- Thrombotic vascular lesions
- Fat embolism
- Air embolism
- Which vessels can be affected by embolism and how does it manifest?
- Carotid embolism
- Occlusion of mesenteric vessels and renal artery
- Peripheral vascular occlusion
- Treatment and prevention of pathology
- Prevention and treatment of fat embolism
- Prevention and treatment of air embolism
- Amniotic fluid embolism
- Causes
- Treatment and prevention
Vascular embolism is a condition in which the lumen of a blood vessel is completely or partially blocked. This leads to disruption of blood supply, which causes oxygen starvation of tissues. If left untreated, they gradually die off as the cells stop receiving oxygen and nutrients. Vessel blockage can be caused by:
- blood clots;
- particles of adipose tissue;
- air bubbles;
- foreign objects.
Regardless of the cause, vascular embolism poses a threat to the health and life of the patient. This condition requires treatment, which can be conservative or surgical.
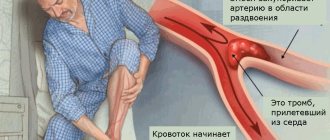
Thrombotic vascular lesions
It is the most common type of embolism and can occur with the following diseases:
- varicose veins;
- heart disease (heart attack, myocarditis, etc.);
- excess body weight;
- thrombophilia.
The risk of pathology increases with a hereditary predisposition to thrombosis, after extensive surgical interventions, when taking hormonal contraceptives, and low physical activity. The most dangerous for the patient are thrombotic lesions of the great vessels of the brain, kidneys and intestines. In this case, there is a direct threat to life due to the development of tissue necrosis of vital organs. If treatment is not carried out in a timely manner, the patient's life can be saved, but he may remain disabled.
If a blood clot occludes a peripheral vessel, gangrene of the limb may develop and amputation may become necessary. Thromboembolism of peripheral arteries is easier to diagnose, which helps prevent severe complications.
Pulmonary thromboembolism is very life-threatening. A blood clot can block the main trunk of the pulmonary artery or its branch. This condition occurs suddenly, and the pathology leads to a very rapid deterioration in the patient’s well-being. He develops cardiopulmonary failure, which ends in cardiac and respiratory arrest.
The main cause of the pathology is the migration of a blood clot from the veins of the lower extremities or pelvis.
Which doctor should I contact?
Embolism is treated by specialists of different profiles - it depends on the type and severity of the disease.
List of main doctors:
- phlebologist;
- angiosurgeon;
- cardiac surgeon;
- neurosurgeon;
- pulmonologist;
- ophthalmologist;
- resuscitator.
Fat embolism
Pathology occurs:
- when injecting oil solutions;
- for injuries and damage that are accompanied by bone fractures and vascular injury;
- with necrotic lesions of pancreatic tissue.
Lipid droplets enter the blood from the yellow bone marrow if the damaged bone is damaged or as a result of surgery. They are able to merge into a single whole and move with the bloodstream throughout the body. Having reached a certain size, the accumulation of adipose tissue particles blocks the lumen of the vessel. Most often, the pathology affects the tissues of the spinal cord, brain, heart, and lungs.
Disease prevention
To avoid embolism, eliminate factors that negatively affect blood circulation.
Prevention methods:
- control your weight;
- treat infectious pathologies in a timely manner;
- avoid physical inactivity;
- stop smoking and drinking alcohol;
- spend more time outdoors;
- For varicose veins of the lower extremities, wear compression garments.
If your blood viscosity is high, take heparin-based medications to prevent blood clots; your doctor will determine the dosage and duration of the course.
Products to improve blood circulation - hot peppers, onions, garlic, pomegranate and citrus fruits, cinnamon, fatty fish, beets, turmeric, herbs.
Embolism is a dangerous, rapidly progressing disease in which the lumens in the vessels are blocked and circulatory failure occurs. It is often a consequence of inattention to one’s own health - undergo a preventive examination, monitor basic blood counts 1-2 times a year. With timely diagnosis, drug therapy is carried out; in severe cases, surgery cannot be avoided; there is a high probability of death.
Air embolism
The pathology is characterized by blockage of the vessel with air or gas bubbles. The reason is:
- improper administration of intravenous injections;
- damage to large vessels;
- decompression sickness.
If a large vein is injured and the bleeding is not stopped in time, air can get inside and move with the blood along the arterial bed, which ultimately leads to a blockage. A type of air embolism is gas embolism, which is caused by the so-called decompression sickness. It develops in people who engage in scuba diving. If a person rises to the surface too quickly, the inhaled gas mixture does not have time to be absorbed. Air bubbles block the vessels and lead to embolism. The person may lose consciousness, and in severe cases, a stroke is possible.
Diagnosis of embolism
{banner_banstat9}
If an embolism is suspected, act quickly, since delay is fraught with death.
Basic diagnostic methods:
- clinical blood and urine analysis;
- blood chemistry;
- plain x-ray and with contrast;
- ECG, ultrasound of the heart;
- arteriography to assess lung function;
- scintigraphy;
- dopplerography;
- fundus examination;
- measurement of arterial parameters;
- CT, MRI.
During treatment, diagnostic measures are carried out several times to assess the degree of effectiveness of therapy and timely relief of complications.
Which vessels can be affected by embolism and how does it manifest?
Blockage of the lumen can occur in any vessel. Depending on the location of the pathology, its symptoms vary. Signs of arterial embolism are:
- a sharp drop in blood pressure;
- irregular pulse and breathing;
- sweating;
- pallor;
- chest pain that radiates to neighboring areas of the body;
- weakness, dizziness;
- loss of consciousness.
Carotid embolism
Signs of pathology are:
- weakness and dizziness;
- headache;
- deterioration in coordination of movements;
- fainting state.
Occlusion of mesenteric vessels and renal artery
In this case, the superior and inferior mesenteric arteries are affected. The pathology is manifested by severe abdominal pain, bloating, loose stools mixed with blood, and impaired intestinal motility.
If there is a blockage of the renal artery, the patient experiences severe pain in the lower back. The functioning of the kidney is disrupted, which causes difficulty urinating until it completely stops, and blood is released in the urine.
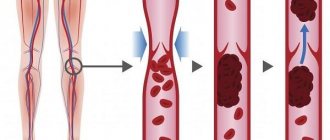
Peripheral vascular occlusion
Embolism of the arteries of the extremities leads to pain in the affected area, which is accompanied by spasms and muscle cramps. Due to impaired blood supply, the skin turns pale. Trophic ulcers appear on the surface - non-healing wounds that can lead to gangrene.
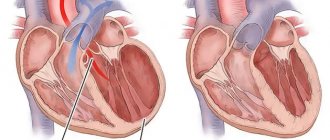
Causes of arterial embolism
A number of diseases can lead to arterial embolism. The most common cause of embolism is atrial fibrillation, when the atria do not contract, causing blood stagnation and the formation of blood clots. At some point, a fragment of this thrombus breaks off and is carried through the bloodstream to some organ, blocking blood flow in it and causing acute ischemia.
Other less common causes of blood clots and embolism include:
- Arterial aneurysms (pathological expansion of the diameter of the vessel)
- Artery injury
- Hypertensive crisis, with dissection of a section of the artery and the formation of a blood clot
Treatment and prevention of pathology
Treatment of the disease depends on its type. A treatment protocol has been developed for each type of pathology. It is aimed at normalizing vital functions and eliminating the cause that led to blockage of the vessel.
Conservative therapy includes taking medications:
- anticoagulants;
- glycosides;
- fibronolytics;
- glucocorticosteroids.
If the pathology occurs due to injury or infection, antibiotics are prescribed.
A patient with thromboembolism is prescribed ozone therapy, which eliminates the lack of oxygen in tissues and has a bactericidal effect.
If drug therapy is not effective enough, surgery is performed to remove the blood clot. To prevent thromboembolism, it is necessary to regularly monitor blood clotting parameters. There is a special analysis for this - a coagulogram. If necessary, a patient at high risk of thrombosis should take anticoagulants.
Varicose veins and heart disease are factors that provoke thrombotic damage to the arteries. If you have such diseases, it is important to monitor your condition and undergo timely treatment.
Prevention and treatment of fat embolism
In case of fat embolism, the patient needs to be hospitalized in the intensive care unit and connected to a ventilator. Drug therapy involves taking drugs that dissolve fatty particles. The patient is also prescribed anticoagulants, cardiac glycosides, and oxygen therapy.
To prevent fat embolism, it is necessary to eliminate factors that could cause lipid particles to enter the blood. In case of fractures, it is important to stop the bleeding as soon as possible, correctly fix the injured limb, monitor the patient’s condition, and control blood pressure.
Prevention and treatment of air embolism
If there are signs of pathology, the patient needs emergency care. He is fitted with a venous catheter for air aspiration and connected to an artificial respiration apparatus. To eliminate tissue hypoxia, oxygen instillations and hyperbaric oxygenation are performed.
To prevent air embolism, scuba divers must strictly follow safety rules when ascending from depth to the surface in order to prevent decompression sickness. The pathology can be caused by air entering an injured blood vessel, so it is important to promptly provide medical care to patients with such injuries and monitor their health.
When injecting drugs into a vein, it is important to follow safety requirements to avoid air bubbles entering the vessel.
Symptoms of arterial embolism
Symptoms of embolism depend on where the clot stops in the artery. Thromboembolism can be suspected if the following signs are present:
- Sudden coldness of the extremity
- No pulse
- Difficulty in movement
- Tingling or numbness
- Decreased sensitivity
- Pain or spasms in the muscles of the affected limb
- Sharp pallor of the skin of the affected limb
If blood flow is not restored in a timely manner, the following symptoms occur:
- Blue or marbled skin color
- Formation of blisters filled with bloody contents
- Absence or sharp decrease in range of motion
- Lack of sensation in the affected limb
- Impossibility of even passive movement in the joints (contracture)
- Signs of ischemic gangrene - tissue breakdown
Amniotic fluid embolism
Amniotic fluid embolism is a pathological condition in pregnant women. It occurs when amniotic fluid enters the mother's bloodstream. This liquid contains prostaglandins and other components, the effect of which causes an anaphylactoid reaction.
Pathology manifests itself in the following forms:
- swelling of the lung tissue with the development of acute respiratory failure;
- cardiac shock, which is characterized by a thread-like rapid pulse, a sharp decrease in pressure, nausea and vomiting, pallor, bluish skin, loss of consciousness;
- convulsive syndrome, which affects all muscle groups;
- hemorrhagic bleeding from the nose and mouth, vagina;
- multiple organ failure, which manifests itself as a disruption in the functioning of the main organs and systems.
Causes
Amniotic fluid can enter the bloodstream of a pregnant woman if the pressure inside the uterus increases, the pressure in the veins of the uterus decreases, or if the vessels that contact the amniotic sac are damaged.
Risk factors are:
- multiple pregnancy or high fetal weight;
- breech presentation of the fetus;
- polyhydramnios;
- low elasticity of the cervix;
- rapid labor;
- individual anatomical features of the birth canal.
The development of embolism against the background of a decrease in venous pressure can occur in patients with diabetes mellitus, heart defects, and preeclampsia. Women with low vascular tone due to frequent childbirth and patients taking diuretics and antihypertensive drugs are susceptible to pathology.
The entry of amniotic fluid into the blood due to damage to the amniotic sac and vascular injury occurs during placental abruption, careless cesarean section or embryotomy - an operation to remove the fetus through the birth canal in the event of intrauterine death.
Treatment and prevention
In case of amniotic fluid embolism, a woman needs urgent medical care, which is aimed at eliminating the anaphylactoid reaction. First of all, oxygen therapy is used, which consists of connecting the patient to an artificial respiration apparatus and using oxygen instillations. To normalize hemostasis, blood products, blood replacement fluids, and high doses of glucocorticosteroids are used.
If the above measures lead to a positive result, delivery is possible naturally through the birth canal. If there is no improvement, an urgent caesarean section is required. To prevent amniotic fluid embolism, it is important to avoid conditions that can lead to such a pathology. It is important to visit your doctor in a timely manner to monitor the progress of pregnancy and eliminate uterine hypertonicity. In the case of placental insufficiency and other pathological conditions, it is necessary to take timely measures aimed at preventing embolism.
Discussion
The presented clinical case describes a rather rare observation of the development of paradoxical air embolism with damage to the vessels of the brain, coronary arteries and lungs.
We found only a few descriptions of similar clinical observations in the literature. It is worth noting that air embolism of the coronary vessels, described in all literature sources, manifested by changes in electrocardiograms and hemodynamic instability, regressed within a short period of time (up to 30 minutes), against the background of inotropic and infusion therapy. Also, in all observations, the predominant entry of air emboli into the right coronary artery was noted [7, 8]. Venous air embolism is a fairly common complication of neurosurgical interventions performed in a sitting position [2, 4, 9-12]. According to various authors [1-3, 5, 11, 13], the frequency of this complication ranges from 1.6-76%, depending on which episodes of VVE are recorded by the authors (all or only massive ones), and the diagnostic method used VVE, which have different sensitivity. The most common target organ for air embolism is the lungs. The severity of pulmonary injury varies from asymptomatic to ARDS [1, 2]. In the presence of an open foramen ovale or an intrapulmonary shunt, the prerequisites are created for air to enter the systemic circulation [1, 2, 6, 14]. In this case, ischemic damage to any organs can occur, but the brain, skin, and myocardium are most often affected [1, 2, 5]. The incidence of open foramen ovale in the population, according to various authors (primarily according to the results of a sectional study of random unselected deaths from various causes), ranges from 5 to 33% [3, 5, 13, 15]. Preoperative examination, including transthoracic Doppler ultrasound with the Valsalva test and the use of contrast, does not allow identifying this anomaly in 1/3-½ of patients [16]. First, the transthoracic Doppler method is not sensitive enough to detect a patent foramen ovale; secondly, in some cases, the oval window begins to function only in conditions of increased intrathoracic pressure during mechanical ventilation. The situation is especially aggravated with the development of VVE, since the resulting increased pressure in the right ventricle due to the massive entry of air into the pulmonary capillaries leads to an increase in pressure in the pulmonary circulation and the opening of the oval window. This is clinically quite important information in the aspect of preventing PVE: 1) using even transesophageal echocardiography we can, and not always, diagnose the presence of a functioning foramen ovale in a patient; 2) the presence and functioning of vascular anastomoses between the pulmonary artery system and the bronchial arteries cannot be diagnosed at all; they are responsible for deaths due to PVE with the verified absence of septal defects in the heart [17].
There are currently no specific methods for treating lung damage caused by venous air embolism. There are a number of studies showing the effectiveness of hyperbaric oxygen therapy in patients who have undergone VVE. It is worth noting that this therapy was used in scuba divers who, due to a violation of the ascent technique, suffered decompression sickness, when the appearance of nitrogen bubbles in the bloodstream was also noted [18, 19]. There is evidence that mechanical ventilation is 100% effective in flushing out nitrogen and thus reducing the volume of air bubbles [20]. In general, treatment of VLE is symptomatic and aimed at correcting organ failure. In VLE, lung damage often has the character of classic ARDS [19, 21]. In these cases, according to the open lung concept, respiratory support is provided, including a recruitment maneuver and the use of an adequate level of PEEP. In the presence of a patent foramen ovale or intrapulmonary shunt leading to PVE, multiple organ failure may develop, requiring an appropriate approach and intensive care [22]. Brain damage in PVE necessitates neuroprotection. One of the most effective methods of neuroprotection is retrograde cerebral perfusion and cerebral or systemic hypothermia, but the effectiveness of this technique in patients with paradoxical air embolism is currently poorly studied [12, 23, 24]. Air embolism of the coronary vessels can lead to the development of myocardial infarction, the clinical and laboratory manifestations of which are indistinguishable from myocardial infarction of atherothrombotic origin. However, given the absence of coronary thrombosis, approaches to the treatment of acute myocardial infarction due to PVE differ from the accepted standards of management of patients with acute coronary syndrome. It is obvious that fibrinolytic, antiplatelet and anticoagulant therapy in this category of patients will be ineffective and even dangerous due to the risk of intracranial hemorrhagic complications when administering anticoagulants and fibrinolytics against the background of a fresh neurosurgical wound. The main therapeutic options are correction of central hemodynamics and, if necessary, the use of inotropic support [25]. It also seems advisable to prescribe β-blockers, which ensure, firstly, prolongation of diastole and thus improvement of coronary perfusion, and secondly, a decrease in myocardial oxygen demand and a decrease in the necrosis zone.
The lack of specific treatments for venous air embolism and PVE and the severity of their course emphasize the importance of prevention. According to a number of authors [2, 14, 16, 26, 27], the use of transesophageal echocardiography during surgery allows one to quickly detect and exclude the possibility of venous air embolism in patients at risk. Installing a transesophageal sensor and fixing it in such a way that after transferring the patient to a sitting position, the superior vena cava, right atrium and LV are visible on the monitor screen, allows timely detection of the appearance of air microbubbles in the bloodstream. This method also allows intraoperatively to determine the presence and functioning of a patent foramen ovale, which theoretically will make it possible to reduce the risk of venous and paradoxical air embolism [2, 16]. However, the problematic nature of this reasoning is discussed above.
The method developed by Bunegin and Elbin for evacuating an air embolus from the right side of the heart through a special multilumen catheter is very effective in the treatment of VLE, but correct installation of an aspiration catheter is far from a simple procedure that should be carried out under conditions of radiological control [28].
Naturally, methods for preventing VVE in neurosurgical patients operated on in a sitting position can reduce the incidence of VVE. Thus, it is believed that the risk of developing VVE is reduced by performing surgery in a semi-sitting position with the foot end of the operating table raised according to the method of S. Jadik et al. [29]. In this position, the hip joints are flexed to a maximum of 90°, the legs are raised up so that the patient's feet are higher than his head. The body is maximally deflected posteriorly, the head is deflected and fixed anteriorly. With this position of the head, it is necessary to ensure that there is sufficient space to perform compression of the jugular veins. This position, by increasing pressure in the right atrium, also reduces the risk of VVE. This is not the only publication where the authors try to avoid negative intrasinus pressure by raising the lower extremities, forced infusion therapy with colloid solutions and other tricks [30]. In one of these works, it was generally proposed to put on patients special pneumatic compression pants (“military anti shock trousers”), which, during inflation, squeeze out the deposited blood from the vessels of the lower extremities [31]. The trouble with all these preventive approaches is that they are all very limited in their effectiveness and their preventive effect has not been confirmed in serious studies [1, 2].
Strictly speaking, there are three reasons for the development of VVE in neurosurgical patients operated on in a sitting position: 1) damage to the walls of the sinuses and large veins of the brain during trepanation and access (an almost inevitable situation); 2) the absence of a protective mechanism for the collapse of the walls of damaged sinuses and veins due to the rigidity of their walls (a mechanism that works in peripheral veins); 3) negative pressure in the veins and sinuses of the brain due to the postural effects of blood circulation [1, 2]. The last point is the only one that can really be influenced, and several methods have been proposed for this [32].
1. Positive end-expiratory pressure. Alas, the method turned out to be not only ineffective, but also dangerous. At high PEEP values, the effect on the value of intrasinus pressure was the opposite - it decreased, apparently due to a decrease in volumetric cerebral blood flow [32]. One study using contrast echocardiography showed that PEEP promotes the transition of air emboli from right to left, i.e., increases the risk of PVE [33].
2. Inflatable neck tourniquet. This simple device allows, due to external compression of the jugular veins in the neck, to increase the pressure in the sinuses of the brain above atmospheric pressure [34]. The method is 100% effective, but labor-intensive, since for safety it requires catheterization of one of the jugular veins (control of venous pressure) above the level of the tourniquet [32].
3. Controlled moderate hypercapnia. The method was first described by a group of German authors back in 1991 [35] and also turned out to be highly effective, but at the same time simple to implement [32].
However, the most effective method of preventing VVE in neurosurgical patients is to avoid operations in the sitting position and switch to surgery in the supine position [36].
What is an embolism?
Embolism is a pathology exclusively of the arterial vascular bed, which is based on the closure of its lumen at a certain level with partial or complete cessation of blood flow, caused by factors not related to the pathology of the affected vessel. Emboli are those substances of the internal environment of the body or the environment that block the vascular lumen. It means that:
- Embolism is caused by the entry or migration of emboli into the arteries of the systemic or pulmonary circulation from other parts of the vascular bed;
- Emboli can have a different nature: blood clots, blood clots, detached atherosclerotic plaques, fat cells and oily solutions, air;
- Sources of emboli can be arterial and venous vessels of any location, as well as the heart;
- The diameter of the embolus determines the size of the artery it will block;
- It is impossible to predict which particular arterial vascular bed the embolus will fall into.
The pathogenesis of embolism can occur in three ways:
- The source of emboli is arterial vessels. In this case, the pool in which the breakdown occurred is affected. In this case, a thrombus or atherosclerotic plaque, breaking away from its place in a vessel of large diameter, becomes an embolus and migrates to smaller vessels in the basin of its branching;
- The source of emboli are venous vessels. Their role may be clots, air, or fat cells. Their migration is a little more complicated, since they first enter the heart from the veins, from where they are released in any direction (brain, limbs, intestines, kidneys, etc.);
- The source of emboli is the heart. These are, as a rule, small blood clots that form against the background of arrhythmias. After they break away from their usual location, they migrate to any arterial vessels.
Embolism is always an acute condition that requires urgent measures. Emboli entering arterial vessels leads to cessation of blood flow. This is fraught with ischemia, which can turn into gangrene or organ infarction (within 6-12 hours). This feature distinguishes it from arterial thrombosis, which is a chronic process that compensates for lost blood flow through collateral (additional) vessels.
Treatment of embolism
Since embolism is an acute disease, its treatment requires urgent measures. The sooner they are provided, the better the prognosis for the patient. Differentiated treatment tactics are given in the table.
| Type of embolism | Complex of therapeutic measures |
| Thromboembolism |
|
| Air embolism |
|
| Fat embolism |
|