Causes of cardiopulmonary failure
Cardiopulmonary failure can be caused by:
- Bronchopulmonary pathologies. They provoke about 80% of all cases of the disease. Insufficiency is explained by bronchial asthma, obstructive bronchitis, pulmonary tuberculosis, polycystic disease, cystic fibrosis, etc.
- Vascular pathologies. This group of factors affects lesions of the pulmonary bed. The development of pathology is facilitated by compression of the pulmonary veins and arteries by tumors, sickle cell anemia, pulmonary vasculitis, and pulmonary embolism.
- Thoradiaphragmatic pathologies. This group of factors is associated with limited mobility of the diaphragm and chest. Massive pleurisy, curvature of the spine, rib fractures, etc. lead to the development of pathology.
Clinic
The main symptoms of pneumonia, which appear in both adults and children.
- Fever: occurs acutely, quickly reaches febrile levels
- Cough with copious discharge of purulent sputum; there may also be blood in the sputum (especially in the case of lobar pneumonia)
- Chest pain associated with breathing
- Shortness of breath, feeling of lack of air
- Manifestations of intoxication: severe weakness, fatigue, sweating, nausea, vomiting
- In the case of “atypical” pneumonia (Mycoplasma pneumoniae, Legionella pneumophila, Chlamydia pneumoniae, Pneumocystis jirovecii), there may be a gradual onset with a dry, unproductive cough, not without common symptoms - pain and sore throat, weakness, malaise, myalgia, headaches, pain in the abdomen - with minimal changes on the x-ray
- Elderly patients often have more severe general symptoms: drowsiness, confusion, anxiety, sleep disturbances, loss of appetite, nausea, vomiting, signs of exacerbation/decompensation of chronic diseases
Classification of the disease
Cardiopulmonary pathology can be:
- Spicy. The development of such failure usually occurs against the background of massive thromboembolism, status asthmaticus or emphysema. The pathological condition occurs within a few hours after a sharp and sudden increase in pressure in the artery.
- Subacute and chronic. In this case, deficiency can develop over several months or even years.
Heart pulmonary failure is divided into several types:
- respiratory;
- abdominal;
- cerebral;
- anginal;
- collaptoid.
Each type has its own characteristics.
results
The average age of study participants was 55 years, 2649 (53.1%) were men, and 63.4% of patients were outpatients.
- During a mean follow-up of 9.9 years (range 5.6 to 10.6 years), 11.9% (n=592) of patients in the study group were diagnosed with HF, while in the control group 7.4% (n =1712); adjusted hazard ratio 1.61, 95% CI 1.44–1.81.
- Patients with pneumonia aged ≤65 years had the lowest absolute increase in risk (but the highest relative risk) of HF compared with controls (4.8% vs. 2.2%; adjusted hazard ratio, 1.98, 95% CI 1.5–2.53 ).
- However, in patients with pneumonia over the age of 65 years, there was the highest increase in absolute risk (but the smallest relative risk) of HF (24.8% vs. 18.9%), adjusted hazard ratio, 1.55, 95% CI 1.36-1.77.
- The analysis showed that the risk of developing HF was comparable between patients receiving outpatient treatment and those hospitalized for pneumonia.
Symptoms of cardiopulmonary failure
Acute cardiac pulmonary failure is characterized by a sudden onset. The patient's condition deteriorates sharply.
Typically patients suffer from:
- pain in the heart area;
- fear of death;
- sensations of suffocation;
- reducing pressure.
Each symptom is worse when sitting or standing. This is due to the fact that blood flow to the heart is reduced.
Important! Sudden death can occur in this condition.
As the deficiency progresses, patients suffer from pain in the right hypochondrium. Increased central pressure causes the veins in the neck to swell.
Chronic deficiency develops gradually.
It is characterized by:
- severe exercise tolerance;
- constant shortness of breath;
- cyanosis of the nose, ears, fingertips and chin.
Patients often suffer from chest pain that is not relieved by nitroglycerin.
In the chronic stage, the disease manifests itself with symptoms such as:
- drowsiness;
- feeling tired;
- fast fatiguability;
- fainting.
Insufficiency is dangerous because its symptoms are easily confused with other pathologies. However, it often causes instant death. That is why the disease must be detected and treated!
CONGISTENT PNEUMONIA IN THE ELDERLY – WHAT IS THIS DISEASE DANGEROUS?
Why does congestive pneumonia appear in the elderly?
- The development of stroke, heart attack, bronchopulmonary diseases, in which in the postoperative period the patient is deprived of the ability to move independently, inevitably leads to the development of congestive pneumonia;
- The older a person gets, the more his respiratory system becomes susceptible to functional changes: weakening of the diaphragm, shallow breathing (this is inevitable for people over 65 years of age), decreased elasticity of lung tissue;
- With age, pulmonary circulation becomes more difficult. Inactive bronchial ventilation leads to the fact that, one way or another, harmful and dangerous microorganisms (anaerobes, pneumococcus, enterobacteria) begin to rapidly multiply in the area of the bronchotracheal tree and oropharynx. Their active life activity leads to the development of congestive pneumonia.
CONGESTAL PNEUMONIA: SIGNS
Due to the fact that traditional pneumonia only affects small areas of lung tissue, drug treatment will be sufficient to treat it. The situation is much worse when it comes to congestive pneumonia, when fluid stagnates in the lungs and bronchi.
Attention! Elderly people may only suffer from weakness or lack of appetite, since other symptoms are often vague, so they may not even be aware of the presence of a dangerous disease.
Hypostatic pneumonia can be diagnosed by the following signs:
- The appearance of chills;
- The occurrence of drowsiness and weakness;
- Continuous cough;
- Increased sweating (the body loses its ability to thermoregulate);
- The occurrence of shortness of breath;
- Sudden changes in body temperature;
- Slight secretion of sputum during coughing;
- Audible wheezing.
Since this disease is insidious, it is very important to diagnose it in a timely manner.
CONGESTIVE PNEUMONIA: DIAGNOSTIC MEASURES IN ELDERLY PEOPLE
This disease does not have any special symptoms, so the main task of loved ones is to sound the alarm in time, and the main task of the attending physician of an elderly person is to diagnose the disease in time. Some previously suffered diseases, as well as diseases that have become chronic, can signal the possible development of hypostatic pneumonia, namely: stroke, heart attack, cardiosclerosis, heart disease, atherosclerosis, kidney inflammation, diabetes mellitus, asthmatic syndrome, pulmonary emphysema. To confirm the diagnosis, you need to resort to:
- X-ray examination. However, the image will be characterized by opacities that identify fluid in the lung. In this case, stagnant clots, characteristic, for example, of bronchopneumonia, are also visible in the image as clouding. In other words, congestive pneumonia can be confused with another disease, and not every medical institution is equipped with equipment for examining a bedridden patient;
- Ultrasound examination. By taking an ultrasound image and thus examining the pleural cavity, you can detect the exact location of the stagnant fluid;
- Steto- or phonendoscope - listening to the lungs. The presence of this disease will be confirmed by hoarse breathing and moist rales.
Localization of secondary pneumonia is the lower lobe of the right lung (the area farthest from the heart). If the doctor diagnoses this disease incorrectly, the elderly person may fall into a coma. Untimely or incorrect treatment also leads to urinary incontinence, depression, and sudden mood swings. This symptomatology is similar to cyanide dementia, so the doctor may make a mistake with the diagnosis.
Another cause of medical error may be the symptom of shortness of breath, since the doctor may regard it as a sign of heart failure. If the diagnosis was made incorrectly, and therefore the wrong treatment was prescribed, or the person consulted a doctor late, consequences may occur in the form of:
- Impaired blood outflow, which will inevitably lead to the pulmonary veins becoming overfilled;
- Leakage of blood plasma through the walls of blood vessels. The pulmonary alveoli begin to accumulate fluid, thus, pathogenic bacteria begin to develop;
The process of replacing lung tissue with connective tissue begins.
CONGISTENT PNEUMONIA: TREATMENT METHODS FOR ELDERLY PEOPLE
This disease requires hospital treatment and continuous monitoring by doctors. Since the disease is infectious, broad-spectrum antibiotics are required. In addition, it is necessary to restore normal ventilation of the lungs, which means that a diuretic, an expectorant, an antioxidant, and an immunomodulator will be prescribed.
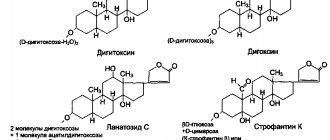
In order to ease the work of the heart, the doctor will prescribe a glycoside and a drug to improve metabolism. To free the bronchi and trachea from sputum, it is necessary to prescribe bronchoscopy. If the pleural cavity is filled with fluid, a diuretic and puncture are necessary. This therapeutic complex will allow you to quickly stabilize the patient’s condition.
In addition, it is necessary to resort to physiotherapeutic methods: a course of massage, inhalations and oxygen masks. It is also useful to perform breathing exercises, especially the Buteyko and Strelnikova complex.
Be sure to perform a set of exercises that can normalize diaphragmatic breathing:
- Taking a lying position, fold your hands on your stomach and take a slow breath, then exhale through your mouth. At the same time, try to tense your abdominal muscles and press with your hands, creating a resistance effect in order to enhance exhalation;
- Taking a standing position, spreading your arms to the sides and spreading your legs wide, inhale. Then exhale slowly, move your arms forward, bend down, and at the same time make sure that your stomach is pulled in.
In order for sputum to be expelled more easily, it is necessary to carry out positional “drainage”, which consists in the fact that the body takes certain positions, so that the liquid flows into the area of reflexogenic zones, which causes a cough. It is necessary to take several deep breaths through the nose and exhale through the mouth, while the teeth should be clenched tightly, and then cough strongly. 30 minutes before the start of this complex, you need to drink a warm decoction: linden, plantain or coltsfoot, or just tea with honey or milk.
After being discharged home, it is necessary to continue treatment through traditional medicine.
CONGISTENT PNEUMONIA: TREATMENT WITH TRADITIONAL MEDICINE
Various decoctions help perfectly in the fight against this disease:
- Decoction of thyme or creeping thyme: 2 tbsp. spoons, brew one and a half liters of boiling water, then strain and take at least 4 times a day, ½ tbsp. before meals;
- Bearberry decoction: 1 tbsp. Brew a spoon with a glass of boiling water, divide into three parts and consume each of them 30 minutes after eating;
- Decoction of viburnum berries: 2 tbsp. Brew spoons with a glass of boiling water and leave overnight. Then add honey and take 2 tbsp. spoons after meals;
- A decoction of a collection of herbs: chamomile, St. John's wort, nettle, calendula, raspberry, marshmallow, elecampane, sage, plantain and calamus. It is necessary to mix all these herbs in 3 tbsp. spoons of each.
- Brew 2 tbsp. spoons of the collection with boiling water (0.5 l.), leave overnight, strain and take half a glass. The course of admission is about three months;
- The medicine “urbech”, whose homeland is Dagestan. Grind apricot kernels (3 kg) and flax seeds (3 kg), be sure to store the mixture in the refrigerator. When treatment is necessary, you need to take butter (1/2 pack), add 1 tbsp. spoon of the mixture and bring to a boil, then remove from heat, let cool and add 1 tbsp. a spoonful of honey. Then put it in the refrigerator and let it harden; if necessary, add it to the patient’s porridge or simply spread it on bread.
SURGICAL INTERVENTION FOR HYPOSTATIC PNEUMONIA
Most often, bedridden patients who cannot breathe need surgical intervention. In order to alleviate suffering, the doctor may prescribe a chest puncture. Thus, it becomes possible to “pump out” the fluid and free the lungs. The procedure is performed only in a hospital, by a qualified surgeon and under general anesthesia.
HYPOSTATIC PNEUMONIA IN ELDERLY PEOPLE: PREVENTIVE MEASURES
As you know, it is better to prevent the development of any disease than to treat it later. Since hypostatic pneumonia is a complication of another disease, older people need to take care and follow the following rules:
- Always ensure that your feet are dry and warm;
- Practice daily walks in the fresh air;
- Take time for proper daily rest;
- To refuse from bad habits;
- Pay attention to proper and nutritious nutrition;
- Allergy sufferers should especially monitor the condition of their disease;
It is mandatory to undergo the vaccination procedure in order to prevent the development of influenza during its epidemic.
If we are talking about a bedridden elderly person, then relatives need to prevent the development of congestive pneumonia: turn the patient over more often, massage his chest, use cups and mustard plasters, perform the previously described physical exercises with him, make sure that the room in which the person is lying , it was well ventilated and the air was humidified.
Modern medicine makes it possible to treat hypostatic pneumonia in older people without any problems, only if they timely seek qualified medical help and correct diagnosis. At the same time, the desire of the patient himself and his efforts during therapeutic exercises are also important, so relatives need to adjust the patient accordingly. And after treatment, it is important for an elderly person to lead a healthy and active lifestyle.
Diagnosis of pathology
For diagnostics, specialists use a whole range of modern methods. All of them make it possible to identify the underlying pathology and assess the degree of decompensation.
Diagnostics include:
- Examination by a cardiologist and pulmonologist. Typically, specialists pay attention to a barrel-shaped deformation of the chest, swelling of the legs and feet, a frequent arrhythmic pulse and a decrease in blood pressure.
- Assessment of blood gas parameters.
- Chest X-ray.
- Pulmonary angiography and ventilation-perfusion lung scintigraphy. These examinations are carried out if PE is suspected.
- Assessment of respiratory function (function of external respiration). Such an examination allows us to determine the nature and severity of pulmonary ventilation impairment and bronchospasm.
- ECG. This examination is aimed at determining the cause of overload of the right side of the heart. The method also makes it possible to identify indirect and direct markers of ventricular hypertrophy.
- EchoCG. This technique allows you to assess the hemodynamics of the heart, determine the size of its cavities, and determine the degree of pulmonary hypertension.
Treatment
Insufficiency therapy is carried out comprehensively and depends on:
- underlying disease;
- general condition of the patient;
- concomitant pathologies and other factors.
For pulmonary embolism, for example, the following is carried out:
- oxygen therapy;
- pain relief;
- thrombolytic therapy.
In some cases, the only effective way to get rid of the pathology is thromboembolectomy from the pulmonary artery.
If the deficiency has developed against the background of bronchopulmonary pathology, the following are used:
- mucolytics;
- bronchodilators;
- expectorants.
For pulmonary tuberculosis, therapy is carried out using antibiotics.
For specific lung diseases, interferon, cytostatics and glucocorticoids are used.
At all stages, therapy is carried out using oxygen inhalation. Vasodilators are prescribed to reduce pulmonary vascular resistance. For swelling, diuretics are additionally indicated. They allow you to restore water and electrolyte balance.
If drug therapy does not give the desired result, surgical interventions are performed.
Today specialists carry out such operations as:
- balloon septostomy;
- reduction of lung tissue;
- sympathectomy.
In the most advanced cases, a lung or lung and heart transplant may be required.
All operations are quite complex and lengthy. That is why endovascular techniques are being actively developed and implemented today. They make it possible to reduce trauma and the duration of rehabilitation, and create the opportunity for patients to recover even in difficult situations.
Of course, in case of any pulmonary or cardiac pathologies, specialists will try to eliminate them with the help of medications and the most minimally invasive interventions possible. Our doctors use all known modern techniques. Particular attention is paid to the prevention of pathologies. Of course, several specialists are involved in working with the patient at once. This allows you to find the optimal solution even in difficult situations.
Prices for therapy depend on a lot of factors, but we never inflate them. Thanks to this, you can benefit from professional support even on a limited budget. The exact price of therapy at a clinic in Moscow will be announced in advance. This will allow you to plan your expenses.
Management of patients with CAP in outpatient settings
For mild pneumonia, antibacterial treatment of adults and children can be completed with stable normalization of body temperature for 3–4 days (total course duration 7–10 days). If there is clinical/epidemiological evidence of mycoplasma or chlamydial infection, the duration of therapy should be 14 days. An initial assessment of the effectiveness of therapy should be carried out 48–72 hours after the end of the course of treatment (re-examination). If symptoms persist or progress, it is necessary to reconsider the tactics of antibacterial therapy and re-evaluate the advisability of hospitalization.
According to the recommendations of the Russian Respiratory Society, outpatient patients are divided into 2 groups, differing in etiological structure and tactics of antibacterial therapy (see Table 1. Antibacterial therapy of CAP in outpatients):
Table 1.
Antibacterial therapy of CAP in outpatients
| Group | Most common pathogens | Drugs of choice | Alternative drugs | Patient characteristics |
| Mild CAP in patients under 60 years of age without concomitant pathology | S. pneumoniae M. pneumoniae C. pneumoniae H. influenzae | Amoxicillin orally or macrolides (azithromycin, clarithromycin) orally | Respiratory fluoroquinolones (levofloxacin, moxifloxacin) orally | |
| Mild CAP in patients over 60 years of age and/or with signs of concomitant pathology | S. pneumoniae C. pneumoniae H. influenzae S. aureus Enterobacteriaceae | Amoxicillin + clavulanic acid or Amoxicillin + sulbactam orally | Respiratory fluoroquinolones (levofloxacin, moxifloxacin) orally | Concomitant diseases affecting etiology and prognosis: COPD, diabetes, congestive heart failure, liver cirrhosis, alcohol abuse, drug addiction, exhaustion |
Prevention
The prognosis for the development of cardiopulmonary failure is very serious. Acute conditions are extremely life-threatening. It should be taken into account that the deficiency is progressive. In the absence of adequate therapy and preventive measures, patients live no more than 2.5-5 years.
Primary prevention of deficiency is:
- quitting smoking;
- maintaining a healthy lifestyle;
- preventing the occurrence of any pathologies of the heart and lungs;
- eliminating risk factors that contribute to exacerbation of the disease.
It is very important to quickly identify and treat the underlying diseases.
If there is any suspicion of deficiency, you should immediately contact specialists to conduct a full examination and select funds for adequate therapy.
Study design
A prospective cohort study included 4988 adult patients with pneumonia without HF seen at 6 Canadian medical centers from 2000 to 2002.
Patients were matched by gender, age and place of treatment (outpatient treatment or hospitalization) in a ratio of 1 to 5 with individuals without pneumonia (n=23,060).
The primary endpoint of the study was the risk of hospitalization due to HF and a composite endpoint of HF and death.
The Cox model was used as a statistical analysis method.