Why is pulse an important parameter in such patients?
To objectively assess the contractile function of the heart, instrumental methods are used, but in everyday life the simplest and most accessible option is pulse analysis in peripheral arteries.
The pulse wave moves from the aorta to the distal parts of the lower extremities, which helps to assess the blood supply to different parts of the body. The pulse is analyzed according to the following indicators:
- frequency;
- rhythm;
- amplitude (strength);
- filling;
- voltage.
Myocardial infarction is accompanied by necrosis (death) of part of the muscle fibers of the heart and replacement with scar connective tissue that is not capable of contraction. A decrease in the working area of the organ leads to changes in pulse rates during myocardial infarction. Their nature determines the degree of compensation and reserve abilities of the heart. By monitoring the heart rate, it is easy to predict the amount of oxygen needs of the body, which must be compared with the capabilities of the muscle.
For this reason, heart rate is one of the key parameters of the cardiovascular system before, during and after a heart attack: this indicator determines the quality and quantity of energy support for the myocardium.
Rehabilitation after a heart attack
Rehabilitation is carried out to restore normal heart function and improve health. The rehabilitation program is developed taking into account the emotional and physical condition of the patient. It involves control over risk factors for a recurrent heart attack, lifestyle modification, and psychological assistance.
Restoring quality of life after a heart attack
This part of the rehabilitation program is aimed at restoring normal levels of functional health. To do this, your doctor may recommend:
- quitting smoking and drinking alcohol;
- following a diet if you need to lose weight or control high blood pressure;
- moderate physical activity. The quantity, intensity and complexity of physical exercises are increased gradually;
- drug therapy: it is possible to continue taking antiplatelet drugs, ACE inhibitors, beta blockers, statins for some time;
- reducing stress levels;
- control of concomitant diseases, prevention of their complications.
In consultation with your doctor, additional treatment programs can be used during rehabilitation after a heart attack. New technologies can be used in recovery after a heart attack, such as stem cell treatment.
Psychological support after a heart attack
A heart attack is life-threatening and can cause severe psychological reactions. If it is normal, the person maintains control over emotions, but may experience fear of a second heart attack or death. He worries about the consequences of a heart attack, may be prone to caution, and the feeling of fear can be quite strong. For rehabilitation in this case, consultations with a cardiologist, psychological support, and gradual restoration of health are sufficient.
With a pathological reaction to a heart attack, an anxious, depressed, depressed, and tense state may develop. It has a bad effect on your well-being: sweating, rapid heartbeat, and insomnia. The reaction may be depressive-hypochondriacal. This means that a person becomes overly suspicious, he is too focused on the state of his health. Hysterical manifestations are possible in behavior after a heart attack: demonstrativeness, egocentrism, constant attempts to attract attention to oneself.
If a pathological reaction develops, the rehabilitation program is supplemented with psychotherapy. It is possible to prescribe sedatives and tranquilizers that will help stabilize the mental state. Without psychological rehabilitation, the condition may worsen: psychosis, severe behavioral disorders, and night wanderings are possible (in older people).
Characteristics and properties of the heartbeat during a heart attack
Qualitative and quantitative indicators of pulse in patients depend on the location and size of the damage. The pulsation of the radial artery changes slightly with focal or subendocardial lesions of the heart muscle. Transmural (“trans” – through, “murus” – wall) infarction is characterized by a significant disturbance of hemodynamics.
The main changes in the properties of blood circulation are realized by a decrease in qualitative (low ejection fraction) and an increase in quantitative indicators.
Low pulse during a heart attack is characterized by:
- small amplitude of the pulse wave;
- slow filling of the artery;
- insufficient tension of the vascular wall.
These changes occur due to a decrease in the contractile force of the myocardium, with the help of which blood is “expelled” from the cavity of the left ventricle. The smaller the affected area, the higher the pulse rate.
Accelerated heartbeat during myocardial infarction (tachycardia) is a compensatory reaction. The mechanism is triggered by a violation of the acid-base balance of the blood: a deficiency of oxygen and nutrients causes dysfunction of metabolic processes, as a result of which under-oxidized metabolites accumulate. Irritation of chemoreceptors in the wall of blood vessels activates the centers of the brain, increasing the rate of breathing, heart rate and blood pressure.
Myocardial infarction
Heart attack
To this day, people sometimes hear, mainly from people of the older generation, something like the following popular cardiological phrases: “This way you can get a heart attack, that is, heart rupture” (usually meaning shock from surprise or, say, from good news).
We bow to our indestructible grandfathers and grandmothers, and may all the news only bring joy to their tired hearts. However, given the exceptional importance of the topic, it is still worth making certainty in the terminology.
A heart attack is not a rupture of the heart. Moreover, we are not even necessarily talking specifically about the heart: no sweeter, say, an infarction of the brain or spinal cord, an infarction of the kidney or intestines.
And the definition that one of the largest search engines on the Internet gives to a heart attack with automatic importunity: “... cessation of blood flow due to spasm of the arteries or their blockage” is also incorrect. A heart attack is not a “cessation of blood flow,” but the result of such a cessation; the result is always pathological and, as a rule, severe.
Therefore, we will strive for accuracy of definitions and clarity of formulations. The topic is really too serious.
Any living tissue, as we know, consists of cells. For normal operation and effective performance of their functions, these cells must breathe, eat and get rid of waste products of metabolism (metabolism). All these processes are ensured by blood flow or, more precisely, by perfusion - constant “impregnation”, through the flow of blood through the tissue, for which the system of capillaries, the smallest blood vessels, is responsible. Arterial blood enters the capillary system, bringing nutrients and oxygen bound by red blood cells to the tissue. Then, through the small, large and main veins, the blood is drained to the lungs, liver, kidneys - for a new cycle of filtration, detoxification, enrichment and gas exchange.
The pumping function, that is, pumping blood under pressure through this complex vascular system, is performed by the heart muscle, or myocardium. The contractile activity of the heart begins in the womb, in the first weeks of pregnancy, and continues non-stop until the last minute of a person’s life. The opposite is also true: the last minute occurs due to the fact that the rhythmic alternation of contractions (systole) and relaxations (diastole) stops.
However, the myocardium, as a hollow pumping muscle (which is anatomically and histologically very complex) consists of living tissues that also need nutrition and oxygen. In this sense, the myocardium is no different from other organs: it itself needs tissue perfusion of blood, continuous and quite intense, given its lifelong work 24/7 without weekends or holidays. The blood supply to the heart is carried out through a special arterial-venous circuit. Due to its external resemblance to the attribute of monarchy, the myocardial circulation is called coronary, or coronary.
Insufficient volume of blood flow through tissue (any tissue, not just the heart) is called hypoperfusion. The widely known term “ischemia” was interpreted differently at different stages of the development of medicine; Today, ischemia is understood as a pathological state of tissue that develops as a result of hypoperfusion, and the obligate (mandatory for the use of the term or diagnosis) signs of ischemia are violations of all the basic processes provided by the tissue blood supply - nutrition, oxygenation (oxygen saturation) and waste removal.
Thus, coronary heart disease (CHD) is chronic starvation and/or “clogging” of myocardial tissue, caused by insufficient functioning of the coronary circulatory circuit. There are many known risk factors and direct causes of the development of ischemic heart disease, as well as its clinical variants, but now something else is more important: this situation inevitably leads to overload, premature wear, degenerative-dystrophic changes in tissues and various malfunctions in the functioning of the heart muscle (for example, attacks angina). In conditions of constant ischemia, the myocardium, brain, kidney and any other organ simply cannot fully perform their functions - just as an athlete who is suffocating and living from hand to mouth will not be able to engage in professional sports.
A heart attack is a simultaneous mass death of cells in a local area of tissue. In other words, this is rapid focal necrosis, occurring as a result of a sharp reduction in blood supply (incomplete ischemia) or a complete cessation of perfusion (total ischemia).
Myocardial infarction is the death of one or more areas of the heart muscle, which occurs due to the fact that coronary blood has stopped circulating in these areas.
A wealth of information is now available regarding myocardial infarction. It is not always, as shown above, reliable and accurate, but in any case it is better than a complete misunderstanding of the normal and pathological processes occurring in one’s own body. We will not dwell on the details of epidemiology here, but we will briefly note the four most significant and alarming points.
Firstly, cardiovascular diseases (primarily ischemic heart disease and heart attacks) stubbornly hold the lead in statistical indicators of non-violent mortality: their share in the overall mortality structure, according to WHO estimates, exceeds 30%.
Secondly, the mortality rate in Russia is two and a half times higher than the European average; three times higher than in the USA; nine times higher than in Japan.
Thirdly, heart attacks are constantly “getting younger”: the average age of primary patients with coronary artery disease and heart attacks is steadily decreasing from year to year.
Fourth, 80% of myocardial infarctions were preventable.
What is submaximal frequency?
Cardiological patients during the rehabilitation period are recommended to perform non-intensive exercises (race walking, jogging), which are characterized by a predominant load on the heart, improving hemodynamic parameters and restoring body functions.
When selecting the intensity of exercises during the rehabilitation process, physical therapy specialists use interrelated indicators of submaximal heart rate and low aerobic power:
- low aerobic power determines the level of load at which less than 50% of oxygen is consumed (compared to the maximum);
- the submaximal pulse characteristic expresses the heart rate at which regulatory systems are strained within the limits of physiological norms, without compensating.
The value of the submaximal contraction frequency in patients depends on the length of time after a heart attack, the condition of the patients, age and gender (the myocardium of young men without pathologies increases strength and endurance at rates of 170 beats per minute; for a 60-year-old woman 3 months after a heart attack, this value is 90 -120 hits).
First aid for heart attack
If symptoms of a heart attack appear, you need to act immediately (video 1):
- call emergency medical assistance;
- Chew and swallow 250 mg of acetylsalicylic acid and take nitroglycerin (spray one dose of spray into the mouth or place one tablet under the tongue). It is better to check with your doctor, therapist or cardiologist in advance whether you can take nitroglycerin (it sharply lowers blood pressure, so it is important to control the dose of the medication);
- provide access to fresh air: open a window or window;
- sit or lie down, take a comfortable position, relax, try not to worry, so as not to increase the load on the heart;
- stay warm (wear warm clothes or cover yourself with a blanket if necessary).
Video 1. How to recognize myocardial infarction and what to do before the ambulance arrives. Boris Todurov. Cardiac surgeon, director of the Heart Institute (Ukraine)
Important! Even if there is doubt that it is a heart attack, emergency medical help should be called immediately. A heart attack can develop very quickly, and you need to act without delay.
If another person has a heart attack, you should:
- call emergency medical assistance;
- check breathing and pulse;
- If a pulse cannot be felt or there is no breathing, perform cardiopulmonary resuscitation.
During cardiopulmonary resuscitation, the airway is checked and cleared, if necessary, artificial respiration is performed and chest compressions are performed.
Important! You can start the heart if it is not beating in a public place (an airport or a shopping mall) using an external defibrillator. Look for a box on the wall with the inscription “AED”, voice instructions will help you attach the electrodes correctly, the device itself will determine the need for defibrillation and allow you to press the button to start the electrical impulse.
How to correct the situation and achieve the desired indicators?
A satisfactory pulse parameter after myocardial infarction is necessary to reduce excessive load on damaged muscle fibers and create conditions for adequate blood supply to organs and tissues. Compensatory reactions of contraction of the muscles of the vascular wall and rapid heartbeat ensure normal functioning with ideal recovery. However, concomitant pathology, irrational therapy, late or inadequate rehabilitation disrupt the process of recovery and adaptation of the heart to work in new conditions.
Based on this, pulse is considered an important indicator of the recovery period. The frequency and strength of blood supply to tissues is corrected using a comprehensive combination of medicinal and non-medicinal methods of therapy.
Taking medications
Heart rate changes in both directions after a heart attack. Tachycardia is a normal physiological reaction of the myocardium during the adaptation period. However, careful monitoring of pulse indicators is necessary, since exceeding the submaximal value develops a repeated ischemic attack.
The following drugs are used to reduce heart rate:
- beta blockers: Bisoprolol, Metoprolol, Carvedilol;
- sodium channel blockers: “Ri;
- cardiac glycosides: Digoxin, Korglykon;
- potassium channel blockers: “Cordarone”, “Sadohexal”;
- sedatives: Novo-Passit, valerian extract.
Bradycardia is a reduced heart rate during a heart attack, which indicates the development of decompensation of the functions of the cardiovascular system. The consequences of this condition are acute or chronic starvation of systems and organs, primarily the myocardium.
For drug correction of bradycardia, use:
- choline receptor blockers: “Atropine”;
- beta-adrenergic agonists: “Isadrin”, “Isoprenaline”;
- stimulants: “Caffeine-sodium benzoate”, “Askofen”, “Citramon” (not prescribed for long-term use);
- herbal remedies: Zelenin drops, hawthorn tincture.
The doctor prescribes medications after examining the patient.
Lifestyle correction
Non-drug methods determine 90% of the effectiveness of post-infarction rehabilitation of patients. Lifestyle modification eliminates rhythm disturbances through a complex effect on neurohumoral regulation.
Patients are recommended:
- Get rid of bad habits - drinking alcohol and smoking. The nicotine contained in cigarettes increases blood pressure, putting additional stress on the heart.
- Reduce excess weight. An increase in the percentage of adipose tissue requires additional blood supply.
- Eat rationally. The diet of cardiac patients contains a large amount of proteins (meat, fish, dairy products), complex carbohydrates (cereals, legumes, potatoes), vitamins and minerals (fresh and dried fruits, vegetables). Limit the consumption of salt, fatty and fried foods. Avoid coffee and strong tea. The normal daily energy requirement for a person is 2500 kcal.
- Physical activity - morning exercises, swimming, jogging increase overall muscle tone and restore heart function faster.
Treatment
Treatment requires hospitalization. Until the condition becomes stable, the person remains in the intensive care unit or intensive care unit. Then he is transferred to the hospital to complete the main stage of therapy. You need to seek medical help and start treatment as quickly as possible. This will improve the prognosis, simplify rehabilitation, and reduce the risk of serious consequences.
Drug treatment
For cardiac infarction, drug treatment is carried out in the following directions:
- anesthesia. For mild pain, analgesics are used. In case of severe pain, in case of pain syndrome, which is accompanied by anxiety, a feeling of fear, sedation and analgesic drugs can be used;
- restoration of blood flow using thrombolytic therapy. It starts immediately and should be carried out within the first 90 minutes after seeking medical help. If pain and changes in the electrocardiogram persist, therapy is continued for 24 hours. Thrombolytic therapy is carried out with caution, taking into account the risk of possible bleeding and other contraindications.
Additionally applicable:
- acetylsalicylic acid. Accelerates the destruction of formed blood clots, improves blood flow;
- heparin. Administered intravenously, it helps restore arterial patency and normalize blood flow;
- beta blockers. Used after completion of thrombolytic therapy and reduce the risk of recurrent myocardial infarction;
- ACE inhibitors. They help normalize blood flow, reduce the load on the heart, and help reduce mortality. They are used taking into account the risk of a possible decrease in blood pressure.
Drug treatment for myocardial infarction is prescribed by a cardiologist, taking into account possible contraindications, health status, and the risk of complications.
Surgical intervention
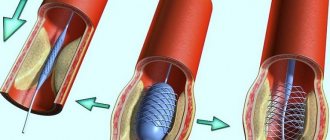
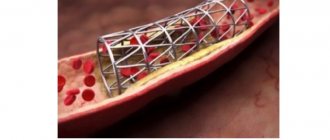
Surgery for myocardial infarction is aimed at increasing coronary blood flow. To do this, two types of operations are used:
- coronary artery bypass surgery. The narrowing of the artery is bypassed by installing a shunt, creating a new “path” for blood flow;
- percutaneous coronary intervention. Interventions that allow you to restore the patency of the coronary artery. To do this, stenting is performed. It involves the installation of a stent, an intravascular prosthesis that helps restore the lumen of the artery in places of its atherosclerotic narrowing.
Alert symptoms and complications
Myocardial infarction in the first months of rehabilitation is accompanied by a pulse with a high frequency and low amplitude, which are caused by the presence of a defect in the muscle tissue of the heart. Heart rate monitoring is carried out to prevent complications.
The pulse rate characterizes the response of the cardiac conduction system to changes in the percentage of oxygen in the tissues. Pathological rapid heartbeat after a heart attack is accompanied by the following clinical symptoms:
- pain in the heart area;
- shortness of breath;
- cyanosis or hyperemia of the skin;
- peripheral edema;
- disturbance of consciousness.
Such conditions are caused by repeated ischemic attack, acute heart failure or other reasons.
Damage to a significant area of the myocardium is accompanied by expansion of the heart cavity and disturbances in the rhythm of contractions. An increase in the volume of organ chambers with hypokinesia is characterized by the development of thrombi (blood clots) in the area of reduced contractile function. Atrial fibrillation contributes to their separation from the walls of the heart and movement along the bloodstream. Stroke is one of the complications that occurs due to blockage of the brain arteries by a blood clot.
Classification
There are several classifications of heart attacks:
- by localization of tissue death. Possible infarction of the left or right ventricle, interventricular septum, apex of the heart, or combined localization;
- by the width of the lesion: extensive (large focal) or small focal. This parameter is assessed by ECG;
- by depth: if all layers of the heart are covered, the infarction is transmural. Subendocardial (affects the inner layer of the lining of the heart walls), subepicardial (affects the outer layer of the lining of the heart walls), intramural infarction (small-focal lesions) can also develop;
- according to the course: monocyclic (the attack develops quickly), protracted, recurrent (a new focus of necrosis develops 3-7 days after the first attack), repeated (a heart attack occurs again within up to 1 month).
When diagnosing, the location of necrosis is assessed (localization, depth and width of the focus of tissue necrosis), as well as the etiology and accompanying circumstances. A heart attack can be spontaneous or caused by ischemia, associated with oxygen deprivation, coronary intervention, or other reasons.
Stages
Symptoms associated with a heart attack may appear in the weeks, days, or hours before a heart attack. Usually this is pain, a burning sensation or squeezing during physical activity, weakness, and mild malaise. Such symptoms appear in the prodromal period preceding the attack. If you consult a doctor at this stage, you can prevent the development of a heart attack (Fig. 2).
Figure 2. Stages of infarction development. Source: Blausen Medical Communications, Inc. / and Journal of the American College of Cardiology
There are four main stages of a heart attack:
- acute. It continues from the development of ischemia until the necrosis of the heart tissue area. The average duration is from 20 minutes to 2 hours. Normal blood flow must be restored as quickly as possible. To do this, you need to remove the blood clot using thrombolytic therapy. If you suspect a heart attack, you should immediately call an ambulance so that doctors can begin such treatment;
- spicy. It begins when tissue necrosis has already occurred. At this stage, enzymatic melting of necrotic tissue occurs, which can last from 2 to 14 days;
- subacute A scar begins to form at the site of necrosis. It takes 4 to 8 weeks to form;
- post-infarction. At this stage, the scar matures and adaptation of the heart occurs.