Make an appointment by phone: +7 (343) 355-56-57
+7
- About the disease
- Cost of services
- Sign up
- About the disease
- Prices
- Sign up
Sinus arrhythmia (SA)
is an fluctuation in the rhythm of heart contractions emanating from the sinus node.
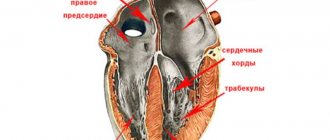
There is a conduction system in the human heart. It consists of nerve fibers, works on the principle of electrical wiring, and is responsible for ensuring that electrical impulses arise in the heart and are carried out to all its departments. This system is a kind of “battery”, since it is self-regulating and autonomous. In this self-regulating system there is an oscillation of the “current”. In humans, like in any living creature, fluctuations in the frequency and rhythm of heart contractions are possible.
The human heart is alive. It is impossible to artificially “set” its rhythm forever; this is not a household appliance, not a car.
The initiator of heart contraction is the sinus node. If “current fluctuations” occur at its level, then SA develops. It is not life-threatening, is usually secondary and goes away on its own.
Sinus arrhythmia can occur in anyone. During physical activity, emotions, both positive and negative, during sleep. But these deviations in heart rate are so short-term and insignificant that they are sometimes detected only during daily monitoring of the electrocardiogram; they do not require treatment, since they go away on their own, without symptoms.
What it is
Let's try to figure out what sinus arrhythmia is in a child, why it occurs, how to recognize it, how and when to treat it.
Doctors classify this type of change in heart rate as a nomotopic disorder of automaticity. The sinoatrial node in this pathology, as well as normally, remains the primary pacemaker, but the formation of the impulse in it is changed. In the medical literature, the term “sinus arrhythmia” (SA) is sometimes considered synonymous with respiratory arrhythmia, when the heart rate increases during inhalation and decreases during exhalation.
The clinical and electrographic classification proposed by M.S. Kushakovsky and N.B. Zhuravleva in 1981 identifies the following disorders of sinus node automatism:
- tachycardia - increased contractions;
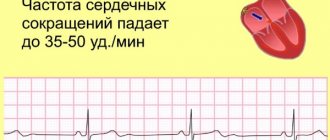
- bradycardia – the heart, on the contrary, works slower than normal;
- arrhythmia – abnormal, irregular rhythm;
- rigid sinus rhythm - the number of beats is the same, regardless of physical activity and emotional stress, time of day, state of sleep or wakefulness;
- sinus node failure;
- weakness of the sinus node.
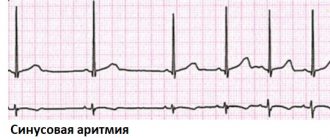
On an electrocardiogram, each complex begins with a P wave and corresponds to one heartbeat. Sinus arrhythmia on ECG film is reflected by different distances between these teeth. That is, the duration of the intervals from one blow to the next one is not the same. In this case, the total number of heart contractions per minute can be equal to the age norm, in contrast to tachycardia and bradycardia.
Age-specific heart rate values
A child's heart works harder than an adult's. To clarify the diagnosis of arrhythmia, it is important for the pediatrician to know the normal heart rate in children.
Domestic and foreign scientists have proven in clinical studies that gender and age values for the number of pulse beats are universal. That is, the heart rate is not affected by:
- race;
- nationality;
- with proportional development of the child - height and weight;
- Country of Residence.
The Center for Syncope and Cardiac Arrhythmias in Children and Adolescents of the Federal Medical-Biological Agency of Russia, based on expert assessment, has developed indicators that it recommends that pediatricians focus on.
The number of heart beats in one minute.
| Age child | Newborn | 1 - 2 years | 5 – 7 years | 12 – 15 years | 16 - 18 years old | Adults |
| Severe tachycardia | more than 160 | more than 175 | more than 130 | more than 110 | more than 110 | more than 110 |
| Moderate tachycardia | 141 — 159 | 141 — 174 | 106 — 129 | 91 — 109 | 81 — 109 | 81 — 109 |
| Normal indicators | 120 -140 | 110-140 | 80 — 105 | 70 — 90 | 65 — 80 | 60 — 80 |
| Moderate bradycardia | 111 -119 | 86 — 139 | 71 — 79 | 51 — 69 | 51 — 69 | 46 — 59 |
| Severe bradycardia | less than 110 | less than 85 | less than 70 | less than 50 | less than 50 | less than 45 |
During physical activity or anxiety, the pulse accelerates, and during sleep it becomes slower. Until the age of eight, boys and girls' hearts contract at the same rate. As they grow older, the main “pump” of the body in the fair half of humanity begins to work somewhat faster – by about 5 beats per minute.
Pathogenesis
Due to the high activity of the autonomic nervous system during inspiration, the atria become filled with blood, the so-called Bainbridge reflex occurs. It consists of an increase in heart rate in response to an increase in central venous pressure (the sympathetic part of the nervous system is activated).
As you exhale, the tone of the vagus nerves increases, which leads to a decrease in the number of heart beats (parasympathetic fibers of the vagus are turned on). Some authors explain the development of sinus arrhythmia as a compensatory mechanism for improving gas exchange, which reduces the load on the myocardium.
Etiology
Sinus arrhythmia occurs in healthy people and is considered normal if it is not accompanied by clinical manifestations. A child may experience this after overeating or during sleep; as a consequence of physical overexertion - in athletes after training.
Pathological reasons:
- Cardiac – trophic disorders and inflammation affecting the pacemaker (myocardial dystrophy, congenital heart anomalies, myocarditis of various etiologies, circulatory failure).
- Extracardiac – bronchopulmonary and endocrine pathologies, negative effects of certain medications, micronutrient deficiency.
- Combined – if cardiac causes are combined with other factors.
I propose to discuss the causes of arrhythmia in adolescents. Child endocrinologists figuratively call metamorphoses of the body during puberty a “hormonal explosion,” and psychologists and neurologists working with teenagers note the lability of their nervous system.
In this age period, arrhythmia is detected most often:
- It is in adolescents that autonomic dysfunctions are usually diagnosed, accompanied by disruption of the interaction of the sympathetic and parasympathetic nervous systems;
- we must not forget about coronary disease, which, unfortunately, has become “younger” over the past decades;
- wanting to appear older, a teenager is easily influenced by his peers, he may secretly try alcoholic drinks or drugs, or pick up a cigarette;
- young people tend to neglect sleep and rest, and sit for long hours at the computer.
Even if your child has no complaints, try to find time to have a confidential conversation about committing to a healthy lifestyle. As surprising as it may sound, taking care of our body is ingrained in us in childhood and is “inherited” from our parents.
Heart rhythm disturbances in children
Posthypoxic complications of the cardiovascular system (CVS) in newborns range from 40 to 70% and represent an urgent problem in pediatric cardiology. In terms of frequency of occurrence, posthypoxic maladaptation states of the cardiovascular system are in second place after organic heart pathology in the neonatal period.
As a result of hypoxia in the fetus and newborn, the autonomic regulation of the heart and coronary circulation is disrupted, which can subsequently lead to the formation of persistent vegetative-visceral disorders, one of the manifestations of which is “posthypoxic syndrome of disadaptation of the cardiovascular system.”
What it is? This is a functional disorder of the cardiovascular system in a newborn and young child, which is associated with chronic antenatal (unfavorable course of pregnancy: long-term gestosis, threat of miscarriage, anemia during pregnancy, exacerbation of chronic diseases) and intranatal hypoxia (weakness of labor, premature birth, labor stimulation, cesarean section, umbilical cord entanglement). The clinical symptoms of this pathology are polymorphic, appear from the first days of life and are often disguised as other diseases. Therefore, the doctor has to carry out differential diagnosis with congenital heart defects, congenital carditis, and cardiomyopathies.
One of the common clinical variants of this syndrome in newborns is cardiac arrhythmia, most often in the form of supraventricular and ventricular extrasystole, rarely supraventricular paroxysmal tachycardia. These changes can occur even in the prenatal period and the first hours after birth.
The severity of the condition is usually due to hypoxic-traumatic damage to the central nervous system in the form of hyperexcitability syndrome, hypertensive-hydrocephalic and convulsive syndromes, impaired innervation of the heart, the condition of the myocardium (heart muscle) and hormonal status.
Extrasystole is a heartbeat that is premature in relation to the main rhythm. Depending on the location of the ectopic focus, atrial, atrioventricular and ventricular extrasystoles are distinguished. Depending on the location of the ectopic focus, atrial, atrioventricular and ventricular extrasystoles are distinguished. The problem of extrasystole attracts the attention of cardiologists due to its high prevalence and the possibility of sudden death. Ventricular extrasystole is considered the most unfavorable prognostically.
Are extrasystoles dangerous? Most arrhythmias in childhood are benign, reversible and do not pose a threat to the child’s life. In newborns and young children, they can lead to the development of arrhythmogenic cardiomyopathy or heart failure, contributing to early disability and even death. Ventricular extrasystole has an adverse effect on hemodynamics, causes a decrease in cardiac output and blood supply to the heart muscle, and as a result can lead to ventricular fibrillation and is associated with a risk of sudden death.
How do heart rhythm disturbances manifest? In approximately 40% of cases, rhythm disturbances in children are asymptomatic and are detected by chance (on an ECG), or during an objective examination during medical examination or after suffering viral or infectious diseases. Arrhythmias are manifested by palpitations, a feeling of interruptions in the work of the heart, and its freezing. In addition, the child may experience weakness, dizziness, fainting, shortness of breath, and periodically pale skin.
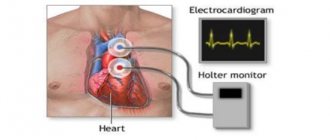
Examination plan for children with cardiac arrhythmias: 1. Assessment of clinical, anamnestic and genealogical data. 2. ECG examination (it is necessary to record a long ECG tape, since often NDCs are of an unstable nature and they do not have time to appear on a short tape). 3. Daily ECG monitoring. 4. Holter monitoring (HM) - long-term recording of an ECG (a day or more) on a special recorder, followed by decoding on a special analytical system. The method is available for any age, incl. and for newborn children. Today, the method is leading in the examination of children with disabilities. The uniqueness of the method is that ECG registration is carried out without restricting the patient’s free activity. The method has no contraindications. 3. Holter monitoring (HM) - long-term recording of an ECG (a day or more) on a special recorder, followed by decoding on a special analytical system. The method is available for any age, incl. and for newborn children. Today, the method is leading in the examination of children with disabilities. The uniqueness of the method is that ECG registration is carried out without restricting the patient’s free activity. The method has no contraindications. 3. Holter monitoring (HM) - long-term recording of an ECG (a day or more) on a special recorder, followed by decoding on a special analytical system. The method is available for any age, incl. and for newborn children. Today, the method is leading in the examination of children with disabilities. The uniqueness of the method is that ECG registration is carried out without restricting the patient’s free activity. The method has no contraindications. Ultrasound examination of the heart, or ECHO-cardiography (Echo-CG) 5. Consultation with a neurologist with NSG (neurosonography) and EEG (electroencephalography) of sleep 6. Consultation with an endocrinologist with an ultrasound of the thyroid gland and determination of hormonal status.
Principles of drug therapy for cardiac arrhythmias in children. Treatment of heart rhythm disturbances, especially life-threatening ones, is carried out strictly individually depending on their origin, form, duration, impact on the child’s well-being and the state of his hemodynamics. For all types of arrhythmias, cardiac and extracardiac causes should be treated simultaneously. Treatment should be comprehensive and include the prescription of neurometabolic, vascular drugs, cell membrane stabilizers and antioxidants. The interaction of these types of therapy makes it possible to ensure long-term remission and complete clinical recovery. There are situations when it is necessary to prescribe specialized antiarrhythmic therapy. Such changes include malignant arrhythmias and arrhythmogenic left ventricular dysfunction.
Clinical observation should be regular. Its frequency is determined depending on the underlying disease (rheumatism, non-rheumatic carditis, congenital heart disease, etc.), the form of arrhythmia and the characteristics of its course. Dynamic ECG recording and 24-hour ECG monitoring are required to assess the effectiveness of therapy.
How to recognize sinus arrhythmia in a child
You and your child may not be aware that they have a heart rhythm disorder. Often sinus arrhythmia is discovered by chance, as happened with my patient.
According to the classification of O.A. Kozyrev and R.S. Bogacheva in 1998, according to the clinical course, heart rhythm disturbances are divided into:
- insignificant;
- significant.
The first ones “do not bother” the patient. The general condition does not suffer, there are no complaints or clinical symptoms. The latter significantly complicate life and have an unfavorable prognostic value. This group of arrhythmias requires careful examination and timely treatment.
Complaints and symptoms, or when it’s time to see a doctor
The child may have complaints of a feeling of “interruptions” in the heart area, unexplained weakness, and dizziness. It is important to understand that preschoolers will not always describe their condition. If you suddenly notice that your baby, who usually runs, sits down to rest, or is experiencing unreasonable fatigue, immediately take him to the pediatrician. This will help you not to miss time in case of any illness.
The doctor will suspect sinus arrhythmia on auscultation if he hears different lengths of pauses between heart sounds. The pulse will correspond to age, but will be characterized by inconstancy: within one minute, too rapid repetition of beats will be replaced by a slow pace.
ECG signs
The main diagnostic method for rhythm disturbances is electrocardiography. An ECG allows you to clarify the type of change in automatism, conductivity, and identify non-physiological foci of excitation.
Sinus arrhythmia is characterized by:
- constancy of the P wave;
- a gradual increase in the distances between neighboring P or T, and then the same gradual decrease;
- stability of the PQ interval;
- normal EGC curve if you ask the patient to hold his breath.
With Holter monitoring, pronounced sinus arrhythmia in a child will be observed during sleep and physical activity. It is under these conditions that the activity of the vagus increases.
Treatment of arrhythmia
Treatment methods for arrhythmia in children depend on the causes and variant of the identified disorders.
Only an arrhythmologist (pediatric cardiologist) makes a decision on the need to treat arrhythmia. Self-treatment of the disease is strictly prohibited. This threatens the child with complications and the development of dangerous symptoms. However, given the often asymptomatic nature of many rhythm disturbances, including life-threatening ones, parents themselves should pay great attention to the problem.
To make an appointment with children's ari, fill out the online form or call us at +7 (495) 292-59-86.
How should the doctor and parents act?
Parents often came to me with complaints that the pediatrician questioned them for a very long time, prescribed numerous examinations, and then said that there was no need to treat sinus arrhythmia in a child or teenager. How so? After all, the child has a heart condition. I absolutely agree with the attending physician on this issue.
Survey plan
Sinus arrhythmia does not require special therapy. In some cases, we focus on eliminating its cause - we treat the underlying disease. But this pathology sometimes “masks” other disorders. It's important not to miss them.
The examination plan for a child with sinus arrhythmia includes:
- A thorough collection by the doctor of anamnesis of life and illness. Don't be surprised if some of the specialist's questions seem strange to you. It is necessary to clarify genetic predisposition, risk factors, and the presence of concomitant pathological processes.
- Electrocardiographic examination. It is important to carry it out at least three times - when the patient is lying down, standing, and then after physical activity.
- Stress tests. These include bicycle ergometry and treadmill. Thanks to them, it is possible to determine how the work of the heart changes during physical activity, as well as to identify hidden rhythm disturbances.
- Medicinal electrocardiographic tests. The action of certain drugs (in pediatric practice, atropine or a combination of potassium chloride and Obzidan is usually used) causes a decrease in the number of heart contractions, which confirms autonomic dysfunction.
- Holter monitoring. Your son or daughter lives with a portable device that records an ECG for at least a day. The examination will allow you to determine the circadian index - the ratio of the average number of heart beats during the day to the same indicator at night. From the age of two, 1.24 – 1.45 are considered normal values. If the index is less than 1.2, this indicates a decrease in vagosympathetic regulation, and if it increases more than 1.5, this indicates an increase in the tone of the vagus nerve. This coefficient is important for the differential diagnosis of sinus arrhythmia.
- Electroencephalography allows you to link changes in the number of heart beats with the bioelectrical activity of the brain.
- Echocardiographic examination diagnoses structural causes of sinus arrhythmia.
Perhaps the doctor will refer the patient for a biochemical blood test, echocardiography, radiography of the cervical spine, or rheoencephalography.
Sometimes viruses are a provoking factor in the development of sinus arrhythmia. Scientists have proven that herpes activates myocardial degeneration. Testing to detect the herpes virus may be required. Our main task is to clarify the cause of sinus arrhythmia and exclude other changes in heart rhythm.
Diagnosis of arrhythmia
To make an accurate diagnosis, consultation with a pediatric arrhythmologist or pediatric cardiologist is necessary. The initial examination by a specialist includes:
- Studying the medical history.
- Carrying out a full examination (palpation, percussion, auscultation).
If an arrhythmia is suspected, the doctor will refer the child for instrumental diagnostics:
- Electrocardiography
is a universal method that allows you to evaluate the work of the heart in a specific time period. - Daily Holter monitoring.
A more accurate method compared to conventional electrocardiography, as it records the work of the heart over a long period of time (days), including sleep, physical activity, various periods of activity, etc. - Load tests.
This is an analysis of cardiac activity during physical activity of varying intensity.
This method can only be used with older children. After making a diagnosis, an arrhythmologist or pediatric cardiologist may prescribe examinations aimed at identifying the causes of the disease:
- EchoCG
(echocardiography or ultrasound of the heart). Allows you to identify organic causes of the disease, for example, heart defects, tumors, etc. - Radiography.
This method is aimed at identifying extracardiac causes of arrhythmia, for example, pathology of the spine, large vessels. - EEG.
Electroencephalography is indicated in cases of suspected connection of arrhythmia with brain diseases.
The SM-Doctor clinic for children and adolescents is equipped with only modern diagnostic equipment, which allows our specialists to make an accurate diagnosis and prescribe timely treatment for the disease.