symptoms resemble an attack of bronchial asthma. It manifests itself as an annoying dry cough, a feeling of chest congestion, and shortness of breath. It occurs when the anterior wall of the left ventricle is damaged.
- A painless version of a heart attack, which can manifest itself as a feeling of vague discomfort in the chest, sweating and general weakness.
Signs and photos
Signs of the disease with such a deviation are typical for a heart attack. The patient complains of compression and burning behind the sternum, shortness of breath, rhythm disturbances and pressure surges. But with a large heart attack, I almost always observed pronounced clinical symptoms. And laboratory tests of markers (ALT, AST, troponins, myoglobin and CK) will be significantly higher than with a minor lesion.
In the attached figure you can see an example of damage to a large area of the heart when an artery is blocked by a thrombus in the area of atherosclerotic plaque.
The photo below shows an anatomical section of the myocardium of a patient who died as a result of an extensive transmural infarction. Necrotic changes are clearly visible on it.
Complications
Complications of a heart attack are associated with damage to areas of the heart, conduction tracts, and thrombosis of the cavities of the heart. The development of a heart attack means the death of one or another structural element of the heart.
- Arrhythmias
Approximately 90% of patients experience some form of heart rhythm disturbance (arrhythmia) during or immediately after the event. In 25% of patients, rhythm disturbances appear within the first 24 hours. In this group of patients, the risk of serious arrhythmias, such as ventricular fibrillation, is greatest during the first hour and then gradually decreases. The physician must correctly evaluate these arrhythmias, since some of them can lead to cardiac arrest, so constant ECG monitoring is necessary in patients with myocardial ischemia.
- Damage to the myocardium and heart structure.
Death of heart tissue due to interruption of blood supply can lead to the breakdown of this tissue and damage to the structure of the heart. Most often, there are 3 main mechanical complications of a heart attack:
- Spontaneous rupture of the ventricular wall.
- A rupture of the interventricular septum means that a disturbance of intracardiac blood flow and hemodynamics develops.
- Severance of the papillary muscle is a rupture with the subsequent development of severe mitral valve insufficiency.
- Post-infarction aneurysms of the left ventricle.
A left ventricular aneurysm is a localized area of the myocardium with abnormal protrusion and deformation during systole and diastole, which appears due to the replacement of the myocardium with scar tissue. An aneurysm is dangerous due to the accumulation of thrombotic masses in its lumen, followed by embolism (transfer) through the bloodstream to other organs. With an aneurysm, the volume of the left ventricle increases, which means its relative functional insufficiency manifests itself.
- Thrombotic complications
During a heart attack, a parietal thrombus often occurs in the left ventricle; it develops especially often after heart attacks that occurred in the area of the anterior wall of the left ventricle. The frequency of this complication during a heart attack is 20-60%, which leads to a high risk of a blood clot breaking off and transferring through the bloodstream (embolism). Anticoagulant therapy can significantly reduce the risk of thrombosis and embolism.
Recovery methods
Basic means of rehabilitation after myocardial infarction:
- drug treatment of circulatory disorders;
- Exercise therapy and physiotherapy;
- psychological support and training at a health school for patients with coronary artery disease;
- Spa treatment.
The doctor develops a recovery program after myocardial infarction individually, taking into account the patient’s condition:
- the extent of the lesion (small focal or transmural infarction can be diagnosed);
- localization of ischemic necrosis (apex, septum, wall are affected);
- presence of concomitant diseases.
Definition of clinical group
There are three clinical groups of patients:
- 1 (mild) – the body responds normally to stress, there are no symptoms of heart failure, conduction and rhythm are preserved;
- 2 (moderate) – against the background of arterial hypertension, drug therapy is required, conduction disturbances, heart failure of the 2nd degree, and a permanent form of atrial fibrillation are diagnosed;
- 3 (severe) – a thrombus is present in the heart cavity, ventricular rhythm disturbances are detected at rest and during exercise, the patient is diagnosed with acute aneurysm and heart failure of 3-4 degrees.
Physical rehabilitation
Recovery is impossible without a gradual and systematic expansion of physical activity. Prolonged bed rest increases the risk of developing congestive pneumonia and thromboembolic complications. Lack of physical activity leads to disruption of the gastrointestinal tract and weakening of muscles. This increases the duration of rehabilitation and negatively affects the quality of life.
Taking into account the type of response, a physical therapy program is selected. The intensity of the load is determined individually. They increase gradually with constant monitoring of all indicators.
Psychological rehabilitation
A heart attack is a disease that requires immediate hospitalization. The need for long-term treatment, fear of death, and restriction of activity lead to serious disturbances in a person’s psychological state. This explains the importance of conducting psychological and psychotherapeutic work with the patient.
In addition to the help of professionals, support from loved ones is also required. This allows you to avoid neurosis and depression, which negatively affect health and adaptive capabilities.
Patients often cease to correctly assess their capabilities. There are two extremes: they are afraid of any physical activity or exceed the permissible limits. Here you also have to work with a psychologist.
Drug therapy
Drug therapy during the rehabilitation period is necessary for:
- blood pressure control;
- prevention of angina pectoris, arrhythmia;
- normalization of lipid metabolism and blood clotting;
- treatment of chronic heart failure.
Main groups of drugs:
- antiarrhythmic - used to prevent disturbances in the rhythm, frequency, and sequence of heart contractions;
- antiplatelet agents - used to prevent thrombosis, reduce the risk of strokes and heart attacks;
- beta-blockers – reduce myocardial oxygen demand;
- hypotensive - they are necessary to normalize blood pressure in hypertension;
- nitro drugs – effective for angina pectoris;
- statins – prevent the formation of atherosclerotic plaques and serve as the prevention of atherosclerosis.
Drug therapy is prescribed by a cardiologist. He monitors the patient’s condition and, if necessary, adjusts the treatment program.
Prevention
Rehabilitation after a heart attack will be incomplete if the patient does not eliminate risk factors. Your lifestyle will have to change. Necessary:
- stop smoking - nicotine negatively affects the inner lining of blood vessels (endothelium), increases cholesterol levels (low-density lipoproteins), causes vasospasm, increases blood pressure;
- minimize alcohol consumption (no more than 30 g for men, 20 g for women) or completely abandon it - alcohol increases blood pressure, causes arrhythmia, tachycardia, has a toxic effect, can provoke a heart attack and death;
- give up unhealthy foods, control your weight (body mass index should be between 25-27 kg/m2).
When preparing your diet, it is necessary to reduce the proportion of animal fats - they contain cholesterol. Smoked meats, canned food, and pickles are excluded. Products are steamed, stewed, baked. Frying is excluded. The basis of the menu after a heart attack:
- sea fish;
- lean meats;
- fruits and vegetables;
- nuts;
- whole grain cereals;
- wholemeal bread;
- dairy products;
- beans, lentils;
- olive oil.
Clinical syndromes associated with myocardial damage after infarction
- Pericarditis
Inflammation of the pericardium is observed in approximately 10% of patients after a heart attack with significant myocardial damage. Pericarditis is usually treated with anti-inflammatory drugs, or if there is a large accumulation of fluid, a pericardial puncture may be performed to relieve the patient's condition.
- Post-infarction autoimmune syndrome (Dressler syndrome)
Before the era of thrombolysis and coronary angioplasty, this syndrome occurred in 5% of patients after a heart attack. With the introduction of reperfusion, the development of Dressler's syndrome occurs less frequently. Distinctive clinical signs include fever, chest pain, and symptoms of pericarditis occurring 2–3 weeks after treatment for myocardial infarction. Treatment includes anti-inflammatory drugs and hormones. Clinical manifestations of the syndrome cause significant heart failure that develops after a heart attack.
Features of rehabilitation
Rehabilitation of patients with a large heart attack consists of taking medications, the patient’s participation in programs that allow them to restore their psycho-emotional background, quit smoking, and ensure proper nutrition. How long can such a period last? The duration of active patient management in the clinic after discharge ranges from 5-6 months to one year.
Motor rehabilitation is mandatory; it begins in the first days after an attack and consists of performing breathing exercises with a gradual expansion of motor activity. Restorative measures also include a light massage of the cervical-collar area and the area of the projection of the heart onto the anterior wall of the chest. This should be done very carefully, taking into account the general condition, the presence of complications and concomitant diseases.
With a large heart attack, it will take a long time for the patient to be able to perform normal activities again and tolerate stress normally. If it is necessary to switch to easier working conditions or if the ability to self-care is limited, the patient is assigned a disability.
After conducting research, it turned out that in the post-infarction period, mortality among experiment participants decreased by 25% if they followed the principles of proper nutrition. The use of whole grains in the diet had a particularly beneficial effect.
First aid for heart attack
If acute pain occurs, you must urgently call an ambulance
. In the absence of contraindications, you can take acetylsalicylic acid in a dose of 150-300 mg, after crushing the tablet.
Before the ambulance arrives, the patient must be kept in a reclining position and at rest.
In the room, you need to open the window and unfasten tight clothes and belt.
Doctors call the first hour of the most acute stage of a heart attack “golden”; the outcome of the disease most often depends on this time.
How many heart attacks can a person survive?
The number of myocardial infarctions suffered is an individual indicator for each individual patient. It often depends on the number of lesions in the coronary vessels. With extensive pathology, no more than 2 attacks are experienced, but there are exceptions to the rule. It is more difficult for young patients to cope with the consequences of the disease, but for older people it is a little easier. This is due to the fact that in elderly patients, collateral circulation stabilizes with age - the blood “learns” to bypass the areas of the vessels that are affected by a heart attack.
REHABILITATION AT HOME
Using the recommendations of exercise therapy instructors, patients should regularly do a set of exercises at home. This includes morning exercises and walking. But we must not forget about self-monitoring (measure blood pressure, pulse). For hiking, it will be useful to purchase a pedometer - this way you will know the results of your training, and possibly your achievements. Do not forget about alternating loads and rest.
To quickly say goodbye to the disease, a person needs to forget that he is sick, believe in himself and his speedy and final recovery. Your loved ones should also work on this. A calm, friendly atmosphere should reign in the house. A person must feel necessary, useful, believe in his return to normal life, perhaps to his favorite job.
Some patients who suffered a heart attack belong to the 3rd and 4th functional class
. Their rehabilitation program differs from the program of the first two. Its goal is to provide the patient with such a level of activity that he can care for himself independently. Perhaps - do simple housework or work in an intellectual field (at home).
Physical rehabilitation of this group of patients takes place at home (physical therapy, massage, walks in the yard, slowly climbing a few steps up the stairs). But the patient must be visited periodically by a therapist and a cardiologist.
RECOMMENDATIONS FOR LFK
Classes at the hospital stage must be conducted by a physical therapy instructor. Although the complex for this group of patients is very gentle, the load still depends on the patient’s condition. Severe degrees require complete rest during the first week. With moderately severe patients, the instructor begins classes on the 2nd – 3rd day.
On the 4th – 5th day the patient is allowed to sit for some time on the bed with his legs dangling. From the 7th day you can take your first steps near the bed. After a couple of weeks, the doctor will allow the patient to “walk” around the ward. Go out into the hallway - from the 3rd week. With the help of an instructor, you can try to climb several steps. The number of steps and meters covered is growing every day (up to 500 - 1000 m). The patient is under the supervision of doctors or relatives, because his condition needs to be constantly assessed - by heart rate (heart rate - pulse) and blood pressure level. For reliability, these indicators are checked before the walk (half an hour) and after (half an hour).
If the treatment proceeds without complications, the patient, after an inpatient course, is sent to a cardiological sanatorium somewhere in the suburbs. There is no need for such a patient to travel long distances. There, as part of a 4-week rehabilitation course, he will receive:
- Drug treatment.
- Help from a psychotherapist.
- Diet food.
- Dosed physical activity.