How many heart attacks can a person survive?
The number of myocardial infarctions suffered is an individual indicator for each individual patient. It often depends on the number of lesions in the coronary vessels. With extensive pathology, no more than 2 attacks are experienced, but there are exceptions to the rule. It is more difficult for young patients to cope with the consequences of the disease, but for older people it is a little easier. This is due to the fact that in elderly patients, collateral circulation stabilizes with age - the blood “learns” to bypass the areas of the vessels that are affected by a heart attack.
Repeated heart attack: how to avoid illness
As you know, circulatory diseases are now widespread not only in Russia, but also in many developed countries of the world. In our country, these diseases are the leading causes of mortality: they account for more than 54% of all deaths. In 2021, for example, circulatory pathologies claimed the lives of more than 900,000 people (almost half of all deaths in the country). Moreover, not only old people die from these diseases: about 30% of deaths are people of working age. One of the causes of diseases of the circulatory system is exacerbation of coronary heart disease. And one of the most fatal manifestations of cardiac ischemia is acute coronary syndrome. It carries consequences such as unstable angina and acute myocardial infarction. And this will require not only the efforts of doctors, but also the financial costs of the state: for the provision of emergency medical care, for long-term expensive therapy, for rehabilitation. But the human losses associated with the premature mortality of the working-age population are incomparable; they are irreplaceable.
At the present stage of development of medicine, the main role in the treatment of acute coronary syndrome is given to the speedy restoration of coronary blood flow. Percutaneous coronary intervention (PCI) is recognized as one of the modern and most effective methods.
Percutaneous coronary intervention will help, but not for everyone
“The problem of acute coronary syndrome and the high mortality associated with it is truly global,” emphasized the professor of the department of preventive and emergency cardiology of the First Moscow State Medical University. I.M. Sechenova, Doctor of Medical Sciences and chief freelance cardiologist of the Ministry of Health of the Moscow Region Maria GLEZER . “Despite obvious successes in its treatment, the costs of treating such a serious disease place a huge burden on the budgets of many countries around the world due to significant socio-economic damage. This includes the costs of healthcare systems for emergency hospitalization of patients, and for expensive operations, in particular for vascular stenting, and for nursing. Plus economic losses due to long-term disability of patients, their disability and mortality in working age. All this makes us think about how to reduce the risk of developing acute coronary syndrome, as well as the occurrence of recurrent cardiovascular problems.
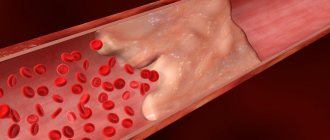
The most dangerous and severe form of acute coronary syndrome is myocardial infarction, in which the death of heart muscle cells occurs due to blockage of a vessel supplying the heart by a blood clot. This can become a life-threatening condition for the patient, causing cardiac arrhythmias, acute heart failure and even death.
Help "MK". In 2021 in Russia, myocardial infarction alone caused the death of more than 60,000 Russians (5 thousand per month!). It is important that patients themselves do not “oversleep” the diagnosis. If characteristic symptoms of a heart attack appear (pain behind the sternum, dizziness, nausea, vomiting, etc.), you should urgently call an ambulance. The time from the patient seeking medical help to arriving at the hospital should be no more than 90 minutes. When the patient is quickly transported to a vascular clinic, the mortality rate from acute infarction is reduced by 60%. If during the first hours the lumen of the vessel is not opened and blood flow is not restored, necrosis of the myocardium will begin. But today, according to statistics, every second death from a heart attack occurs at home, before the doctor arrives.
You should also know: every third heart attack passes without any special symptoms or with mild symptoms. Even an ECG does not always show abnormalities in blood vessels. People with heart disease need to be especially vigilant during the cold season (a 16-year study showed a connection between cold weather and heart attack) and those who have already had a cardiac catastrophe (the risk of a second heart attack is from 10 to 20% in the first year).
“For any symptoms that suggest the development of acute coronary syndrome, it is important to immediately call an ambulance in order to provide first aid to the patient as quickly as possible,” advises the deputy director for scientific work of the Medical Research and Educational Center of Moscow State University. M.V. Lomonosova, MD, Corresponding Member of the RAS, Professor, Member of the Presidium of the Russian Society of Cardiology Simon MATSKEPLISHVILI . — It is very important to quickly transport the patient to the hospital and begin treatment immediately. This is the only way to prevent most of the life-threatening consequences of this condition.
Photo: Alexandra Zinovieva
Stenting, balloon angioplasty, laser angioplasty - what else?
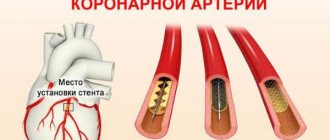
As our experts explained, today the treatment of myocardial infarction in our country, as well as abroad, is carried out mainly using minimally invasive methods. In the acute period, doctors perform coronary angiography, find the problematic artery and widen it with special devices. This procedure is called "percutaneous coronary intervention." It is carried out immediately after the patient enters a medical institution, without waiting for the effect of therapy, or when other methods have already been exhausted. However, in acute myocardial infarction, the risk of complications during coronary angiography increases significantly compared to a planned procedure. But there is no choice: none of the drugs can restore blood flow in the affected artery as quickly and well as can be done with the help of mechanical elimination of this problem - percutaneous coronary intervention.
And this is a whole range of methods designed to reduce stenosis (narrowing) of the coronary arteries: stenting, laser angioplasty and other modern techniques. They all have their own indications and contraindications. Experts briefly described some of them.
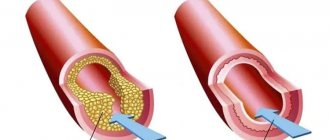
For example, “balloon coronary angioplasty was initially used for individuals with stable angina, later for unstable angina, and for patients in the acute phase of myocardial infarction. The method of expanding the arteries of the heart narrowed by atherosclerotic plaques has long been worked out: a catheter equipped with a balloon is inserted into a vessel on the thigh or arm under local anesthesia, and it is advanced to the site of stenosis (narrowing) of the coronary artery under X-ray control in a specially equipped operating room. At the site of stenosis, the balloon is inflated, and the pressure thus created destroys the plaque and restores the lumen of the vessel.”
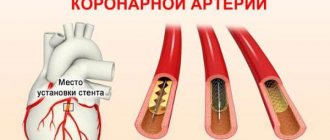
Stenting has also been used for a long time. Allows you to quickly restore blood flow in a thrombosed heart vessel and prevent recurrent coronary circulation disorders. Doctors often combine this method with balloon coronary angioplasty, which reduces the risk of recurrent heart attacks. In recent years, in order to prevent re-narrowing of blood vessels, drug-eluting stents have been used, which helps prevent the increase in atherosclerotic plaque. Stenting can be planned or emergency. It is performed under local anesthesia and under the control of X-ray equipment. After surgery, it is necessary to undergo periodic vascular examinations and take a maintenance dose of aspirin (8 mg/day), as advised by experts.
And also mechanical (surgical) removal of blood clots from affected vessels using special catheters.
But one of the most effective methods for treating complex lesions of the coronary vessels, according to experts, is laser coronary angioplasty. “Laser radiation is delivered to the site of blockage or narrowing of the vessel through a special fiber-optic catheter, and the blood clot is destroyed. The good thing about this method is that it damages the vessel less, and the laser prevents platelets from sticking together.”
Of course, all these methods do not eliminate the very cause of the disease (they do not affect atherosclerosis), but only reduce the pathophysiological effect of atherosclerotic plaques, experts warn. But they can improve the long-term prognosis of the disease, prevent recurrent heart attacks, and attacks occur less frequently. As a result, mortality rates are reduced. This effect is possible only if these life-saving methods are applied to the patient after a vascular accident quickly, by an experienced specialist and if the clinic has the appropriate equipment.
But, alas, such clinics and such specialists are not available everywhere today.
The indifference of our patients knows no bounds
The quality of life of patients after a myocardial infarction largely depends on the patient himself, experts especially emphasize. Yes, today in Russian healthcare many steps have been taken to save the lives of patients with acute coronary syndrome: there are more regional vascular centers; the number of surgical procedures has increased; Innovative drugs have appeared to prevent the formation of blood clots. However, the number of recurrent myocardial infarctions remains high. This means that it also has to do with the behavior of the patients themselves after vascular accidents have occurred.
“The key factor influencing the risk of a recurrent heart attack remains the extent to which the patient strictly follows the doctors’ recommendations,” says the head. Department of Reanimation and Intensive Care, City Clinical Hospital No. 29, Moscow, senior researcher at the cardiology laboratory of the Federal Scientific and Clinical Center for Physical and Chemical Medicine, FMBA, Doctor of Medical Sciences. Alexey ERLIKH . — Often, it may seem to a patient that he is already healthy, nothing hurts him, and there is no point in taking medication for so long (for a year). But practice shows: if a patient stops taking special medications (especially in the first 6 months after a heart attack), his risk of death will increase by 2.7 times! And if patients treated their illness more responsibly, we would not have discussed the problem of high mortality from repeated cardiovascular pathologies in our country for many years.
But the indifference of our patients, even heart patients, knows no bounds.
It was possible to reduce mortality when treating such patients in hospitals, which does not happen in outpatient settings. However, during outpatient treatment, patients and doctors face many insoluble problems. First of all, due to the inaccessibility of effective drugs for such severe patients, even within the framework of preferential treatment. And they must be taken for at least a year, and sometimes longer, which reduces the risk of developing recurrent cardiovascular diseases. Clinics do not have enough specialists and special equipment who are knowledgeable about circulatory problems. This problem is multifactorial and requires attention both from the Ministry of Health of the Russian Federation and from the patients themselves.
Yes, the lifestyle of patients after myocardial infarction, their knowledge of the rules of behavior, and especially adherence to these rules are no less important than competent therapy. No medicine or doctors’ efforts will save you if the person himself, after a vascular accident, continues to smoke, drink alcohol, eat junk food, and do not take medications on time...
Consequences of a heart attack
After a severe heart attack, complications are often recorded. The main consequences of a major heart attack in men and women are as follows:
- heart block;
- pulmonary edema (acute heart failure);
- blood clot formation;
- recurrence of heart attack;
- pericarditis;
- there is a danger of mental disorders;
- disorders of blood circulation in the brain;
- malfunctions of the digestive system;
- heartbreak;
- failure of internal organs;
- Paralysis of the limbs may occur.
How long do they live after a heart attack?
Many people who have suffered a heart attack and their relatives are always interested in how long they live after a major myocardial infarction. Life expectancy depends on the quality and quantity of the consequences of the blow, the size of the lesion of the heart muscle, and the age of the patient. To prolong your life as fully as possible after a heart attack, you need to take prescribed medications, lead a healthy lifestyle, and follow all medical recommendations. According to statistics, about 20% of patients live up to 5 years after a major attack.
Tatyana Raush: “Myocardial infarction is dangerous due to its diversity and suddenness”
Heart and vascular diseases remain the leading cause of death and disability worldwide. According to the World Health Organization, cardiovascular diseases (CVDs) cause nearly 17 million deaths per year. In Russia, over the past ten years, mortality and disability indicators have exceeded the corresponding indicators of economically developed countries by 4-5 or more times and amount to 56 percent of the total number of deaths. In Komi, the prevalence of CVD among the adult population has increased by 17 percent in recent years. How to influence these bleak statistics and what doctors themselves think about this, Tatyana Raush, head of the emergency cardiology department of the cardiology clinic, told Respublika in an interview.
– What is myocardial infarction?
– Myocardial infarction (MI) is a lesion of the heart muscle caused by an acute disruption of its blood supply due to blockage (thrombosis) of one of the arteries of the heart by an atherosclerotic plaque. In this case, the affected part of the muscle dies, that is, its necrosis develops. Cell death begins within 20-40 minutes from the moment blood flow in the vessel stops.
-What happens to the heart?
– The heart is a muscular organ whose main function is to “pump” blood throughout the body. The heart muscle (myocardium) is constantly subjected to very serious stress (on average, at rest, the heart “pumps” five liters of blood per minute, and under intense stress - 15 liters or more). In order to effectively perform such work, the myocardium must be very well supplied with nutrients and oxygen. In the wall of the vessels that supply blood to the heart (coronary arteries), over time, cholesterol-containing thickenings, called atherosclerotic plaques, appear from the inside. Plaques gradually grow and cause a narrowing of the artery (stenosis), which naturally reduces blood flow to the heart. This process is commonly called atherosclerosis. Currently, there are two main reasons for the development of atherosclerosis: a violation of cholesterol metabolism and damage to the inner lining of the vessel, where this cholesterol is deposited. More often this is a gradual process: the heart muscle adapts to it for quite a long time, a person can feel normal for a long time, unaware of what is happening in his blood vessels. But as the process progresses, a person begins to show signs of the disease - paroxysmal pain, which is often localized in the chest, can be burning, squeezing, may be accompanied by a feeling of lack of air, and usually occurs during physical and emotional stress. This is a signal that the heart muscle (myocardium) in the area of vessel narrowing is experiencing a lack of blood supply (ischemia). In this case, it is customary to talk about coronary heart disease. Coronary heart disease can suddenly manifest itself as a heart attack, which is based on the formation of a blood clot - a thrombus. A thrombus forms at the site of damage to an atherosclerotic plaque, to which platelets from the blood flowing through the vessel begin to “stick.” A thrombus causes blockage of a vessel. In this case, blood flow to the corresponding part of the heart suddenly and abruptly stops. If the supply of blood to a section of the heart muscle is stopped for a sufficiently long time, its death develops - a heart attack.
– When should you start sounding the alarm?
– One of the main symptoms of myocardial infarction is chest pain. Intense (sometimes unbearably strong) pressing, squeezing or burning pain behind the sternum is typical. Pain can also be felt on the left of the sternum, rarely on the right. The pain can radiate to the jaw, throat, back under the left shoulder blade or between the shoulder blades, to the upper abdomen. The pain is usually not localized, but widespread. They can occur in waves, sometimes growing, sometimes weakening, stopping and then resuming again. The duration of pain can be from 20 minutes to several hours. There may be accompanying symptoms such as severe weakness, cold sticky sweat, trembling, a feeling of shortness of breath, difficulty breathing, cough, dizziness, fainting. A person may experience emotional agitation, and behavioral disturbances may also occur, including the development of psychosis. Also, a heart attack or pre-infarction condition may be accompanied by nausea, vomiting, and bloating. All of the listed symptoms can occur in various combinations with each other; it is not necessary that all the described signs will be present. There may also be no chest pain (the absence of pain syndrome occurs in 20-30 percent of cases of myocardial infarction). There may be few symptoms, they may not be too pronounced. Myocardial infarction is often asymptomatic in people with diabetes and in elderly patients. Quite often, the symptoms of myocardial infarction are atypical, for example, stabbing pain in the chest. The condition can imitate an exacerbation of osteochondrosis, gastric ulcer, etc. I repeat, if you have sensations that are unfamiliar to you before and it seems to you, for example, that it is radiculitis, which was not there before, call an ambulance. In some patients, acute coronary syndrome occurs against the background of pre-existing stable angina, when the patient is well familiar with the nature of the sensations in the chest that occur during physical activity. Symptoms of acute coronary syndrome may resemble normal human pain, but much more intense, prolonged, and do not stop after taking nitroglycerin. Thus, if you have any sensations in the chest (from mild to strong) or any new symptoms in your health, you should consult a doctor and follow medical recommendations.
– What forms of heart attack exist?
– Sometimes myocardial infarction is disguised as other diseases. The gastrological variant is similar to the picture of an “acute abdomen”: abdominal pain, bloating, and with them weakness, drop in blood pressure, tachycardia. Only an electrocardiogram can clarify. The asthmatic variant occurs without severe pain in the heart, the patient begins to choke, he is given drugs to make breathing easier, which do not make him feel better. The cerebral variant resembles a stroke, confusion of consciousness and speech occurs. A “silent” heart attack occurs completely without pain and most often occurs in patients with diabetes mellitus. Severe fatigue and shortness of breath after physical efforts, which were previously given without difficulty, may be its only signs. Angina pectoris is another mask of a heart attack, under which it “hides” in approximately ten percent of patients. They only experience pain when walking. Often such patients come to the clinic on their own, where an ECG shows a heart attack.
– What are the risk factors characteristic for the development of myocardial infarction?
– Among the risk factors for myocardial infarction, there are those that we cannot influence. For example, a person’s gender, age. Men are more often susceptible to heart attacks; women up to a certain age are protected by their sex hormones. Age – over 65 years old, heredity. Although, it must be admitted, in recent decades, heart attacks have become “younger”; people much younger than 65 years of age are increasingly becoming its victims. The second group of risk factors are those that completely depend on our lifestyle and can be reduced. These are smoking, hypertension, elevated cholesterol and glucose levels, physical inactivity, and excess weight. Knowing your cholesterol level is just as important as your blood pressure. If the numbers exceed the norm, it is necessary to do a detailed blood test for a lipid profile to determine what percentage of total cholesterol is low- and high-density lipoproteins. This will help the doctor select modern medications. Let me emphasize: reducing blood cholesterol levels by just ten percent reduces mortality from heart attack by 15 percent. It must be remembered that elevated blood sugar levels contribute to the formation of atherosclerotic plaques. Regarding weight. To find out if your weight is normal, just determine your waist circumference. In women, it should normally be less than 80 cm, in men - less than 94 cm.
– A heart attack, as is known, is very dangerous in a recurrent form. What brings the risk of another heart attack closer?
– The threat of a recurrent heart attack is increased by four main factors: atherosclerosis, high blood pressure, increased blood clotting and carbohydrate metabolism disorders. These risk factors can only be controlled with the help of properly selected drug therapy. To slow down the further development of atherosclerosis, it is important to prevent the formation of fatty plaques in the vessels. For this purpose, modern drugs are prescribed. You cannot change the dosage of medications at your own discretion. If any problems arise, the doctor will adjust the course of treatment.
– What assistance can those who are nearby provide to the patient before the ambulance arrives?
– If you have the slightest suspicion that a person has symptoms of a heart attack, you should immediately call an ambulance. Before the team arrives, the patient should be kept at rest.
If you have chest pain, take nitroglycerin under the tongue in the form of a tablet or spray (if you are not prone to low blood pressure) and an aspirin tablet if there are no contraindications. If there is no effect, taking nitroglycerin can be repeated, but immediately call an ambulance. An ambulance should be called if this is the first attack of angina pectoris in your life, as well as if the chest pain or its equivalent intensifies or lasts more than five minutes, especially if all this is accompanied by deterioration in breathing, weakness, vomiting, if the chest pain does not stop or intensifies in within five minutes after dissolving the nitroglycerin tablet. The first hours of the disease are critical, not to mention the fact that sudden cardiac death can occur in the first minutes. Thus, the prognosis depends primarily on the speed of medical care provided: the sooner it is provided, the greater the chances of saving the heart muscle, as well as on the success of the measures taken and, accordingly, on how much the heart muscle is damaged, as well as the presence and degree risk factors for cardiovascular disease in a particular person.
– How to behave at home after a myocardial infarction?
– For recovery after a heart attack, the right diet is important: a minimum of fat, nothing fried or spicy, more fiber, dairy products, fruits, vegetables, fish. You will have to give up sausages and sausages, ready-made semi-finished products (dumplings, cutlets, etc.) - they contain a lot of hidden fats that increase cholesterol levels. For the same reason, pates, liver dishes, offal, and caviar are prohibited. Milk fat is also dangerous: you will have to sharply limit butter, fatty cottage cheese, cheese, milk, kefir, sour cream, and cream. When cooking chicken or turkey, all fat and skin must be removed from the carcass. And, of course, a minimum of salt. Vodka, cognac and other strong drinks are canceled. But sometimes you can allow a glass of natural dry red wine. You'll have to change some habits too. If you used to smoke, cigarettes are now completely taboo. An indisputable fact: almost 80 percent of people who have had a heart attack can return to normal life.
– What can you recommend to patients who have had a heart attack?
– To restore the functioning of the heart muscle, it is important to engage in physical therapy. Walking is a great restorative. After just one and a half to two months of training, you can walk at a pace of up to 80 steps per minute without shortness of breath or weakness. And over time, switch to very fast walking - up to 120 steps per minute. Climbing stairs, cycling, and swimming are also useful. Dancing two or three times a week for 30-40 minutes, which will also give a person additional positive emotions. However, make sure that your heart rate during exercise does not exceed more than 70 percent of your threshold.
- How to calculate this?
– From 220 you need to subtract your own age - this is the maximum heart rate. Then we calculate the percentages. For example, for a 60-year-old person, the threshold load is calculated as follows: 220–60 = 160 heart beats per minute, and 70 percent will be 112. This figure should be a guideline. But if unpleasant sensations appear at this frequency, the load needs to be reduced. And most importantly: after a heart attack, lifting heavy objects is strictly contraindicated.
– What means are used to treat myocardial infarction today?
– People who have had a myocardial infarction have a very high risk of having another heart attack, stroke, and death from cardiovascular disease. It is especially important for them to follow all recommendations that will help reduce this risk. Long-term care of patients after hospital discharge is aimed at achieving two main goals. The first is the prevention of the development of recurrent myocardial infarction and death from it (the so-called “secondary prevention”). The second is the correction of complications of myocardial infarction. Secondary prevention includes the maximum possible impact primarily on the risk factors for myocardial infarction, which we have already discussed. As well as drug therapy. In the absence of contraindications, patients after myocardial infarction are prescribed the following groups of medications. These are drugs that thin the blood by preventing platelets (blood cells) from sticking (aggregating) to each other and to the walls of blood vessels. Taking these drugs reduces the likelihood of a thrombus (a blood clot in the lumen of a blood vessel or in the cavity of the heart) forming in the arteries, thereby blocking the main mechanism for the development of myocardial infarction. When treated with these drugs, there is a risk of bleeding, most often gastrointestinal bleeding. Therefore, you should pay attention to the presence of black stools, blood in the stool, or other signs of bleeding. If alarming symptoms occur, you should immediately consult a doctor. Drugs that lower blood cholesterol levels have a direct beneficial effect on arterial walls, “stabilizing” atherosclerotic plaques and preventing their rupture. Because rupture of atherosclerotic plaque is the mechanism that triggers blood clotting and artery blockage, taking these drugs reduces the risk of another heart attack. The doctor selects the dose in such a way as to achieve the target level of cholesterol, and especially low-density lipoprotein cholesterol (LDL), the target numbers are less than 2.6 mmol/L (preferably less than 1.8 mmol/L). The drugs are prescribed for an indefinite period. Only a doctor prescribes medications. In addition, there is a set of mandatory medications after myocardial infarction, which are indicated in the patient’s discharge document after treatment in the hospital, and the duration of their use.
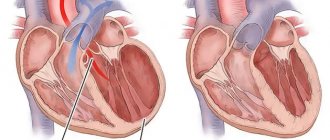
– What are the complications of myocardial infarction?
– Arrhythmia is considered the most serious. It is the most common complication of myocardial infarction. The greatest danger is ventricular tachycardia (a type of arrhythmia in which the ventricles of the heart take on the role of pacemaker) and ventricular fibrillation (chaotic contraction of the walls of the ventricles). In addition to arrhythmia, heart failure (decreased contractility of the heart). It happens quite often with myocardial infarction. The decrease in contractile function occurs in proportion to the size of the infarction. As well as mechanical complications (cardiac aneurysm, rupture of the interventricular septum). They most often develop in the first week of myocardial infarction and are clinically manifested by a sudden deterioration in hemodynamics. The mortality rate in such patients is very high, and only urgent surgery can save their lives. Recurrent (constantly recurring) pain syndrome occurs in approximately one third of patients with myocardial infarction; dissolution of the thrombus does not affect its prevalence. Post-infarction symptom complex. It manifests itself as inflammation of the heart sac, lung sac, or inflammatory changes in the lungs themselves. The occurrence of this syndrome is associated with the formation of antibodies.
– Is it possible for a person who has had a heart attack to use dietary supplements? Or, on the contrary, use them for preventive purposes?
– Biologically active food additives (dietary supplements) are not drugs, although they may have an external resemblance to drugs, for example, they contain some active substances (vitamins, minerals, etc.) that are part of the drugs, and are produced in the same dosage forms ( tablets, capsules, syrups, etc.), but in much smaller doses. In all approved documents, dietary supplements are defined as food products, so they cannot be used for the prevention, diagnosis, or treatment of disease. Remember that not a single dietary supplement has been seriously studied in terms of prevention, much less treatment of patients with myocardial infarction and heart failure. The safety of dietary supplements as food products is regulated by sanitary rules and regulations. Their side effects are often not studied, although they are possible, therefore the instructions for their use may not contain sections “Side effects”, “Contraindications”, “Precautions”. This allows manufacturers of dietary supplements to advertise them as absolutely safe products that can be used without consulting a doctor. Unfortunately, the practice of using dietary supplements around the world does not confirm this. It must be remembered: self-medication is life-threatening; you should consult a doctor for advice on the use of any medications.
– What modern methods of treating acute myocardial infarction exist?
– Treatment of myocardial infarction aims, first of all, to ensure the viability of the heart muscle. This is possible if coronary blood flow is restored in the first hours after the attack. This is the only method of treating myocardial infarction that can save a person’s life. Blood flow through the coronary arteries can be restored only in two ways, which are included in the standards of treatment for myocardial infarction. These are thrombolytic therapy (dissolution of a blood clot with the help of drugs) and surgical treatment: percutaneous transluminal angioplasty, most often with stenting of a coronary vessel, sometimes emergency coronary artery bypass grafting. Thrombolytic therapy with modern medications should ideally be carried out by an ambulance team. Angioplasty and stenting of the coronary arteries are performed in the cardiology clinic on an emergency basis for those patients who promptly sought medical help; For those patients who sought help late, these procedures are carried out delayed or as planned and do not always help save the dead area of the heart muscle.
– What is a stent?
– A stent is a thin metal tube consisting of wire cells, inflated with a special balloon. It is injected into the affected vessel and, expanding, is pressed into the walls of the vessel, increasing its lumen. This improves the blood supply to the heart, quickly relieves pain, limits the size of the infarction, improves contractility in the area of the infarction, reduces the severity of heart failure, reduces the likelihood of developing complications and, as a result, reduces mortality. It should be borne in mind that the earlier treatment for myocardial infarction is started, the higher the effectiveness of treatment and the lower the likelihood of adverse outcomes. It must be remembered that only after a regular high-quality medical examination can you consider yourself healthy or having a disease in a state of stable remission. As well as the fact that early detection of the disease in the initial stages will allow timely and high-quality treatment to be carried out, maintaining efficiency and quality of life. Remember also that only a doctor can diagnose and treat, and the patient must conscientiously follow his instructions and have a firm conviction in the need to maintain a healthy lifestyle.
Stages
An extensive heart attack develops in stages. Doctors identify five stages in the evolution of a dangerous disease:
- Pre-infarction state (prodromal period). This stage lasts from several hours to a month, for each patient individually. The patient has regular angina pectoris.
- The next stage is the most acute. It lasts approximately 30 minutes to 2 hours. A person experiences severe chest pain and breaks out in a cold sweat. In addition to this, the heart rate decreases or increases, and blood pressure decreases.
- The acute period of a heart attack is from 3 to 10 days. During this time, a patch of dying tissue forms in the heart muscle, pain dulls, arrhythmia and high body temperature appear.
- In the area of tissue death, a scar is formed, pain completely disappears, heart rhythm and blood pressure return to normal - all these are symptoms of the subacute stage of the development of a heart attack. The duration of this period is 4-5 weeks.
- The last stage of the disease is called post-infarction, the duration is from 3 months to six months. The characteristic symptoms of this period are an increase in the density of scar tissue and the adaptation of the “engine” to changed working conditions.
“I thought it would go away on its own” Why seven Russians die from heart attacks every hour
The main cause of mortality in Russia is diseases of the cardiovascular system. Every hour, seven people die as a result of a heart attack, and half of all “cardiac” deaths occur due to ischemia. Meanwhile, doctors are confident that most premature deaths can be prevented. And the point here is not at all due to weak promotion of a healthy lifestyle, untimely diagnosis and qualifications of doctors. Lenta.ru looked into how Russians are being killed by their own ignorance.
When 37-year-old father of three children, businessman Igor N., was admitted to the hospital with a myocardial infarction, the prognosis was poor. The young man’s relatives were distressed and kept insisting that the man monitored his health and regularly visited the medical center. The patient's tests showed very high cholesterol levels in the blood. This affects the development of atherosclerosis and the formation of blood clots.
— I asked: have you ever been prescribed medications? — says Maria Glezer, Doctor of Medical Sciences, Professor of the Department of Preventive Emergency Cardiology of the Sechenov First State Medical University, chief freelance cardiologist of the Moscow region. “It turned out that he was indeed prescribed a medicine, and a very good one at that.” He took it for a month or two. Then he stopped. He says: “And I had neither weakness nor drowsiness, which they write about in the instructions. Therefore, I was sure that the drug did not work. I decided not to poison myself in vain.”
Professor Glaser has long ceased to be surprised by the unpredictable behavior of patients. Moreover, the eccentricities of patients do not depend on their age and education. Igor N., as it later turned out, was part of a medical family. His brother ran the genetics center.
“Approximately 40-50 percent of patients with cardiovascular pathologies die at home, before any medical care begins,” Maria Glezer is indignant. — People don’t know the symptoms of attacks. And it happens that they simply underestimate the seriousness and are embarrassed to call an ambulance. Sometimes they will bring in a neglected patient. I ask: “Why did you sit at home for three days?” He replies: “I thought it would go away on its own, resolve itself.”
Photo: Sergey Malgavko / RIA Novosti
If we recalculate the number of deaths from circulatory diseases per 100 thousand inhabitants, in Russia the mortality rate is significantly higher than in most countries. In 2015, the global average was 8.9 deaths. Ours is 13.1. Between Russian regions, the difference in mortality from heart attacks and strokes is also significant - about 30 percent. In Russia, the average mortality rate from ischemia is 72. And in Moscow - 36. In the Central Federal District - 42 people. In the Far East - 60.
The system of organizing medical care and the presence of vascular centers play a huge role. According to the standard, if a patient has symptoms of coronary artery disease and it is possible to get to a specialized institution in 120 minutes, he needs to be taken there. However, patients and their relatives often do not understand why they are being taken to distant lands when they can rest in their local hospital. But, for example, in the Moscow region alone, the launch of vascular centers helped reduce hospital mortality from acute heart attacks by 60 percent.
The statistics are worsened by citizens who were already saved once. The share of repeated heart attacks in Russia is 10-30 percent. Compared to Europe - a lot. Doctors believe that here, too, the main reason is lack of education combined with medical progress. Just 5-10 years ago, most cases of heart attack ended sadly. Now they are treated in such a way that outsiders do not even suspect that the person was on the verge of death. And for the patient, the heart attack proceeds unnoticed: something hurt, they brought him to the hospital, inserted wires into the vessel, five days later he was discharged - and back to work.
“It is important to understand that, even when a heart attack has already occurred, the processes of atherosclerosis and thrombosis in the body do not stop,” says Alexey, senior researcher at the cardiology laboratory of the Federal Scientific and Clinical Center for Physical and Chemical Medicine of the Federal Medical and Biological Agency, head of the intensive care unit No. 29 in Moscow. Ehrlich. — Doctors can slow it down with medications. But almost always medications must be taken for life.
One patient can sometimes be prescribed up to 10 different tablets daily. Citizens are often frightened by such numbers. Having been safely discharged from intensive care, most Russians immediately decide to lead a healthy lifestyle. In the understanding of many, this concept includes giving up all medications. “Because all our troubles come from them.” In addition, people are often sure that they have already recovered from their illness.
“The head is splitting, the person took a painkiller pill - the effect is obvious,” explains Erlich. — The patient does not feel how the medicine affects blood clotting. You don’t feel what happens when you take statins that lower cholesterol. After some time, it begins to seem to him that he is poisoning himself. Some people can also read on the Internet about statins, which destroy the liver. And they get scared. In fact, it has already been proven that these drugs are not dangerous. Everything has side effects. But if we put benefit on one side of the scale and harm on the other, the first will outweigh many times over.
Photo: Igor Zarembo / RIA Novosti
And if for patients who have had a heart attack treated using traditional methods, giving up medications is like a lottery - some are lucky and manage to avoid complications - then for those who have had vascular stenting, statins are necessary.
“If the operated patient does not take these drugs, this almost always means death for him,” adds Professor Maria Glezer. “Therefore, at the stage of inpatient care, when interventions are taking place, an operation is planned, doctors must inform the patient that he will always have to take pills. And if for some reason he refuses, other methods of treatment should be chosen.
The patients themselves hint that their “ignorance” and adherence to a healthy lifestyle are often forced. Cardiac medications are expensive. Not everyone has the opportunity to constantly buy them.
“My father suffered a heart attack and had a stent placed,” says Olga Mikhailova from Nizhny Novgorod. - Already discharged. They prescribed a lot of drugs. One of them costs about 6,000 rubles per month, to drink for a year. The father is a widower and does not work. Pension - 7,000 rubles. I am a single mother, I earn pennies. Medicines are not given for free. And the choice is cannibalistic. Either the father’s diet should be reduced, or his son should be put on a diet.
Sometimes, in order to optimize drug costs, people do not even go to their clinics, but ask pharmacists directly at pharmacies to select generics (copies of original drugs - note by Lenta.ru
). Often they actually turn out to be cheaper. But whether they help is a big question.
“Sometimes there are such pills that it’s scary to take them in your hands,” Maria Glezer shakes her head. — Released in some village of Dyatkovo by some unknown company. And how to treat such people, how to take responsibility?
Simon Matskeplishvili
, Doctor of Medical Sciences, Corresponding Member of the Russian Academy of Sciences, Deputy Director for Scientific Work of the Medical Research and Educational Center of Lomonosov Moscow State University, member of the Presidium of the Russian Cardiological Society:
One of the global problems facing the country is demographic. We are trying to solve it by increasing the birth rate, maternal capital, emigration, and so on, but the most important direction is to save the lives of those who already live in Russia.
The majority of the population (52 percent) in our country dies from diseases of the cardiovascular system, more than a million people a year. The disadvantages are that these are serious diseases. Pros: They are preventable. This also applies to healthy people, but more so to those who have already suffered similar events.
If we look at the initiatives being carried out by the Ministry of Health, they are, in principle, positive, and our successes are colossal. This is the construction of modern vascular centers, new approaches to the treatment of such cardiovascular pathologies as acute coronary syndrome, acute cerebrovascular accident (stroke). This is the proliferation of new pharmacological agents and all types of medical devices. All this is good, but the principle of continuity of treatment is no less important.
Photo: Vitaly Nevar / TASS
So a patient came to this vascular center, where he underwent an excellent procedure. We performed primary coronary intervention, placed a stent and eliminated the cause of acute coronary syndrome, or treated some patients conservatively, depending on what was needed, and gave the patient prescriptions. These appointments are designed to preserve everything that we were able to save, designed to ensure that the patient does not have the same episode again. According to the law of medicine, if it happened once, then it can happen a second, third, and fourth time. If a patient is lucky enough to survive the first time, they will not necessarily survive again.
But patients today are not the same as they were 20-30 years ago, they come already knowing everything about their diagnosis, tell us how we should treat them, know in advance what complications they will have, side effects from the drugs we give them we appoint, and begin to choose. “I don’t want to take this drug, I want this one.” Plus, advertising of dietary supplements is everywhere, but we do not have the right to advertise the drug. Therefore, patients either do not comply with the prescribed treatment or change it based on their own considerations. Plus, the drugs are also different. There are original and non-original. This question is more about price, although there is a difference in quality. And our patients can buy a new phone every month and stand in line for two months to receive a free drug. This is the reality of our life.
And another problem is that not only patients, but also doctors today are also different. Patients are annoying people who interfere with the doctor’s work with documents. Doctors stopped talking to patients, stopped explaining to patients what was done to them, why and how to avoid problems in the future. We do not explain why we give medications that thin the blood, lower cholesterol, or why we prescribe any other medications. “Here’s your assignment—go.”
Factors provoking myocardial infarction
Myocardial infarction
There are various reasons for the development of the pathological condition:
- Diabetes. The formation and increase in atherosclerotic plaques occurs more intensely in people suffering from diabetes. This disease is characterized by vascular fragility and metabolic disorders. Atherosclerotic plaques and blood clots more often occur on vulnerable vessel walls.
- Hypertonic disease. High blood pressure causes the walls of blood vessels to thicken. They become dense and lose elasticity. During exercise, altered blood vessels cannot meet the heart's increased need for oxygen.
- Heredity. The tendency to develop hypertension, atherosclerosis and thrombosis can be inherited.
- Floor. Heart attacks occur 4 times more often in men than in women.
- Age. Young people are less likely to develop atherosclerosis and extensive myocardial infarction.
- Tobacco smoking. After inhaling tobacco smoke, a sharp narrowing of blood vessels occurs.
- Lack of movement. In people who lead a sedentary lifestyle, the walls of blood vessels lose their elasticity.
- Obesity. Excess weight creates additional stress on the cardiovascular system
- Alcohol abuse. Alcohol causes dysfunction of the liver, which is responsible for breaking down fats. As a result, fat accumulates in the blood and is deposited on the walls of blood vessels.
- Kidney disorders. In renal failure, the exchange of phosphorus and calcium is disrupted. As a result, calcium is deposited on the walls of blood vessels and thrombosis develops. Many of those suffering from kidney disease have experienced a massive heart attack.
- Stress. Severe psycho-emotional shock or frequently occurring stressful situations can cause a critical narrowing of the lumen of blood vessels.
- Hyperlipidemia. Abnormally elevated levels of lipids and lipoproteins in the blood are a provoking factor for the development of extensive myocardial infarction.
- Excessive physical activity. High myocardial oxygen demand, insufficient elasticity of blood vessels and their spasms can lead to the development of a heart attack during intense sports.
- Trauma or surgery. Pathological narrowing of the lumen of the coronary vessels can occur as a result of injury or surgery.
Harmful work or why heart attacks become younger and hearts become decrepit
Even in children 10-15 years old, doctors have recently observed signs and prerequisites for the development of atherosclerosis, the consequence of which is myocardial infarction. They are found to have fibrous cholesterol plaques. A heart attack no longer just makes you look younger. It is becoming a very tangible threat even to the youngest inhabitants of the planet. At the same time, in young people, atherosclerosis takes on more aggressive forms than in older people. “Healthy Heart” week is a week when a complete examination of the cardiovascular system can be carried out at the Medservice clinic at the most attractive prices.
Cardiovascular disease is often called the epidemic of the 21st century. They spare no one. Neither athletes at the peak of their careers, nor stars, nor so-called ordinary people. Vladimir Turchinsky died at the age of 46 - Dynamite. A heart attack claimed the life of Roman Trachtenberg, an optimistic radio joke teller, when he was just 38 years old. At the same age, the Russian actor, the best Huck Finn of all time, Vladislava Galkina, died of acute cardiovascular failure. Antonio Banderos suffered a heart attack while playing sports. At one time, Julia Roberts also had this problem.
The statistics are inexorable
40% of Russians die from cardiovascular diseases. Every year in Russia, 50,000 cases of myocardial infarction are registered. Every day - 136 cases! Every hour, 5-6 people go to medical institutions with myocardial infarction.
30% of patients in our country die from acute myocardial infarction. At the same time, the number of cases in people aged 25-29 has tripled. Among those aged 30-40, this figure has doubled. The risk of recurrent heart attack is as high in younger patients as in older patients.
5-10% of the total number of heart attack survivors are men under 39 years of age. But the risk is highest in men over 45 years of age and women over 50 years of age.
Even athletes have myocardial infarction at a young age. The number of deaths among this group of patients has recently increased by more than one and a half times.
Stress is everything to us
Most often, they say that myocardial infarction is a consequence of poor lifestyle and stress. The medical literature provides the following factors that predict early heart attack:
- heredity;
- some diseases, including hypertension, diabetes;
- viral diseases transmitted on the legs;
- bad habits, including smoking, alcohol, drugs, especially cocaine;
- poor nutrition;
- overweight;
- low physical activity;
- stress and (attention!) harmful work.
In the reality we have created, stress is a constant companion of a person. We often associate stress with obvious manifestations - anger, rage, irritation... If only it were that simple. Often we don't notice it at all.
We are stuck in a traffic jam or parking, and a “deer” blocks our view nearby. It seems like a normal situation, it doesn’t even annoy us, but it’s stressful for the body. We fly by plane in two hours the distance that our ancestors covered on foot in a month. An obvious advantage, but stress for the body. For our body, even the fact that we have food in the refrigerator and it is easy to get from there is stressful. This is stress because the body “thought” that it had to hunt or gather pasture for hours to kill the worm.
That is, stress is not only nerves and pent-up negative emotions. This is our way of life, including, at first glance, such advantages as availability of resources, mobility, information wealth.
Not junk food at all. AdviсeRegularly include sea fish in your diet, which not only contains complete protein, but is also rich in omega-3 polyunsaturated fatty acids. Every day, consume vegetables in amounts from 100 to 400 grams (except potatoes) and fruits in amounts from 100 to 250 grams. Limit your consumption of table salt. The daily intake for an adult should not exceed 5 grams. Avoid fast foods, canned food, salty cheeses, and sausages. | Smoking is bad. Got it?Smokers have a four to five times higher risk of heart attack than nonsmokers. If a smoker has high blood cholesterol and high blood pressure, the risk of developing a heart attack increases eight times, and cerebral stroke is four to eight times more likely than among non-smokers and former smokers. When you quit smoking, your cardiovascular risk is significantly reduced after just two weeks, and after three to five years, the risk of death from cardiovascular disease does not exceed the risk of a person who has never smoked |
As for harmful work, this is a special topic.
“Heart dangerous” are professions in which there is low physical activity, the need to make decisions, high personal responsibility and responsibility for people, daily and rotational work schedules, night shifts, prolonged stay in an upright position, emotional stress and concentration. We have created a world where everyone works in this mode. Any modern work activity becomes dangerous for the heart. Managers, officials, shift workers, salespeople, service workers, businessmen, teachers, drivers - all these are potential patients with a bunch of cardiovascular diseases and more. These also include representatives of creative professions who are in a state of permanent stress - to have time to do everything, to defeat everyone, to please everyone.
The consequences of stress and harmful work are aggravated by the lack of physical activity, proper nutrition and regular sex. Where do we go after work? That's right - stuck in a traffic jam with “deer” for three hours. And at home - a sofa, food rich in animal fats, smoking and alcohol.
What to do?
Eat less, worry less, at least in cases where we can control our consciousness, move more, give up bad habits and have regular sex. In fact, this is a universal, albeit banal, recipe.
Quite often, the root cause of mortality from cardiovascular diseases is heredity and congenital defects that were not detected in time. They may remain in “sleep” mode. But they can deliver a mean blow if a person suddenly decides to become an athlete, goes to the gym and, picking up the first dumbbells he comes across, dies. It happens. But it happens the other way around - a person still becomes an athlete and dies, either in competitions or in training. Because his congenital heart defects were not detected in time, even during medical examinations to which athletes are regularly subjected. This is called "underdiagnosis." This happens even among athletes who are always under the supervision of a doctor.
Therefore, regular examination of the body should become another excellent habit. A medical examination at work is a “piece of paper” for the employer so that he is not fined by supervisory authorities. If you are interested in living a healthy life, regularly undergo a complete body examination.
The question is often asked: at what age is it necessary to undergo a complete examination of the body? There are risk groups, including age groups. But congenital heart defects and a rare heart rhythm, in some cases, can be detected in a person in utero. Thus, the prevention of cardiovascular diseases must begin even before birth! Although this already depends on the parents.
How to protect yourself from a heart attack
| “In Russia, the state has managed to seriously reduce mortality from acute forms of coronary artery disease—myocardial infarction. A wise decision was made and a network of Regional Cardiology Centers was created. There they provide emergency care to patients who have suffered a heart attack - primary percutaneous coronary intervention and vascular stenting. This helps prevent necrosis of cardiac tissue, sudden cardiac death and patient disability. As for the prevention of heart attacks, everything is in the hands of the person himself, his personal attitude towards his health. The statistics are that after 30, a heart attack becomes a real risk for everyone! Therefore, you need to regularly contact specialists and undergo diagnostics. The minimum diagnostic complex includes an ECG, ultrasound of the coronary vessels, and Holter monitoring. and ultrasound examination such as LVAF. Together they make it possible to determine a person’s heart rate, myocardial condition and capacity. Therefore, the Medservice clinic implements unified cardiological complexes, which our specialists can perform on-site with a 50% discount.” | Elena Vladimirovna Guseva, cardiologist-arrhythmologist, head of department, candidate of medical sciences |
Diagnosis of heart attack
Ultrasound examination of the heart
Extensive myocardial infarction is diagnosed based on the following points:
- Patient complaints
- ECG study in dynamics
- Ultrasound examination of the heart
- Laboratory detection of elevated levels of myocardial enzymes, monitoring them over time
- Coronary angiography according to indications
- Myocardial infarction in diabetes mellitus
Life after a heart attack
A heart attack is one of the most serious heart pathologies. In the world, more than 2 million people have suffered myocardial infarction to date. And although this is a very dangerous condition, practice shows that if a patient lives a month after a heart attack, then the subsequent probability that he will live at least a year, and with the right lifestyle - much longer, is about 80%. Most people who survive a month after a heart attack live 10, 20 or more years. And although there is a risk of a second heart attack, by following the recommendations of doctors, it can be minimized.
The favorable prognosis depends on the person’s age, the cause of the heart attack, the presence or absence of concomitant pathology (arterial hypertension, obesity, diabetes mellitus, atherosclerosis, etc.). From the timeliness and completeness of medical care during a heart attack. And first of all, it depends on the person’s lifestyle after a heart attack, his attentiveness to the signals of his body and the recommendations of doctors.
What determines life expectancy after a heart attack?
The favorable prognosis depends on the person’s age, the cause of the heart attack, the presence or absence of concomitant pathology (arterial hypertension, obesity, diabetes mellitus, atherosclerosis, etc.). From the timeliness and completeness of medical care during a heart attack. And first of all, it depends on the person’s lifestyle after a heart attack, his attentiveness to the signals of his body and the recommendations of doctors.
When should you see a cardiologist to prevent a heart attack?
It is worth thinking about the possibility of heart failure if a combination of the following symptoms occurs: snoring, shortness of breath, apnea, bleeding gums, swelling of the legs and face, arrhythmia, frequent headaches and pain in the left shoulder, frequent urination at night. Well, the so-called “pre-infarction state” occurs during exacerbation of coronary heart disease. This usually happens over the age of 50. If you are over 50, you should take a blood test at least twice a year for preventive purposes and monitor your cholesterol levels. A sign of an approaching heart attack is pain in the sternum after exercise. Such pain is relieved with vasodilator drugs. But self-medication is deadly. The doctor will prescribe treatment and prevent a heart attack.
What measures should the rehabilitation period include ?
After the patient is discharged from the hospital, he needs rehabilitation measures, which should be carried out at home. This is, first of all, proper nutrition (table No. 10). It is important to completely avoid alcohol, coffee, rich broths and soups using them, mayonnaise, egg yolks, fatty meats, sausages, pancakes, baked goods, offal, canned food, smoked foods, pickles and sweets. You should eat fractionally - in small portions 5-6 times a day. Acceptable methods of cooking are stewing, boiling, baking, steaming. Be sure to include fruits and vegetables containing potassium and magnesium in your diet. And it is very important to reduce your salt and liquid intake. You should absolutely not be nervous, you should completely eliminate stress and heavy physical activity, and stop smoking. Hiking in the fresh air and sanatorium treatment are recommended. The patient should be regularly examined by a cardiologist. Physical therapy and the use of cardiac herbs (celandine, sage, meadowsweet and other herbs) are indicated. But it is very important that folk remedies are approved by your doctor.
How long does the rehabilitation period last after a heart attack?
Anatomical changes after a heart attack usually occur in the first 6 months. This is the rehabilitation period. If you neglect the doctor’s recommendations during this period, serious consequences are possible. Even if a person feels well, he should not consider himself “perfectly healthy.” It is important to relieve the heart as much as possible. So, after a heart attack, the heart rate should be kept with the help of appropriate medications and exercises within the range of 55-60 beats per minute, that is, less than the physiological norm for a healthy person. This reduces the load on the heart.
In general, during these six months it is very important to take care and be sure to do exercises that help the heart work (physical therapy). And it will be better if the patient performs these exercises under the guidance of a physical therapy instructor in the clinic. You should definitely undergo all prescribed examinations and take all tests on time to prevent another heart attack. Based on the results of these examinations, a person may be given disability due to a myocardial infarction (diagnosis - “post-infarction cardiosclerosis”).
CVD - diseases of the circulatory system
IHD - coronary heart disease
MI - myocardial infarction
ACS - acute coronary syndrome
CVD - cardiovascular diseases
Cardiovascular diseases (CVD) are a leading problem in healthcare and society as a whole, since 50% of all deaths in the Russian Federation occur as a result of these diseases. In recent decades, economically developed countries have seen a steady decline in mortality from circulatory system diseases (CVDs) [1–5]. In our country, there has been a positive trend towards a decrease in mortality from CSD since 2004 [6], however, this figure remains 2-3 times higher than in economically developed countries. The leading cause of death from CSD is coronary heart disease (CHD), which in 2011 accounted for 52.8% in the structure of mortality from CSD [7]. Mortality from IHD in Russia is 3 times higher than in the USA [8], and higher than in Japan – 9 times [9]. A major contribution to mortality from coronary artery disease is made by mortality from myocardial infarction (MI).
The purpose of this analysis was to study the dynamics of morbidity and mortality from MI for the period from 2000 to 2011 in the Russian Federation.
Materials and methods
To analyze the incidence and mortality from MI among the urban and rural population, we used official statistics from Rosstat and the Russian Ministry of Health for the period from 2000 to 2011 [7, 10]. Mortality from myocardial infarction was assessed according to sex and age. The number of cases of myocardial infarction and death from it was analyzed in absolute values and per 100 thousand population (coefficients). Data on a number of indicators for CVD and IHD are also presented. Coding of causes of morbidity and mortality was carried out according to the International Classification of Diseases, 10th revision.
In current statistical forms, MI is divided into acute and recurrent. In this article, the term “acute” is replaced by the term “primary”, which seems more appropriate, since recurrent MI also goes through an acute stage.
results
In the Russian Federation, the total number of patients (over 18 years of age) suffering from CSD in 2000 was about 19.5 million; Since 2003, there has been a significant increase in the number of these patients, which by 2011 reached 31.8 million. This trend was accompanied by an increase in the number of patients with a newly diagnosed CSD from 2.2 million in 2000 to 3.5 million in 2011 d. The total number of patients with IHD during this period also increased from 5.4 million in 2000 to 7.4 million in 2011. A particularly noticeable increase in the incidence of IHD was observed in 2004 (Fig. 1).
Figure 1. Number of patients (18 years and older) with coronary artery disease, including those newly diagnosed, in the Russian Federation in 2000–2011. The increase in incidence rather indicates an improvement in the diagnosis of coronary artery disease, since this indicator in our country is determined mainly by the population’s seeking medical care.
When assessing the incidence of MI, it was found that the number of patients with this pathology over the past decade remained practically stable and only in 2004 was there a slight increase in this indicator. This applies to both cases of primary and recurrent MI. Primary MI predominated and was recorded in 87% of cases, and repeated MI in 12.5-13% of cases. The ratio of the number of cases of primary and recurrent MI among all registered cases of MI also remained relatively stable (Fig. 2).
Figure 2. Number of patients with primary and recurrent myocardial infarction in the Russian Federation in 2000–2011. In 2011, there was a decrease in the proportion of primary MI to 83.8% and an increase in the proportion of repeated MI to 16.2% in the total number of MI cases.
It is noteworthy that in the structure of the incidence of coronary heart disease, the share of myocardial infarction accounted for only from 2.5 to 3.2%, and in the structure of mortality - from 10.1 to 11.6%. It should be noted that over the course of 9 years, the proportion of registered patients with myocardial infarction among the number of patients with coronary artery disease decreased, while the proportion of those who died from myocardial infarction in the structure of the number of deaths from coronary artery disease increased annually (Table 1).
Mortality from MI (primary and recurrent) increased by 3.8% from 2000 to 2011. At the same time, the number of deaths from primary MI decreased by 5.3%, while the number of deaths from repeated MI increased by 33.7% (Table 2).
A greater number of deaths from primary MI occur due to its predominance over recurrent MI.
During the analyzed period, no significant positive dynamics in mortality from primary myocardial infarction was noted, with the exception of 2011, when a decrease in this indicator by 4.9% was recorded compared to the level of 2010.
Due to the fact that over the past 2 years there are no mortality rates by sex and age in official statistics, we analyzed mortality from MI in men and women using absolute indicators. At the same time, an increase in the number of deaths since 2004-2005 was revealed. by 2011 for women by 9.7%, and for men by 1.3% (Fig. 3).
Figure 3. Number of deaths of men and women from myocardial infarction in the Russian Federation in 2003–2011.
The analysis of mortality from MI (absolute indicators) in men and women showed that the mortality rate of men of working age is higher than that of women. In 2003, the number of men who died exceeded the number of women who died from primary MI by 7.5 times, in 2011 by 8.3 times, from repeated MI by 12 and 17.4 times, respectively. At retirement age, the number of women who died exceeded the number of men who died from primary MI by 1.3 times in 2003, and by 1.4 times in 2011. The number of men who died from repeated MI exceeded the number of women who died in 2003 by 1.2 times, and in 2011 by 1.1 times (Table 3).
An analysis of the characteristics of mortality from MI (coefficients) depending on gender also showed a high mortality rate for men of working age, the level of which exceeded the mortality rate of women from primary MI by 8.1 times, and from repeated MI by 13.7 times (Table 4).
When analyzing mortality from MI in different age groups, an increase in this indicator in men from 35-39 years old by 2.7 times, in women from 45-49 years old by 2.7 times (2003) compared with the previous age group and its progressive increase in subsequent age groups in both men and women. In 2009, a similar trend was observed (Table 5).
The excess of mortality in men over the same indicator in women was determined to a greater extent at working age, and at retirement age it was much less pronounced. The increase in mortality among women in older age groups in 2009 compared to 2003 is noteworthy.
Mortality from MI among urban and rural residents varied significantly: among the urban population it was 1.6 times higher than among the rural population (2009).
Analyzing hospital mortality from MI, it should be noted that this figure from 2000 to 2011 was 15-16%. Among all patients who died from MI since 2003, almost 60% died in the hospital (Table 6),
of these, in the first 24 hours after admission to the hospital, 40.4%, of which 33% were under 65 years of age.
Discussion
In the first decade of the 21st century (2000-2011) in the Russian Federation, according to official statistics, there is no significant dynamics in the incidence of myocardial infarction and the mortality rate from it increases by 3.8%.
When analyzing the morbidity and mortality from MI in the structure of IHD, it becomes obvious that such a small percentage, which MI occupies in the structure of morbidity (about 3) and mortality (about 11) from IHD, apparently does not reflect the real situation in our country. The small share of mortality from MI in the structure of mortality from IHD with a relatively stable number of cases of the disease and low variability in the incidence of MI may indicate that statistics operate with insufficiently verified data, poor diagnosis of MI outside medical organizations and, apparently, doctors’ errors in coding morbidity and mortality from MI and IHD in our country. When comparing the incidence of CHD and MI in the Russian Federation with other countries, it turned out that in the USA the incidence rates of CHD are significantly lower than in our country. Moreover, about 50% of all cases of IHD are MI [8], while in Russia, among all cases of IHD, angina pectoris is diagnosed in 43.5% of cases, other forms of IHD are diagnosed in 54.2%, and MI accounts for only 3 % [10]. According to these data, it can be assumed that in our country, MI is diagnosed and registered much less frequently. In addition, if in the USA about 32.7% of deaths from IHD are caused by MI [11], then in the Russian Federation this figure reaches only 10.6% [12]. According to official statistics, chronic forms of IHD predominate among the population of the Russian Federation; high mortality from IHD exceeds that in the USA by 3 times, and this situation raises the question of the causes of death of patients with IHD [11-13]. Thus, official statistics on morbidity and mortality from coronary artery disease and myocardial infarction, apparently, do not fully correspond to the real situation.
Mortality from MI significantly predominates in men, especially in working age. In recent years, there has been an increase in the number of deaths from MI among women in older age groups. This may be due to the longer life expectancy of women, the more severe course of MI and the peculiarities of treatment tactics (women undergo fewer revascularization procedures).
From 2000 to 2011, there was a 33.7% increase in mortality from recurrent myocardial infarction, while other countries, such as Sweden, recorded a decrease in the number of recurrent myocardial infarctions [14]. This may indicate poor secondary prevention of MI and a lack of continuity in the provision of medical care to patients who have suffered an MI.
In addition, the high hospital mortality rate from MI is noteworthy. According to official statistics, hospital mortality from MI (15-16%) is comparable to that in a number of Russian studies. Thus, according to the results of the RECORD Register, hospital mortality was 13.2% [15], according to a study conducted at the Lyubertsy hospital in the Moscow region - 15.2% [16]. According to the Moscow Department of Health, mortality from MI in Moscow hospitals in 2006 was 15.4% (the range of this indicator is from 3.1 to 24.4%). Thus, the hospital mortality rate in the Russian Federation, according to official statistics, appears to reflect the real situation and is consistent with the results of other studies. In economically developed countries of the world, mortality from MI is significantly lower. In the EHS registry, mortality in acute coronary syndrome (ACS) with ST segment elevation was 7.5% [17], in the GRACE registry - 8% [18], and in the CRUSADE registry - 6% [19]. The problem of high hospital mortality on the 1st day after admission to the hospital (40.4%) deserves special attention. This necessitates an additional analysis of its causes, among which are the late admission of patients to medical organizations, the severity of the patients’ condition and, apparently, the provision of specialized medical care is not at the proper level (lack of thrombolytic therapy, resuscitation, etc.). Understanding the causes of high hospital mortality, especially on the 1st day, will make it possible to develop measures to reduce it. Created in the USSR in the 60-70s of the last century on the initiative and under the leadership of academician. E.I. The Chaz system of providing medical care to patients with MI, recognized throughout the world, has significantly reduced hospital mortality from MI, which was less than 10%, which is comparable to the same figure in foreign countries [20].
To reduce the incidence and high mortality from myocardial infarction in our country, it seems advisable to implement a number of measures, including increasing the effectiveness of primary prevention, including specialized health care in clinics and cardiology clinics, increasing the efficiency of the formal dispensary observation of patients with coronary artery disease that exists to date, in primarily those who have had an MI. Thus, in 2007, the coverage of dispensary observation of patients with MI was 10% for primary and 10.2% for repeated MI, and in 2011 - 14.5 and 11.7%, respectively. Currently, the Ministry of Health of the Russian Federation is preparing a procedure for dispensary observation, including for patients with CVD, developed by specialists of the Russian Cardiology Research and Production Complex.
Since 2008, within the framework of the National Project “Health” under the leadership of the Ministry of Health and Social Development of the Russian Federation, a system of medical care for patients with acute vascular diseases (MI, stroke) began to be organized in the country. This “vascular program,” which includes a transportation system, the widespread use of thrombolytic therapy, including in the prehospital stage, the use of high-tech treatment methods and modern drug therapy in patients with ACS, is currently actively developing. Regional vascular centers are being created and are functioning, in which emergency X-ray endovascular interventions are already performed in patients with ACS. Thus, according to the monitoring of regional vascular centers carried out by the Russian Ministry of Health, the number of x-ray endovascular interventions performed in patients with ACS in 2009 was 19,814, and in 2011 this figure increased 2.8 times and amounted to 55,227, while hospital leave mortality for 2009-2011 amounted to 5.5%. At the same time, in vascular centers there are problems such as a lack of qualified personnel, insufficient financial support, etc. Analysis of mortality rates from CSD indicates a greater rate of decline in this indicator in the regions participating in the “vascular program”. So, for 2010-2011. in the regions participating in the “vascular program”, mortality from CVD decreased by 11.4%, while in other regions of the Russian Federation - by 2.9%, which indicates the contribution of the implementation of the “vascular program” to reducing mortality from CVD in our country.
For a more complete and objective assessment of morbidity and mortality from MI and the quality of treatment of patients with this disease in the Russian Federation, it seems appropriate to conduct epidemiological studies, as well as a comparative analysis of the results of monitoring of regional vascular centers, data from the Federal Register of ACS [21] and the results of audits of vascular centers, conducted by specialists of the Russian Cardiology Research and Production Complex. This analysis is currently underway.
Conclusion
According to official statistics, in the first decade of the 21st century in the Russian Federation there has been a small share of mortality from MI in the structure of mortality from IHD, with a relatively stable number of MI cases and low variability in the incidence of MI.
Mortality from MI significantly predominates in men, especially those of working age. In recent years, there has been an increase in the number of deaths from MI in women in older age groups.
Over the years of observation, an increase in mortality from recurrent MI has been recorded (from 2000 to 2011 by 33.7%).
There remains a high hospital mortality rate from myocardial infarction, which for the analyzed period of time is 15-16%, with a high mortality rate on the 1st day after admission to the hospital (40.4%).
How does a second heart attack manifest itself and its consequences?
How does a second heart attack manifest itself and the consequences it can cause? This question worries perhaps a considerable number of elderly people. How it manifests itself, what causes it, and how to avoid such an unpleasant phenomenon as a second myocardial infarction, the consequences of which will be very disastrous, even fatal.
The consequences of a second heart attack can begin as early as 2 months from the previous one. Recurrence of myocardial infarction is most often observed in elderly men with arterial hypertension during the first year after thrombolysis or after myocardial infarction without a Q wave. It is severe, and asthmatic variants and arrhythmia can often be detected. There may also be frequent development of acute heart failure and chronic heart failure, or its worsening if it already exists.
Clinically, recurrent and repeated myocardial infarction is manifested by a pain syndrome that is less expressive, and this is due to a decrease in pain sensitivity of the previously affected area of the myocardium. Acute left ventricular failure can also dominate due to the growth of the necrosis zone.
Second myocardial infarction - consequences and complications
Recurrent myocardial infarction is difficult to diagnose. Myocardial infarction, the consequences do not exclude the consequences of a second heart attack and its manifestation. They always negatively affect the condition of the whole organism. It all depends on how extensive the myocardial damage was. Patients who have had a myocardial infarction may experience heart rhythm disturbances. Due to the fact that a section of the myocardium dies, heart failure may develop.
As a result of an extensive heart attack and the formation of a sufficiently large scar, a cardiac aneurysm may occur, this is a life-threatening condition for the patient. An aneurysm requires surgical treatment. It not only worsens the functioning of the heart, but also significantly increases the likelihood of blood clots forming in it, and the risk of its rupture is quite high.
A second myocardial infarction can have extremely serious consequences. It appears most often in older people. In some people who suffered a heart attack, the pain syndrome was either mild or completely absent. This is explained by an increase in the threshold of pain sensitivity as a result of cerebral sclerosis and changes in the receptor cardiac apparatus. Recurrent infarction may also take the form of cardiac asthma or an episode of acute arrhythmia. The consequences of a second myocardial infarction may vary. After this, circulatory failure often develops. Diagnosis of recurrent myocardial infarction is also difficult because the ECG already shows post-infarction changes.
It should also be understood that the mortality rate with repeated myocardial infarction is much higher than with its first manifestation. Also, the risk of death increases significantly with shorter interinfarction periods.