In practice, the New York Heart Association (NYHA) classification is often used to assess the severity of heart failure:
I class
— Physical activity is not limited
Class II
— Mild limitation of activity.
The appearance of shortness of breath and weakness after moderate physical activity. Class III
- Marked limitation of activity.
Shortness of breath after minimal physical activity Class IV
- Severe limitation of activity. Symptoms of heart failure at rest
Causes
Acute left ventricular failure is characterized by low cardiac output and reduced (in some cases normal) blood pressure.
Pathology is observed in acute coronary syndrome, myocarditis, mitral and aortic stenosis, etc. The main cause of low cardiac output is insufficient filling pressure of the ventricles of the heart. Pathology with signs of congestion in the lungs usually develops with:
- myocardial dysfunction;
- chronic diseases;
- myocardial infarction;
- acute ischemia;
- valve dysfunction;
- rhythm disturbances;
- tumors of the left heart.
Pathology can also develop when:
- anemia;
- thyrotoxicosis;
- severe forms of arterial hypertension;
- injuries and brain tumors.
Description of left ventricular failure
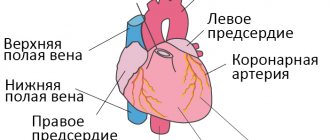
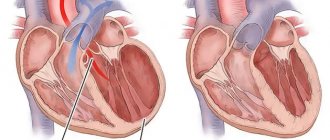
The ventricle, located in the left half of the pumping organ, has a thick muscular wall that allows it to supply blood to the entire body. During diastole, blood from the pulmonary artery enters the left atrium and then fills the left ventricle. Its task is to completely push the oxygen-enriched biological fluid into the aorta (the largest artery) at the moment of systole.
If the myocardium of the left ventricle for any reason loses its contractility, venous blood stagnates in the pulmonary circulatory system (pulmonary circulation), resulting in pulmonary edema. Ineffective blood pumping instantly causes oxygen deficiency in all tissues of the body.
Left ventricular failure has been reported in 0.4-2.0 percent of European residents, and there are 40 million patients with this diagnosis in the world. The pathology is included in the international directory of diseases, its ICD-10 code is I50.1. With age, the likelihood of developing LN increases: it is diagnosed in almost 20% of all hospitalized patients over 65 years of age. Mortality, taking into account etiology, varies between 50-80%. In the rapid course of heart failure, the first and main sign of the disease, as well as a threatening factor, is pulmonary edema.
Classification of the disease
There are 2 forms of heart failure:
- Energy-dynamic. This pathology is associated with metabolic disorders. Usually it occurs in a mild form.
- Hemodynamic. Associated with myocardial fatigue. It is characterized by primary lesions.
There are several stages of pathology:
- First stage. The disease is characterized by initial manifestations. Failure occurs during exercise.
- Second stage. Form A pathology is characterized by shortness of breath, swelling during exercise, and palpitations. Form B is characterized by more pronounced symptoms. They occur not only under load, but also at rest.
- Third stage. At this stage, irreversible changes occur. Liver cirrhosis is often added to the underlying pathology.
Symptoms and stages of the chronic form of the disease
A distinctive feature of the pathology is a systematic violation of the blood ejection regime of the left ventricle. Chronic left ventricular failure leads to constant interruptions in the blood supply to the entire body, congestion in the pulmonary circulation and lower respiratory tract. The patient's condition worsens gradually, each phase of the disease is characterized by its own clinical manifestations.
Stage 1. Shortness of breath and increased heart rate are noticeable during intense physical movements. This sign will be noticed only by trained people who previously reacted calmly to increased loads. For an ordinary person, such a reaction is normal.
Stage 2a. When climbing stairs above the 4th floor, walking for half an hour, or short jogging, a person cannot catch his breath, and a strong heartbeat begins. A dry cough is a constant concern (in the absence of respiratory tract disease caused by infection). Blueness appears on the lips, called cyanosis.
Cyanosis of lips
Stage 2b. In addition to the left ventricular failure, right ventricular failure develops, due to which stagnation of venous blood is already observed in the systemic circulation. Shortness of breath and an accelerated pulse are observed with minor exertion (moving around the house, light housework), and then at rest. Impaired blood flow leads to liver enlargement (pain in the right hypochondrium), cough, cyanosis, and attacks of cardiac asthma. In addition to swelling of the extremities, swelling of the abdominal cavity (ascites) is added. Since the blood supply to the brain suffers, it often hurts and feels dizzy.
Stage 3. All of the above symptoms are most pronounced. The transformations that have occurred in the lungs, heart, and liver become irreversible. It is no longer possible to recover at stage 3.
Symptoms
An attack of insufficiency is accompanied by symptoms of severe suffocation. The patient's skin becomes cold and damp. Breathing is hoarse. Tachycardia also occurs. Blood pressure can fluctuate within fairly wide limits.
As insufficiency progresses, a picture of “classic” pulmonary edema develops. The patient's bubbling breathing can be heard in the distance. The respiratory rate can reach 30-40 per minute. Often a cough with pink sputum appears. Acute pulmonary edema can last 2-4 hours. Subacute conditions are longer lasting. With prolonged pulmonary edema, the patient’s condition does not change from 12 hours to several days.
If the patient delays therapy, the risk of death increases significantly.
Pathogenesis
Pathogenetic mechanisms are associated with a sharp, critical drop in blood pressure and subsequent weakening of blood flow in organs and tissues. The leading factor is not hypotension , but rather a decrease in blood circulating through the vessels in a certain period of time. Compensatory-adaptive reactions are triggered in response to deteriorating perfusion.
The body directs all its reserve reserves to provide nutrition to vital organs: the brain and heart. In this case, skeletal muscles, limbs and skin experience oxygen starvation. In response, peripheral capillaries and arteries spasm. All this leads to activation of neuroendocrine systems, water and sodium ions are retained in the body, and acidosis .
Diuresis may decrease to 0.5 ml/kg per hour or less. Patients are diagnosed with oliguria , anuria multiple organ failure develops . Excessive vasodilation occurs in later stages and is triggered by cytokine and acidosis .
Diagnostics
Primary diagnosis consists of:
- Conducting a patient interview. Be prepared to talk about the severity of the pathology. The specialist will examine the anamnesis and medical history. This will allow us to determine the main causes of the pathology.
- Physical examination. The doctor palpates the area of the right hypochondrium, measures blood pressure and pulse, and listens to the heart.
- Laboratory research. Patients usually undergo blood and urine tests. These studies are carried out to study the condition of various organs and systems of the body.
- Instrumental research. The patient undergoes an ECG, cardiac ultrasound, PET scan, and chest x-ray.
Acute left ventricular failure
Acute left ventricular failure is a serious condition caused by decompensation of heart pathology and requiring emergency medical care. In the structure of mortality of cardiac patients, this disease is the first cause of death. What are the main causes, symptoms, diagnostic methods, how is left ventricular failure treated - information about this is further in the article.
Risk factors
Acute cardiac left ventricular failure occurs as a result of complex pathogenetic mechanisms causing primary hypertension (increased pressure) in the pulmonary circulation. Risk factors for decompensation of severe cardiac pathology are physical or emotional stress, fluid overload of the vascular bed, infections, etc.
The development of heart failure is associated with impaired systolic or diastolic function, which is caused by various reasons. In order to understand the pathogenetic mechanism, one should recall some aspects of the anatomical and functional features of the heart.
The heart is a muscular “pump” that continuously pumps blood through 2 circles of blood circulation – large and small. Acute left ventricular failure occurs when there is difficulty in the functioning of the left sections (atrium and ventricle) of the heart and is caused by overload of the pulmonary circulation (PB).
8
24/7
In a simplified manner, the ICC diagram can be described by the following sequential stages of blood circulation through the cardiovascular system:
- Right ventricle.
- Pulmonary trunk.
- Right and left pulmonary arteries.
- Arteries, arterioles, capillaries of the bronchopulmonary system.
- Venules and veins.
- Left atrium.
Oxygen-enriched blood through the mitral valve, during diastole, enters the left ventricle, and from there in systole, it is pushed into the aorta.
Acute left ventricular failure develops under the influence of such unfavorable factors as:
- cardiac ischemia;
- long-term surgical intervention;
- infections;
- hypertonic disease;
- excess fluid in the body;
- bronchial asthma;
- severe kidney disease;
- taking certain medications;
- congenital and acquired pathology of the valve system;
- diseases of the endocrine system.
Under the adverse influence, backflow occurs, overflow and volume overload of the left atrium and pulmonary vascular bed. This causes swelling of the intercellular spaces, reactive narrowing of the bronchial lumen, and foaming of the protein contents of the alveoli. All this leads to the development of a clinical picture of cardiac asthma and pulmonary edema.
Causes
The causes of acute left ventricular failure are cardiac (heart) and non-cardiac in nature. The reasons causing the development of this pathology include:
- chronic heart failure in the decompensation phase;
- myocardial infarction;
- aortic dissection;
- cardiac tamponade;
- infection of arteries and valves;
- severe acute myocarditis;
- arrhythmia attack;
- hypertensive crisis.
Factors that do not affect the anatomical structures of the heart, but significantly affect its work with the development of failure, include:
- violation of treatment tactics (overdose of drugs, non-compliance with the rhythm and frequency of taking medications);
- fluid overload (especially with intravenous infusions);
- alcohol abuse;
- tumor of the adrenal cortex (pheochromocytoma);
- renal failure;
- severe lung pathology (bronchial asthma, COPD, pneumonia, tuberculosis);
- stroke;
- sepsis.
In addition, conditions such as severe anemia and thyrotoxic crisis cause increased cardiac output syndrome, which also negatively affects the condition of the left ventricle.
8
24/7
What happens
Acute left ventricular failure, according to the etiological factor or origin, can be primary and an exacerbation of chronic failure. Primary heart failure is caused by:
- acute nephritis (inflammation of kidney tissue);
- acute myocardial infarction;
- hypertensive crisis.
And among the acute manifestations of chronic left ventricular failure are:
- mitral heart defects;
- defects of aortic origin;
- blood stagnation in the ICC in chronic heart failure;
- left ventricular aneurysm.
According to the clinical course, according to the new recommendations of the Society of Cardiology, heart failure (HF) can be:
- acute decompensated (newly occurring, exacerbation of chronic HF);
- hypertensive – symptoms of heart failure are combined with arterial hypertension;
- pulmonary edema;
- cardiogenic shock;
- HF combined with high cardiac output (more often with infections).
When taking into account the clinical course together with radiographic data, acute HF is divided into 4 degrees of severity:
- There are no clinical signs of heart failure.
- The appearance of symptoms and radiological signs consistent with cardiac asthma.
- Detailed picture of pulmonary edema.
- Cardiogenic shock with a drop in blood pressure.
Based on systematic observation of the clinical course, depending on the volume of blood ejected by the left ventricle, left ventricular HF with high or low cardiac output is distinguished.
Symptoms
At the moment when acute left ventricular failure develops, assistance should be provided according to the clinical variant, each of which has its own characteristics.
Precursors and acute forms of left ventricular failure manifest themselves in the form of:
- increased or onset of shortness of breath;
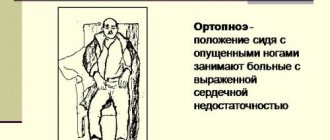
- forced body position (orthopnea), which alleviates the condition;
- rawness behind the sternum during physical activity;
- cough when changing body position;
- the appearance of wheezing in the lower parts of the lungs.
With stagnation in the pulmonary vessels and their increased tension, fluid leaks from the bloodstream into the intercellular tissue (interstitium). It is interstitial pulmonary edema that underlies the development of cardiac asthma, which has the following clinical manifestations:
- nocturnal asthma attack;
- shortness of breath accompanied by chest pain;
- orthopnea;
- participation of auxiliary muscles in breathing;
- sticky, cold sweat on the face and chest;
- cyanosis (blue discoloration) of the nasolabial triangle, lips, neck, fingertips;
- dry and moist wheezing in the lungs;
- pulse is rapid and arrhythmic.
If help is not provided or treatment is ineffective, the following type of manifestation of left ventricular failure develops - pulmonary edema, which is characterized by symptoms such as:
- suddenness of occurrence;
- bubbling breathing;
- feeling of fear of death;
- moist rales heard at a distance;
- discharge of white-pink frothy sputum;
- Moist rales are heard over all the lungs.
If acute left ventricular failure develops, pulmonary edema must be stopped immediately, since severe respiratory failure leads to acute oxygen starvation of the entire body. This is a critical condition that leads to death in a short time.
8
24/7
Diagnostics
The basis of diagnostic measures aimed at confirming the diagnosis is the collection of objective data, especially auscultatory data (when listening to the lungs with a stethoscope).
The following additional laboratory and instrumental methods are used:
- electrocardiography;
- chest x-ray;
- ECHO-cardioscopy with Dopplerography;
- blood chemistry;
- study of blood gas composition;
- general blood and urine tests;
- study of the coagulation system and D-dimer.
When recording an ECG, a number of characteristic changes are revealed that confirm decompensation of the pathological condition. On the cardiogram, changes in the isoline are recorded in the leads corresponding to the damage.
X-ray allows you to assess the presence and extent of damage to the lung tissue, displacement of the cardiac border, enlargement or displacement of the borders of the heart and mediastinum.
ECHO cardioscopy is performed using an ultrasound sensor with the function of measuring the speed and volume of blood flow through the vessels (Doppler). This study helps to visualize the site of damage, the valve apparatus, measure the volumes of the heart chambers, the thickness of the heart walls, the speed and magnitude of blood flow, and ejection fractions.
A biochemical blood test involves the identification and quantitative assessment of substances that are markers of acute cardiac pathology. Among the biochemical indicators, total protein, ALT and AST, creatine phosphokinase, haptoglobin, creatinine, potassium, sodium, urea, and sugar are taken into account.
Blood gases allow you to determine the degree of decrease in oxygen in the blood and increase in carbon dioxide. The criteria for these indicators reflect the severity of hypoxia – oxygen starvation and help monitor the patient’s condition and the effectiveness of therapeutic measures.
Treatment at different stages
If acute left ventricular failure develops, emergency care should be provided even before the ambulance arrives. The algorithm of actions is as follows:
- Call an ambulance.
- Position the patient in a semi-sitting position.
- Provide access to fresh air.
- Unbutton your shirt collar and loosen your belt.
- If possible, calm down, give Valoserdin, Valocardin, Corvalol to drink.
- Measure and record blood pressure and pulse, do this every 10 minutes.
- When systolic (upper) pressure is above 100 mm Hg. suggest dissolving a Nitroglycerin tablet under the tongue.
- Apply tourniquets to the thighs (15-20 cm below the inguinal fold), loosen them every 15 minutes.
- If you lose consciousness, place yourself in a safe position on your side.
- Clear your mouth of foam.
- If there is no breathing or heartbeat, begin chest compressions and artificial respiration.
Acute left ventricular failure, the treatment of which must be carried out in an intensive care unit or resuscitation room, is an absolute indication for hospitalization in a cardiological or therapeutic hospital.
Therapeutic measures aimed at relieving this pathological condition include methods such as:
- oxygen therapy - inhalation of heated, humidified oxygen through a mask or nasal cannulas, for pulmonary edema, passed through an antifoam agent - ethyl alcohol;
- administration of narcotic analgesics (Morphine), which provide a sedative (calming) and analgesic effect;
- intravenous administration of Nitroglycerin;
- use of diuretics (Lasix, Furosemide, Ethacrynic acid);
- prescription of cardiac glycosides (Strophanthin, Korglykon, Digoxin);
- cardioversion – used for atrial flutter or fibrillation.
For successful treatment of acute HF caused by non-cardiac pathology, it is important to establish and eliminate the cause that causes it. With continued exposure to a negative factor, therapeutic measures turn out to be ineffective, which leads to rapid death.
Forecast
The prognosis for this disease is rarely favorable, and despite the achievements of modern resuscitation, pulmonary edema is very often the cause of death. The forecast largely depends on the following factors:
- etiology of the development of heart failure (acutely occurring or decompensation of chronic heart failure);
- the extent of damage to the cardiac structure due to cardiogenic causes;
- possibilities for rapid relief of non-cardiac causes of heart failure (pneumonia, sepsis, thyrotoxic crisis);
- age;
- the presence of concomitant pathology.
Left ventricular failure, which occurs as a transient condition, has a more favorable prognosis, which depends on the volume and timeliness of medical intervention. Often acute heart failure is accompanied by massive damage to the heart and becomes chronic.
Disease prevention
The basis for preventing the development of acute left ventricular failure is a commitment to strict adherence to doctor’s prescriptions. It is important to exclude all provoking factors that contribute to damage to the cardiovascular system.
Measures to prevent heart disease include the following:
- to give up smoking;
- avoiding the consumption of alcoholic beverages;
- compliance with diet therapy (limiting cholesterol-rich foods, fatty, fried, canned foods, coffee, confectionery, animal fats);
- performing feasible physical exercises daily (jogging, yoga, Nordic walking, swimming);
- exclusion of stressful situations and neuro-emotional experiences;
- limiting physical overexertion.
8
24/7
Acute left ventricular failure is based on cardiac and non-cardiac causes, which cause hypertension in the pulmonary circulation. The main manifestations of the pathology are cardiac asthma and its complication – pulmonary edema. Timely provision of emergency and specialized care for acute heart failure affects the prognosis of the disease.
Treatment
During an attack, it is necessary to provide the patient with timely assistance.
- The person should be seated on the bed, ensuring sufficient air flow.
- Oxygen therapy is necessary.
- The patient should be given nitroglycerin.
When pulmonary edema develops, doctors must administer prednisolone. After stopping the attack, all patients are subject to mandatory hospitalization.
Drug therapy is provided in the hospital.
It consists in:
- normalization of myocardial contractility;
- preventing the formation of blood clots and the risk of blocking blood vessels;
- elimination of sinus tachycardia;
- normalization of fluid removal processes.
Oxygen therapy is mandatory. Diuretics are used to remove fluid. The patient is limited in fluid intake. To reduce vascular resistance and improve blood circulation, antiplatelet agents and vasodilators are prescribed. To enhance myocardial contractility, patients take cardiotonics and cardiac glycosides.
Important! All medications can only be prescribed by a doctor. Medicines are selected individually. The doctor takes into account the patient’s condition, the presence of other diseases, and previous pathologies. Self-therapy is very dangerous! It can be fatal.
When treating left ventricular failure, an integrated approach is very important.
Patients are prescribed:
- Complete peace.
- Diet.
- Refusal of any physical activity.
When are surgical interventions performed?
Surgeries are prescribed if drug therapy does not alleviate the patient’s condition.
Today there are 2 types of interventions:
- Implantation of a device that improves blood circulation.
- Cardiomyoplasty.
Both interventions are life-threatening. Therefore, they resort to them only in emergency cases. It is also important that rehabilitation after interventions is very long. Recovery usually takes 3-4 months.
Do you want to receive quality treatment and avoid difficult and dangerous interventions? Contact our clinic! After a thorough diagnosis, during which each symptom of the pathology will be studied, the specialist will prescribe adequate therapy.
You won't have to overpay for it. We adhere to a loyal pricing policy. Approximate prices for specialist consultations and examinations are indicated on the website. Our medical center (Moscow) is open to all clients! The exact price for specific examinations and consultations will be announced by specialists over the phone. The cost of the entire therapy complex will be calculated by a specialist during the first appointment. This will allow you to plan your expenses.
First aid for AHF
A patient with AHF must immediately receive emergency care, since cardiogenic shock may occur during a heart attack. At the same time, his skin turns pale, his blood pressure drops sharply, severe pain appears, and his pulse is practically not palpable. If you do not respond in time, swelling of the kidneys and lungs can quickly develop, which can lead to death.
In case of AHF, first aid is provided at the scene of the incident, while it is necessary to reduce the load and ensure the redistribution of blood flow by performing the following actions:
- Place the patient in a comfortable sitting position; to do this, lower his legs to the floor and raise his back.
- It is better to immerse your feet in a basin of hot water, reducing the flow of blood to the heart.
- Remove the patient from clothing and open the windows, ensuring maximum flow of fresh air.
- Call emergency doctors and report the symptoms of an attack.
- Apply a tourniquet in the groin area to each leg alternately (20 minutes), which will reduce the flow of blood into the myocardium.
- Provide the patient with emotional and physical peace; he is strictly forbidden to get up and walk.
If there are signs of AHF, you need to measure your blood pressure. If the upper reading is more than 90 mmHg, then 1 tablet of nitroglycerin should be placed under the patient’s tongue. After this, you need to monitor the pressure all the time. If necessary, you can give 1 more tablet after 7 minutes, but not more than 4 times.
Patients suffering from heart disease or hypertension with severe swelling of the legs and shortness of breath should always carry a first aid kit with medications prescribed by the attending physician. Then, at the first signs of AHF, people around you will be able to provide emergency assistance.
Prevention
To prevent left ventricular heart failure, a number of recommendations should be followed:
- Give up bad habits: smoking and drinking alcohol.
- Follow your diet. Minimize the amount of salt you consume and avoid animal fats, spicy, fatty and fried foods.
- Be careful with any physical activity. They should be moderate.
- Maintain an optimal weight.
- Maintain your blood pressure levels. If your blood pressure rises, consult your doctor immediately. He will prescribe medications that will help relieve a disease such as arterial hypertension.
- Promptly treat all pathologies that can provoke left ventricular heart failure.
- Avoid stressful situations.
- Get regular check-ups with a cardiologist. It will allow timely detection of pathologies that can lead to the development of deficiency.
Secondary prevention consists of preventing the development of attacks of insufficiency. Be sure to take all prescribed medications on time and in the required dosage, and consult your doctor if your condition changes.
Forecast
Left ventricular failure allows for a favorable prognosis only at the onset of the disease and with timely treatment. Only in this case can the development of irreversible disorders in the heart be prevented. The acute form of the disease significantly worsens the prognosis, since it contributes to the destruction of not only the heart muscle, but also other internal organs.
Surgical operations help to significantly increase a patient’s life expectancy, but they require a long rehabilitation period to restore body functions.
Did you like the article? Save it!
Still have questions? Ask them in the comments! Cardiologist Mariam Harutyunyan will answer them.
Ivan Grekhov
Graduated from the Ural State Medical University with a degree in General Medicine. General practitioner