What happens when the heart is injured
Injury to the heart usually results in tamponade.
In most cases, cardiac injury is fatal, but sometimes the victim can be saved. Most often, the right or left ventricle of the heart is affected, pushing blood into the pulmonary artery for oxygen enrichment or into the aorta for delivery to the organs. When wounded in the back, the atria are more often damaged - the upper chambers of the heart, during the contraction of which blood enters the corresponding ventricles.
When injured, not only the heart muscle itself is damaged, but also the coronary blood vessels. Usually this is the right coronary artery or the anterior interventricular branch of the left coronary artery, lying on the anterior surface of the heart.
The heart is surrounded on all sides by the pericardium, consisting of two layers. Due to the wound, blood accumulates between them. There is a threat of compression of the heart, or its tamponade, as a result of which the contractions of the organ stop. Therefore, even an initially non-fatal wound to the heart can quickly lead to the death of the victim. Blood often accumulates in the pleural cavity surrounding the lungs.
Heart wounds can only be treated surgically. After opening the chest cavity, the wound of the heart muscle and pericardium is sutured, and bleeding from damaged vessels is also stopped. After such an operation, a small scar is formed, which usually does not interfere with the normal functioning of the heart.
Introduction
Despite a well-developed surgical technique for cardiac injuries, the level of postoperative complications remains very high, reaching 57% [2]. The purpose of this study is to systematize complications of wounds of the heart and pericardium using large statistical material,
accumulated in one medical institution, identifying the most significant factors contributing to the development of complications and determining measures to prevent complications.
Material and methods
With wounds of the heart and pericardium at the Research Institute of Emergency Medicine named after. N.V. Sklifosovsky from 1980 to 2010, 936 victims were admitted: with cardiac injuries - 760 (81.2%), with isolated pericardial injuries - 176 (18.8%). The average age of the victims was 35.6±10.6 years. There were 90.7% men, 9.3% women.
The main mechanism of injury was stab wounds with cold weapons (97.8%), gunshot wounds occurred in 2.2% of victims. 23.5% of patients were injured as a result of a suicide attempt, 48.8% were under the influence of alcohol or drugs. Combined wounds of the chest and abdomen were present in 235 (25.1%) patients. 97 (10.4%) patients died during surgery (90 with cardiac injuries, 7 with pericardial injuries). An analysis of complications was carried out in 839 patients who underwent surgery. Statistical processing was carried out to evaluate groups of patients according to the ISS, RTS, TRISS scales, age, volume of blood loss, and time from the moment of injury to surgery. The postoperative period proceeded without complications in 537 wounded, which was 64.0%. The remaining 302 (36.0%) victims had from 1 to 8 complications within a period of 2 to 79 days.
To compare the results of prevention and treatment of complications, two periods were identified: 1980-1995. (267 patients) and 1996-2010. (572 patients). Both groups are comparable in terms of main baseline indicators (Table 1).
In the postoperative period, to assess the condition of the heart and pericardium and timely diagnosis of complications, all victims underwent a dynamic instrumental examination, including electrocardiography, chest radiography and two-dimensional ultrasound (EchoCG and ultrasound of the pleural cavities). In the presence of ultrasound signs of valve and septal defects, ventriculography was performed; in the case of coronary vessel injury and myocardial infarction, coronary angiography was performed.
Results and discussion
Analysis of basic statistical data showed that the likelihood of developing complications was determined by the age of the patients, the amount of blood loss, the severity of the injuries, and the condition of the victim at the time of admission (Table 2).
For convenience of presentation and analysis, we used a classification by organs and systems, separating purulent-septic complications and postoperative bleeding into separate groups (Table 3).
Cardiopericardial complications were most frequently observed.
Myocardial infarction (MI) was diagnosed in 24 (2.9%) patients. The most common cause of its development was certain damage to the coronary vessels (Table 4).
According to the literature, injuries to the coronary arteries (CA) occur in 2.8-8.0% of cases [3, 4]. In case of damage to vessels in the proximal part, restoration of the integrity of the vessel or bypass is considered optimal, while in case of distal damage, one can limit ourselves to suturing and ligation of the vessels [7, 8, 10].
Numerous manuals on the surgery of cardiac wounds describe in detail the technique of suturing wounds of the heart located in close proximity to the coronary vessels, however, in 8 victims who underwent surgery, when multiple sutures were applied to the wound of the heart, the anterior interventricular branch (LAD) of the left was caught in the suture CA, poorly visualized in fatty tissue. Subsequently, 7 of them developed MI, which was the cause of death in 1 case.
In 2 young patients (29 and 36 years old), the development of MI (taking into account coronary angiography data) was associated with stenosis of the LAD as a result of vessel involvement in the scar in the area of suturing the cardiac wound. Unlike MI that developed due to coronary heart disease, with MI due to involvement of the coronary artery in a suture or scar, dilatation and stenting of the vessel are technically impossible. Both patients underwent delayed coronary artery bypass grafting several months after discharge.
It should be emphasized that in 4 elderly wounded patients, MI developed in the absence of damage to the coronary vessels. 3 of them had severe coronary sclerosis, diagnosed in 2 by pathological examination and in 1 by coronary angiography. In one victim, the infarction was actually an area of myocardial contusion due to a gunshot wound.
In 6 victims who suffered an MI, a cardiac aneurysm formed. In total, 2 people died with a cardiac aneurysm, one of them from its rupture. One of these patients underwent surgery: on the 3rd day after suturing the heart wound, he underwent myocardial revascularization by mammary coronary bypass (with the LAD distal to the site of injury), and 8 months later - resection of the aneurysm and plastic surgery of the left ventricular wall. The remaining 3 patients were discharged after stabilization of their condition; their further fate could not be traced.
Trauma to intracardiac structures (IC) when the heart is wounded sharply aggravates the condition of the victims; most of these wounded die at the scene of the incident and on the operating table. These injuries are usually detected during postmortem examination [3], while the frequency of injuries detected in the hospital ranges from 1 to 4% [1, 5]. Perhaps such injuries occur more often, but remain undiagnosed in some surviving patients. Currently, surgical treatment in two stages is considered optimal, with the best results observed after operations performed within 2-3 months after injury [5]. In case of significant hemodynamic disturbances, primary repair is suggested [7].
In our observations, only 2 (0.2%) patients were diagnosed with a ventricular septal defect in the postoperative period; both of them were successfully operated on. In 18 of the deceased, VC injuries were detected only at autopsy, 10 of them died during surgery, the rest within 1 hour to 10 days after surgery.
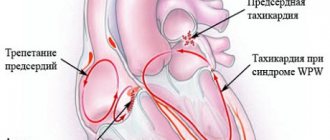
Persistent heart rhythm disturbances were observed in 3 (0.4%) victims. They were caused by damage to the conduction system of the heart due to injury to the high parts of the interventricular septum, injury to the interatrial septum, and injury to the left ventricle posteriorly in the projection of the sinoatrial node.
Foreign bodies of the heart and pericardium were observed in 2 (0.1%) victims admitted in a stable condition after suicide attempts. They were operated on in a delayed manner after additional examination and clarification of the localization of foreign bodies: a sewing needle in one observation, a piece of glass in another.
A rare complication of cardiac injuries is vascular embolism from foreign bodies trapped in the chambers of the heart [9]. We have one such observation: in a 34-year-old patient with a gunshot wound to the left ventricle of the heart, no foreign body was found during thoracotomy, but on the 8th day after the operation an embolism of the right femoral artery occurred with a bullet. An arteriotomy was performed and the foreign body was removed.
The most common postoperative complication is pericarditis, the clinical and instrumental signs of which are Yu.L. Shevchenko, A.D. Kucherenko was noted in 33.3% of the wounded [6]. We observed pericarditis in 146 (17.4%) patients.
The main predisposing factors for the development of pericarditis: exposure for more than 8 hours from the moment of injury to surgery due to late admission or late diagnosis - 10 (6.8%) cases, technical difficulties when suturing a cardiac wound - 6 (4.1%), open cardiac massage - 4 (2.7%), inadequate drainage of the pericardial cavity after pericardiotomy - 49 (33.6%), inadequate drug prevention - 36 (24.7%) cases. In addition, pericarditis developed in 8 wounded patients who, due to postoperative bleeding, underwent rethoracotomy with repeated revision of the heart (5.5%), as well as in 10 victims with thoracoabdominal and abdominal-thoracic wounds with damage to hollow organs (6.8%).
Isolated pericarditis was observed in 72 (49.3%) of the wounded, 74 (50.7%) of the victims had a combination of pericarditis in various combinations with other complications that could play a role in its development. Most often, pericarditis was combined with pneumonia (35), pleurisy (27), and MI (9).
The timing of the onset of pericarditis varied depending on the leading etiological factors and ranged from 1 to 48 days. Early (from 1-3 days) appearance of effusion in the pericardium was observed in the absence of adequate drainage. Primary isolated pericarditis developed by 4-9 days. Later development of pericarditis was associated with other purulent-septic complications.
Serous-fibrinous pericarditis is most often observed after pericardiotomy (112), serous pericarditis was diagnosed in 27 wounded, purulent pericarditis developed in 7 patients in the presence of other severe purulent-septic complications. To prevent pericarditis, we perform thorough sanitation of the pericardial cavity, before suturing the pericardiotomy incision, we form a window on the posterior wall of the pericardium with a diameter of at least 2-2.5 cm, and in the postoperative period for 5-7 days we carry out drug prevention of pericarditis with non-steroidal anti-inflammatory drugs under the cover of gastric blockers secretion with regular ultrasound monitoring. This made it possible to reduce the incidence of postoperative pericarditis from 27.1 to 13.9%.
Treatment of pericarditis consisted of a course of anti-inflammatory therapy with non-steroidal drugs, if ineffective - with corticosteroids, while other complications were also eliminated. Puncture and drainage of the pericardium were performed in 4 cases; in another 1 case, subxiphoid pericardiotomy was performed with subsequent drainage of the pericardium. The indication for drainage in 3 patients was the progression of hydropericardium, and in 2 patients it was the development of purulent pericarditis. One patient experienced progression of the process with the formation of constrictive pericarditis, which required surgical treatment.
Pulmonary-pleural complications
are not specific for cardiac injuries and in a certain percentage of cases are observed after thoracotomy for any penetrating chest wounds.
Postoperative pneumonia developed in 88 (10.5%) patients. In most cases, pneumonia was observed on the side of the thoracotomy, only in 2 cases - on the contralateral side, and in 26 cases it was bilateral. In 82 victims, hypostatic segmental lower lobe pneumonia developed, in 6 deaths - subtotal and total pneumonia in the presence of other complications.
The likelihood of developing this complication was significantly higher in cases of suicidal and auto-aggressive actions (43), in patients who suffered alcoholic delirium (13) and prolonged (over 10 hours) artificial ventilation (16) in the postoperative period, as well as in the presence of combined penetrating chest wounds and abdomen (17). 32 victims had lung wounds; these were superficial wounds of the peripheral parts, which did not affect the development of pneumonia, with the exception of 3 wounded with deep wounds with the formation of intrapulmonary hematoma and hemoaspiration.
Predisposing factors for the development of pneumonia were hypoventilation of lung segments (48 observations), venous congestion (31), segmental and lobar atelectasis (30), intrapulmonary hematomas (3). X-ray signs of pneumonia in most patients (44.4%) appeared on days 4-6 after surgery, in 17.7% on days 1-3, in 14.4% on days 7-9 . In 5 victims, pneumonia was detected at autopsy within 2 to 8 days after surgery.
Prevention of pneumonia was aimed primarily at preventing hypoventilation. Treatment of pneumonia was carried out according to the generally accepted scheme: antibacterial therapy with the use of broad-spectrum antibiotics, mucolytics, inhalations, exercise therapy, and for persistent atelectasis - sanitary fibrobronchoscopy.
Pleurisy was observed in 68 (8.1%) victims. It was manifested by the constant accumulation of aseptic exudate in the pleural cavity for a long time. Predisposing factors for the development of pleurisy were mediastinal hematoma due to parasternal wounds (28), lung injury (25), pneumonia (14), coagulated hemothorax (5), and long-term pneumothorax (5). Treatment of pleurisy in most cases consisted of repeated pleural punctures under ultrasound guidance and a course of therapy with non-steroidal anti-inflammatory drugs.
Purulent-septic complications
were observed in 13.0% of victims.
Pleural empyema was diagnosed in 21 (2.5%) patients, including 6 who died, within 6 to 15 days after surgery. In 7 patients it was localized in the anterior parts of the pleural cavity and was limited, associated with a suppurating thoracotomy wound. The development of pleural empyema was promoted by parasternal localization of wounds with subsequent suppuration (10 observations), massive blood loss (6), injury to hollow organs due to thoracoabdominal wounds (3), rethoracotomy (3), and prolonged pneumothorax (2).
Mediastinitis developed in 4 (0.5%) wounded, 2 of them died. 3 victims had parasternal wounds with damage to the internal thoracic vessels and mediastinal hematoma, another 1 had multiple wounds to the neck, chest, and abdomen with damage to hollow and parenchymal organs.
Treatment of pleural empyema and mediastinitis consisted of drainage of the pleural cavity and mediastinum with TMMK-24 tubes, followed by constant lavage with aspiration, and complex antibacterial and immunocorrective therapy.
Suppuration of the thoracotomy wound occurred in 69 (8.2%) patients. In most cases (40), wound suppuration developed in parasternal wounds, which is explained by damage to the cartilaginous parts of the ribs and the difficulty of hermetically suturing the medial angle of the thoracotomy wound. When the wound is localized in this area with a known infection of the wound channel, additional conditions are created for suppuration, which was observed in 25 patients after suicide attempts and in the presence of multiple chest wounds, regardless of their location.
Rare complications of cardiac injuries are sepsis and osteomyelitis of the ribs and sternum.
Sepsis was diagnosed in 5 (0.6%) victims in the presence of other complications (pneumonia - 5, pericarditis - 4, pleural empyema - 3, wound suppuration - 2, septic thrombophlebitis - 2). Three patients died. The most significant factor in the development of sepsis was blood loss in combination with infection of the chest wall, pleural cavity and pericardial cavity with prolonged exposure from the moment of injury and multiple wounds.
Chronic osteomyelitis of the ribs and sternum developed in 2 (0.2%) patients in the presence of suppuration of the thoracotomy wound and pleural empyema. After sanitation of the wound and pleural cavity, both patients underwent radical surgery 2 months after receiving the injury.
Vascular complications
noted in 8 (1.0%) victims. These were complications associated with thrombosis of large veins (superior vena cava - 2, brachiocephalic vein - 1) and deep veins of the lower extremities (4), in 3 cases there was, in addition, thromboembolism of the branches of the pulmonary artery. In all these observations, the course of the postoperative period was accompanied by the development of severe purulent-septic complications due to massive blood loss. 6 victims died, including a 75-year-old patient, whose cause of death was a rupture of a previously diagnosed abdominal aortic aneurysm.
Abdominal complications
developed in 13 (1.5%) patients, 8 of them with combined wounds of the chest and abdomen. These were adhesive intestinal obstruction (3), acute pancreatitis (2), gastrointestinal bleeding from acute and chronic ulcers (3), peritonitis (2), as well as biliohematoma, intestinal fistula, and volvulus of the small intestine. In one patient with an injury to the interventricular septum, the course of the postoperative period due to hemodynamic disorders was complicated by the development of a non-occlusive disorder of the mesenteric circulation with necrosis of the small and large intestine, leading to death.
Neurological complications
were in 7 (0.8%) wounded: acute cerebrovascular accident due to hemodynamic disorders and coagulopathy - in 5 patients with cerebral atherosclerosis, meningoencephalitis - in 1 patient with simultaneous penetrating injury to the skull, cerebral edema and ischemia - in 1 patient .
Postoperative bleeding
observed in 32 (3.8%) patients. In 18 wounded, the source of bleeding was small vessels of the chest wall as a result of insufficient hemostasis against the background of hypotension and coagulation disorders due to massive blood loss.
In 2 victims, a wound to the aorta was missed, in another 1, a cardiac wound was not found during inspection, in 7 cases bleeding was noted from a sutured myocardial wound due to the cutting of sutures, in another 1 case there was bleeding from a missed second wound due to a through wound of the heart, in 3 cases - from a wound pericardium.
For postoperative bleeding, rethoracotomy was performed in 21 cases; 13 out of 32 patients died. In surviving patients, bleeding after surgery was the cause of the development of complications such as coagulated hemothorax (9), pleurisy (8), and pleural empyema (4).
Thus, the main objective factors contributing to the development of complications after cardiac injuries are the volume of blood loss, the age of the victims, the severity of associated injuries, the patient’s condition at the time of admission, long periods from the moment of injury to surgery, as well as technical errors during surgery. Features of postoperative management and early diagnosis of complications are of great importance. To identify complications, all patients in the postoperative period need to undergo a comprehensive instrumental examination over time. Studying the causes of various types of complications made it possible to develop appropriate preventive measures and reduce the frequency of complications over the past 15 years from 43.8 to 32.3%, and postoperative mortality from 13.8 to 6.8%.
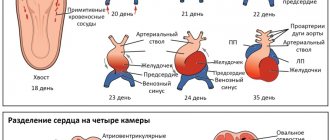
Types of heart injuries
The classification of such injuries depends little on the damaged organ. According to the damaging factor, heart wounds can be non-gunshot or gunshot. If only the pericardium and heart muscle are damaged, such a wound is called non-penetrating. If a traumatic factor (knife, bullet, etc.) violates the integrity of the intracardiac cavities, they speak of a penetrating injury to the heart. It can be blind, when only one hole is formed in the wall of the heart chamber, or through.
The left ventricle is most often damaged (up to half of all cases). In 40%, the right ventricle is affected. Damage to the left and right atrium accounts for 20% and 12%, respectively. Often, when injured, several heart chambers are affected at once. In this case, such injuries are divided into subtypes:
- with damage to intracardiac structures - chordae tendineae, papillary muscles, valves;
- without damaging the internal structures of the heart.
With a penetrating wound to the chest, the heart is damaged only in 5-7% of cases. The proportion of these injuries among gunshot wounds is low - about 1%. Knife injuries predominate, and in 20% of such cases only the pericardial sac, the pericardium, is affected. This condition in itself is non-lethal. However, blood accumulating in the pericardial cavity leads to cardiac tamponade, which is life-threatening.
The sooner a victim with a chest wound is taken to the hospital, the greater the chance he has of surviving the injury. However, only a third of the wounded survive during transport. The rest die before entering the hospital from bleeding and cardiac tamponade. The last complication occurs in 55-70% of the wounded. With gunshot wounds, the victim has very little chance of survival.
Signs of a bruise in the heart area
A strong blow to the chest, leading to a contusion of the heart, leads to the following symptoms:
- Get sick. They do not always occur immediately; sometimes the victim begins to notice painful sensations 2-3 days after the injury;
- Tachycardia;
- Shortness of breath to the point of suffocation. This sign indicates a violation of blood flow in the pulmonary circulation;
- Reduced blood pressure. Hypotension that increases over 5-7 days indicates serious damage to the heart;
- Pallor of the skin. Indicates a drop in blood pressure or a state of shock;
- Heart rhythm disturbances.
When listening with a stethoscope, the doctor can pick up extraneous noises resulting from rupture of internal tissues. Some victims complain of numbness and tingling in the fingertips, uncontrollable anxiety and panic, and pulsation in large vessels. Upon examination, the chest in the area of impact may be swollen, the skin of the injured person may be moist due to profuse sweat.
The clinical picture of cardiac contusion can develop in two ways:
- The angina type of bruise is characterized by short-term pain and lack of air. Recovery occurs quickly, there are practically no long-term consequences of the injury;
- Heart attack-like. The painful attack is long-lasting and pronounced. In addition to pain, shortness of breath, increased body temperature, and agitation of the victim are observed. Without timely treatment, heart failure develops.
Treatment is selected depending on the signs of injury and data obtained during diagnosis.
Diagnostics
A preliminary diagnosis of “heart injury” is usually made by emergency medical services teams.
For the initial diagnosis of heart injury, two signs are important:
- presence of a wound in the left side of the chest or upper left abdomen;
- a progressive decrease in pressure, pronounced pallor of the skin, cold sweat, agitation, which gives way to apathy and loss of consciousness, frequent weak pulse, swollen veins in the neck (signs of internal bleeding and tamponade).
In cases where a heart injury is suspected, but the victim’s condition is stable, additional diagnostic tests can be used - echocardiography, chest x-ray, sometimes pericardial puncture (does not reveal cardiac injury in a third of victims), ECG (changes may be absent).
Spasm of coronary vessels and organ bruise - differences
The clinical picture of the bruise resembles a heart spasm (suddenly occurring coronary insufficiency). Treatment of pathologies is different, so differential diagnosis is necessary. Reliable results are provided by diagnosis, but before it is carried out, a drug test can be carried out - nitroglycerin reduces or completely relieves pain during spasm of the coronary vessels, whereas in case of a bruise, the painful sensations do not go away.
It is also necessary to find out from the patient the entire history of the disease. If in the days preceding the deterioration of health there were blows to the chest, then only a doctor can rule out a bruise.
Treatment of a bruise in the heart area
If a cardiac injury is suspected, victims are hospitalized in a hospital. The main goal of therapy is to restore the functions of the organ. Depending on the identified changes and signs of injury, the following is prescribed:
- Analgesics. These can be both narcotic and non-narcotic analgesics - Morphine, Omnopon, Analgin;
- Antiarrhythmic drugs - Panangin, Trazikor, Isoptin;
- Diuretics, cardiac glycosides, potassium preparations when detecting heart failure;
- Vitamin complexes to strengthen the heart muscle.
In case of complete blockade, cardiac pacing is performed. Surgery is necessary if the bruise is accompanied by damage to the valves.
During the rehabilitation period, it is necessary to follow the doctor’s recommendations:
- Follow a daily routine - get enough sleep, minimize physical activity;
- Stick to a diet - exclude spicy and fried foods, strong tea, coffee;
- Do breathing exercises and physical therapy.
The duration of recovery depends on the nature of the injury and the age of the patient. The consequences of the blow also depend on whether the victim has cardiovascular diseases. In uncomplicated cases, cardiac functions are completely stabilized within 25-30 days. If the bruise is accompanied by serious complications, recovery may take up to 6 months.
Use of traditional methods of treatment
Additionally, you can use traditional methods of treating bruises at home. In the first two to three days, cold compresses are applied; their use reduces pain and helps stop internal bleeding. Compresses are applied for 15-30 minutes up to 6 times a day.
The following means help speed up the resorption of compaction and hematoma:
- Aloe. The agave leaf must be cut and the fleshy side applied to the bruised area.
- Ointment from hop cones. Two hundred grams of interior fat must be melted and mixed with 50 grams of crushed cones. The resulting raw material is filtered and used as an ointment; it must be rubbed into the sore spot two to three times a day.
- Sagebrush. Mash the fresh stems of the plant and apply to the bruise. The bandage is kept for 1-2 hours.
It is advisable to coordinate the use of any folk remedy for closed heart injury with a cardiologist, this is especially necessary for injuries in a child.