Myocardial infarction is the leading cause of death on the planet
Every year, about 18 million people die from cardiovascular diseases worldwide (WHO data). Heart disease is the leading cause of death on the planet. Myocardial infarction is one of the forms of IHD (coronary heart disease), which leads to the formation of muscle tissue necrosis. The cause of the development of the pathology is insufficient blood supply to the area of the heart muscle, resulting from obstruction of the lumen of the coronary artery.
Vessels can become clogged during surgery, atherosclerosis, fat embolism and severe spasm. Risk factors that increase the likelihood of developing myocardial infarction include hypertension, smoking, obesity, alcoholism, physical inactivity, previous infections and psychological stress.
Causes of myocardial infarction
Etiology of MI
- sudden obstruction to blood flow in the branches of the coronary artery (vessels supplying the heart). Most often, such an obstacle is an atherosclerotic plaque with a blood clot.
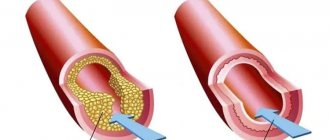
Atherosclerosis in the walls of the arteries is the formation of peculiar “growths” - plaques consisting of fatty, fibrous tissue, calcium, and which, as they progress, narrow the lumen of the vessel up to 90% or more. At the time of increased blood pressure, physical effort, or psycho-emotional stress, rupture of an atherosclerotic plaque is possible, the reaction to which is thrombosis.
Less commonly, the cause is a prolonged, prolonged spasm
coronary artery in the absence of significant atherosclerosis, or a complication of other diseases: congenital malformations, trauma to the coronary arteries, vasculitis, embolism, tendency to hypercoagulation (increased blood clotting), syphilis.
There are a number of risk factors
, repeatedly increasing the likelihood of myocardial infarction.
There are non-modifiable ones, that is, those that cannot be influenced:
- male gender (up to 50-55 years, then the incidence levels off),
- age,
- genetic conditioning (coronary artery disease and other manifestations of atherosclerosis in blood relatives);
- low physical activity (hypodynamia),
- obesity or increased body weight,
- smoking (active or passive),
- arterial hypertension,
- diabetes mellitus and metabolic syndrome,
- dyslipidemia.
And
modifiable, by changing which you can significantly reduce the likelihood of disease:
How to recognize myocardial infarction: symptoms and signs of the disease
The main sign of myocardial infarction is severe chest pain, which can radiate to the left shoulder, neck, ear and interscapular area. The intensity of pain is closely related to the area of damage to the heart muscle. On average, an angina attack lasts from 15 to 60 minutes. In patients with diabetes mellitus, cardiac pathology can be painless.
Additional symptoms of myocardial infarction include arrhythmia, systolic murmurs, weakness, anxiety, and profuse sweating. With large-scale lesions of the heart tissue, a nonproductive cough and shortness of breath appear. Symptoms of myocardial infarction also include sudden cardiac arrest.
Necrosis of an area of muscle tissue leads to fever, which lasts from 3 to 10 days. The patient continues to have signs of heart failure and blood pressure drops. An atypical course of a heart attack occurs in elderly people with severe symptoms of cardiosclerosis and circulatory disorders.
Symptoms of myocardial infarction
The main manifestation of a heart attack is very intense, burning, baking, squeezing, pressing, tearing or “dagger” pain behind the sternum
. The pain may spread to the left arm, scapular region, shoulder, neck, and lower jaw.
The duration of the episode is always more than half an hour, the slightest physical stress causes increased pain. An important sign is the lack of analgesic effect of nitrates. Patients may also experience severe weakness, shortness of breath, rapid heartbeat, sweating, and nausea. Most people feel anxiety, doom, and fear of death.
In addition to the typical variant, there are several more atypical
, capable of masquerading as other diseases of the internal organs. Among these are abdominal (epigastric pain, nausea, vomiting), asthmatic (nasty dry cough, suffocation), cerebral (headache, loss of coordination of movements), arrhythmic, erased version (deterioration of sleep, emotional background, feeling of inexplicable discomfort in the chest, sweating ). It is also possible that there are no symptoms—a “silent” heart attack, which accounts for up to 20% of all MIs.
Clinical manifestations
Myocardial infarction can be either the first manifestation of coronary heart disease or occur against the background of long-term angina. The main symptom of myocardial infarction is an attack of unusually intense chest pain, which in patients with angina pectoris does not go away after taking the usual doses of nitroglycerin.
The pain is usually wave-like and can often spread to the left arm, shoulder blade, neck, and teeth. Myocardial infarction occurs both against the background of high blood pressure, and may be accompanied by a decrease in blood pressure with a sharp deterioration in the general condition (severe weakness, cold sweat, nausea). One of the characteristic signs of a heart attack is the fear of death.
Manifestations of a heart attack may differ from the classic picture. There are so-called atypical forms.
Abdominal form
manifested by severe abdominal pain, nausea, vomiting, and digestive disorders.
Asthmatic form
may occur as an attack of bronchial asthma (shortness of breath, difficulty breathing, feeling of lack of air). One of the most insidious forms of myocardial infarction is painless, which occurs without a typical painful attack (angina). The only manifestation of this form may be an unexplained deterioration in general condition, decreased tolerance to physical activity, and weakness.
Diagnosis of myocardial infarction
It is possible to recognize acute myocardial infarction taking into account:
- A characteristic clinical picture
(severe pain in the chest area or the heart area), medical history (duration of a painful attack of more than 30 minutes, lack of results from taking nitroglycerin, presence of previously established coronary heart disease, risk factors) - Changes in the ECG
(negative T wave, pathological Q, QS complexes, ST segment elevation in leads corresponding to the location of the damage to the heart muscle) - Laboratory diagnostic data
(general blood count: increased ESR, leukocytes; biochemical indicators: increased aspartate aminotransferase, alanine aminotransferase, fibrinogen, appearance of CP protein; presence in the blood of cardiac-specific markers of cardiac muscle cell death: myoglobin CPK, LDH, tryponins). - Valuable information is provided by EchoCG, which reveals a local violation of myocardial contractility and thinning.
Providing first aid for myocardial infarction
When symptoms of a heart attack appear, the patient should be placed in a reclining position with knees bent or seated on a chair with a backrest. You should also loosen buttons, loosen ties, and loosen tight clothing. After this, you need to call an ambulance. Nitroglycerin can only be given if you have high blood pressure. If the patient has hypotension, then the drug should not be used. Taking nitroglycerin in the presence of low blood pressure can lead to the development of collapse. If the patient is not allergic to aspirin, then you need to give him 300 mg of this medicine.
The tablet must be chewed and washed down with water. In this case, it will act quickly. In case of cardiac arrest, loss of consciousness and agonal breathing, cardiopulmonary resuscitation should be started immediately.
Treatment of myocardial infarction
Myocardial infarction
- an emergency disease in cardiology and serves as an indication for immediate hospitalization in intensive care.
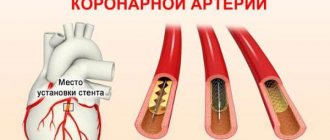
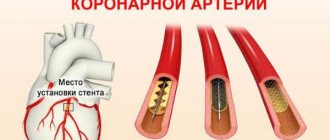
The number one task for doctors is to restore blood flow
in a thrombosed vessel. They achieve this in different ways. The priority and most effective is surgical intervention - angioplasty with stenting of the affected area of the artery or coronary artery bypass grafting. In parallel, medications are used that inhibit the development of a blood clot - disaggregants (aspirin, clopidogrel) and anticoagulants (heparin), and if immediate surgery is not possible, thrombolytics - drugs that dissolve the blood clot (alteplase, prourokinase).
Pain relief
carried out with narcotic analgesics, neuroleptics, intravenous infusions of nitroglycerin.
The size of the necrosis zone can be reduced by reducing myocardial oxygen consumption by using beta-blockers (metoprolol, bisoprolol, atenolol), ACE inhibitors (enalapril, lisinopril, ramipril), and oxygen therapy.
For arrhythmias
antiarrhythmics are used (magnesium, lidocaine, amiodarone), atropine for bradycardia. Anxiolytics and sedatives are prescribed to ensure psycho-emotional peace of the patient.
Strict bed rest
in the early stages of treatment and fractional meals, limited in volume and calorie content.
Myocardial infarction - rapid diagnosis and first aid
07.09.2021
infarction (heart attack) is the death of myocardial tissue due to insufficient oxygen supply. It develops as a severe complication of atherosclerosis . The development of a heart attack leads to death, so the patient needs emergency medical care. And in order to provide it on time, you need to be able to quickly diagnose a heart attack.
Causes of myocardial infarction
Tissue malnutrition occurs when the duct in the coronary artery becomes narrowed or blocked. This happens in the case:
- formation of a large atherosclerotic plaque;
- blood clot formation and arterial ;
- blockage of an artery by an air bubble or in case of injury.
Most often, it is atherosclerosis that leads either to severe narrowing of the artery , or to rupture of the plaque and the formation of a blood clot at the site of the crack.
Symptoms of myocardial infarction
Symptoms may come slowly if the supply of the myocardial area is not completely blocked, but is difficult. They can develop rapidly; to others, a heart attack may look like a normal fainting spell. Rarely do all symptoms appear at once; often only one or two can be observed:
- chest pain ;
- feeling of squeezing, constriction, fullness in the chest;
- vague discomfort in the upper body, including shoulders , face ;
- dizziness.
In this case, the patient may feel nausea , sweating, and difficulty breathing. Vomiting may begin. Attacks of pain may become larger or smaller. Without urgent help, the patient eventually loses consciousness, and it is impossible to bring him out of the state of fainting.
First aid for signs of a heart attack
If you seriously suspect a heart attack, seek emergency medical help, sit in a comfortable position, and take an aspirin tablet, chewed thoroughly or dissolved in a small amount of water. As soon as a medical professional arrives, he needs to tell him about all the symptoms and about the aspirin he took.
You should immediately dissolve a nitroglycerin tablet by placing it under your tongue. Then another one after 5 minutes and, if the sensations do not change, the last one. Three doses are enough, no need to take more without a doctor .
It is important to reassure the patient, since angina pectoris may cause panic and a feeling of imminent death. The person loses control of himself, rushes around the room for no reason, and needs to be calmed down.
Preventing another heart attack
Upon discharge, doctors give detailed instructions on lifestyle, nutrition, and physical activity. However, after the condition improves, patients often neglect the recommendations of doctors.
Atherosclerosis develops for many reasons, but it is aggravated by poor diet, bad habits, and excessive physical and mental stress. It is necessary to lead a measured, healthy lifestyle if you are diagnosed with atherosclerosis , angina pectoris , or after infarction .
After your first heart attack, a second one becomes more likely. The prognosis becomes more pessimistic with each case of myocardial tissue damage. Therefore, carefully following all the recommendations of your doctor and strictly adhering to the regimen is important for the rest of your life.
Published in Cardiology Premium Clinic
Prevention of myocardial infarction
Prevention of coronary artery disease and its extreme expression - myocardial infarction - comes down to influencing modifiable risk factors, namely: physical activity, nutrition, body weight, bad habits, blood glucose and cholesterol levels, blood pressure.
After a heart attack, it is important to regularly independently measure blood pressure and heart rate, systematically undergo ECG and EchoCG diagnostics, and take daily medications to prevent the progression of heart dysfunction and recurrence of the disease.
Complications
Complications of myocardial infarction are early and late. As a rule, early complications develop in the first hours of a heart attack during hospitalization or for several days after the attack. The occurrence of complications is significantly influenced by the timeliness of first aid and hospitalization.
The most common early complications include:
- disturbances in the rhythm and conduction of the heart, which in most cases are fatal;
- rupture of the heart muscle;
- development of acute left ventricular failure, which is accompanied by pulmonary edema.
The last stage of left ventricular failure is cardiogenic shock, in which myocardial contractility sharply decreases and the blood supply to all organs is disrupted. The condition is accompanied by a strong drop in blood pressure, a decrease in body temperature, pale skin, difficulty breathing, oliguria, and loss of consciousness. The probability of death with cardiogenic shock is 90%.
Late complications of myocardial infarction:
- early post-infarction angina. A person who has such a complication does not tolerate even the slightest physical activity. Any activity causes squeezing pain behind the sternum. Even simple self-care activities lead to pain. The pain is less severe than during a heart attack itself, but quite painful;
- chronic heart failure, which is accompanied by shortness of breath, edema of the lower extremities, enlarged liver, and the development of chronic left ventricular aneurysm.