Cardiopulmonary failure is a decompensated stage of cor pulmonale, which occurs with acute or chronic right ventricular heart failure. The occurrence of pathology is associated with impaired blood circulation in the vessels of the lungs, which is accompanied by a decrease in blood oxygen saturation.
There are two main forms of cardiopulmonary failure - acute and chronic. The acute form in most cases occurs as a result of asthma, emphysema or massive thromboembolism. Clinical signs appear several hours after a sharp increase in arterial pressure. The chronic form is characterized by slow development with an increasing clinical picture (it can develop over several months or years).
There are several types of cardiac pulmonary failure, which differ in their characteristic symptoms. Among them: cerebral, anginal, respiratory, abdominal and collaptoid type of pathology. The cerebral type is characterized by signs of encephalopathy (for example, drowsiness and lethargy or, on the contrary, excitability and aggressiveness). Some patients complain of headaches and dizziness.
The anginal type is characterized by the appearance of severe pain in the area (with no irradiation) and a feeling of lack of oxygen. The progression of the respiratory type is accompanied by the appearance of shortness of breath, cough and cyanosis of the skin. The abdominal type is characterized by painful sensations and a feeling of nausea. Without further treatment, stomach ulcers may occur. The collaptoid type is accompanied by a persistent increase in blood pressure, tachycardia and general weakness. In this case, patients experience pallor of the skin.
Circulatory failure depends on two main factors: a decrease in the contractile force of the muscular membrane of peripheral vessels and a decrease in the contractility of the muscular organ. If the first factor significantly predominates, then we are talking about vascular circulatory failure, and if the second predominates, we are talking about chronic heart failure.
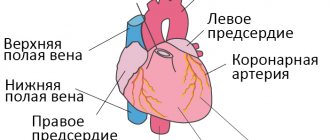
The left and right sections of the muscular organ are responsible for blood circulation. When one of these sections is damaged, isolated or predominant lesions appear, respectively, on the left or right half of the muscular organ. Based on this, left ventricular failure and right ventricular failure are distinguished.
From an anatomical and functional point of view, the lungs and heart have a close relationship. This explains the fact that when one organ is damaged, negative consequences subsequently affect the other. Depending on which of these organs is more affected, pulmonary-cardiac and cardiopulmonary failure are distinguished.
There are two main phases – compensation and decompensation. In the compensation stage, the muscular organ is able to cope with its load and work. But this does not always happen: over time, a period comes when its internal reserves are completely exhausted, resulting in a decompensation phase. In this phase, the muscular organ is no longer able to cope with the load.
First aid for pulmonary edema
Unlike the chronic form, the acute form of the pathology requires immediate assistance during an attack. A person is not able to help himself, so he needs help from the outside. First of all, you should call an emergency team. While waiting for her, the person should be seated on a chair and given a Nitroglycerin tablet. If the attack occurs indoors, be sure to open all windows to provide fresh air flow.
If a person gets worse, cardiopulmonary resuscitation methods are required. To do this, rhythmically press on the chest area or do 30 presses and mouth-to-mouth breathing (alternating these actions). The main goals of these measures are to normalize blood circulation and restore respiratory function. If you lack the skills, you can simply massage the sternum.
What awaits patients
Half of all patients diagnosed with heart failure live more than five years. It is difficult to talk about maximum life expectancy; this indicator is determined by many factors. These include the severity of the disease, concomitant background, and the effectiveness of the prescribed treatment. The kind of life the patient leads and much more is of great importance.
If the disease is detected in the initial stage, with the help of therapy the patient’s condition can be completely compensated. At stage 3 of the disease, experts talk about a worse prognosis.
Causes of cardiopulmonary failure
Cardiopulmonary failure never occurs without a reason. As a rule, several reasons lead to its development. There are three main groups of causes that can provoke pathology:
1. Bronchopulmonary diseases. According to statistics, they act as a provoking factor in more than 70% of all cases. Among the most common diseases are bronchial asthma, pulmonary tuberculosis, chronic bronchitis and other severe disorders of the respiratory system (for example, cystic fibrosis).
2. Thoradiaphragmatic diseases. They are directly related to pronounced deformation of the chest and limited mobility of the diaphragm. The appearance is caused by severe curvatures of the spinal column (in particular, kyphoscoliosis), ankylosing spondylitis, and restrictions on the expansion of the lungs (pleuritis).
3. Vascular diseases. This group includes diseases that affect lesions of the pulmonary bed. These include sickle cell anemia, pulmonary vasculitis, compression of the pulmonary veins and arteries by neoplasms.
4. Vascular diseases. Often, the development of cardiopulmonary failure is provoked by aneurysms, atherosclerosis and blood clots in the arteries of the lungs.
Reasons for development
Chronic heart failure occurs against the background of other diseases that affect the myocardium and blood vessels. Therefore, it is always necessary to treat or keep primary diseases under medical supervision, as well as monitor the condition of your circulatory system.
Factors in the development of CHF
- Arterial hypertension (AH) is the main cause of chronic heart failure.
- Coronary heart disease (CHD) is in second place among the provoking factors.
- Cardiomyopathies (including those provoked by infectious diseases, diabetes mellitus, hypokalemia, etc.).
- Valvular (mitral, aortic, tricuspid, pulmonary) and congenital heart defects.
- Arrhythmias (tachyarrhythmias, bradyarrhythmias).
- Diseases of the pericardium and endocardium.
- Conduction disturbances (antrioventricular block).
- High load (for example, with anemia).
- Volume overload (eg, renal failure).
The course of any disease from the list above should be monitored by the attending physician
Diagnosis of pathology
The diagnosis of cardiopulmonary failure is established based on the results of a comprehensive examination. During the initial examination, the doctor collects anamnesis (listens about symptoms, chronic pathologies in the patient and immediate family), performs a visual examination (possible swelling of the feet and legs), conducts a physical examination and standard measures (measuring blood pressure, listening to breathing using a phonendoscope). Upon palpation, a cardiac impulse is detected, and upon percussion, an expansion of the boundaries of the region of the muscular organ, which is partially covered by the lungs, is detected.
Among the laboratory diagnostic methods for making a diagnosis, an analysis of the gas composition of arterial blood is required. If there are problems, patients experience a decrease in P02 and SAO2 P02, and an increase in PC02. Additionally, a general blood test is prescribed to detect an infectious process in the body (by increasing the level of leukocytes). The most informative ways to detect cardiopulmonary failure are instrumental diagnostic methods. Depending on the symptoms, the patient may be prescribed:
- study of respiratory function (external respiration function). With the help of this examination, it is possible to establish the nature and severity of pulmonary ventilation impairment;
- electrocardiography (ECG). This is an accessible method that does not require additional preparation from the patient. The essence of electrocardiography is to record the electrical potentials of a muscle organ, which makes it possible to detect changes in rhythm and electrolyte deficiency. If the disease occurs in an acute form, it is possible to detect signs of overload in the right parts of the muscular organ. If the disease is chronic, it is possible to detect markers (both direct and indirect) of right ventricular hypertrophy;
- echocardiography (EchoCG). It is often prescribed in addition to an ECG, since the information content of this examination regarding cardiopulmonary failure is very high. This is the main non-invasive method with which it is possible to assess intracardiac hemodynamics, determine the size of the cavities of the muscular organ and the degree of pulmonary hypertension. EchoCG allows you to detect a number of possible disturbances in the functioning of the heart, differentiate it from heart disease and other pathologies;
- chest x-ray. This is a simple technique with which it is possible to assess the condition of the respiratory system (detect damage to the internal organ and notice signs of pulmonary hypertension);
- transbronchial lung biopsy. These methods are rarely resorted to, in particularly advanced clinical cases. A puncture biopsy of the lung is performed under ultrasound or X-ray guidance using a local anesthetic.
Treatment
Insufficiency therapy is carried out comprehensively and depends on:
- underlying disease;
- general condition of the patient;
- concomitant pathologies and other factors.
For pulmonary embolism, for example, the following is carried out:
- oxygen therapy;
- pain relief;
- thrombolytic therapy.
In some cases, the only effective way to get rid of the pathology is thromboembolectomy from the pulmonary artery.
If the deficiency has developed against the background of bronchopulmonary pathology, the following are used:
- mucolytics;
- bronchodilators;
- expectorants.
For pulmonary tuberculosis, therapy is carried out using antibiotics.
For specific lung diseases, interferon, cytostatics and glucocorticoids are used.
At all stages, therapy is carried out using oxygen inhalation. Vasodilators are prescribed to reduce pulmonary vascular resistance. For swelling, diuretics are additionally indicated. They allow you to restore water and electrolyte balance.
If drug therapy does not give the desired result, surgical interventions are performed.
Today specialists carry out such operations as:
- balloon septostomy;
- reduction of lung tissue;
- sympathectomy.
In the most advanced cases, a lung or lung and heart transplant may be required.
All operations are quite complex and lengthy. That is why endovascular techniques are being actively developed and implemented today. They make it possible to reduce trauma and the duration of rehabilitation, and create the opportunity for patients to recover even in difficult situations.
Of course, in case of any pulmonary or cardiac pathologies, specialists will try to eliminate them with the help of medications and the most minimally invasive interventions possible. Our doctors use all known modern techniques. Particular attention is paid to the prevention of pathologies. Of course, several specialists are involved in working with the patient at once. This allows you to find the optimal solution even in difficult situations.
Prices for therapy depend on a lot of factors, but we never inflate them. Thanks to this, you can benefit from professional support even on a limited budget. The exact price of therapy at a clinic in Moscow will be announced in advance. This will allow you to plan your expenses.
Disease prevention
In order to prevent pathology, all risk factors that can provoke it should be eliminated. If any negative symptoms appear, it is important to consult a doctor in order to promptly diagnose and treat lung or heart disease. Also, experts recommend leading a healthy lifestyle (not smoking or drinking alcohol), engaging in moderate physical activity and eating right. The diet should be balanced with a predominance of fresh vegetables and fruits.
In order to prevent the development of acute cor pulmonale, patients diagnosed with varicose veins and atrial fibrillation are prescribed indirect anticoagulants. If there are blood clots in the veins, a vena cava filter is often installed. It is a small device that is installed into the lumen of the inferior vena cava. With its help, detached blood clots do not enter parts of the heart muscle and the pulmonary artery system.
What are the types of heart failure and what are their symptoms?
Each type of heart failure has different symptoms, and the symptoms can vary in intensity. However, the main symptom of heart failure is difficulty breathing during exercise or at rest. Warning signs may include sweating with mild exercise, an inability to lie flat, tightness in the chest, or swelling in the legs.
Left-sided heart failure
The left side of the heart is responsible for pumping oxygen-rich blood throughout the body to the organs. In left-sided heart failure, the pumping function of the left ventricle is limited, resulting in insufficient oxygenated blood to be pumped throughout the body. Instead, the blood remains in the pulmonary circulation, which can lead to fluid in the lungs (pulmonary edema), difficulty breathing, throat irritation, a rattling sound when breathing, weakness, or dizziness.
It is most often caused by coronary artery disease (CHD), high blood pressure or a heart attack, and less commonly by problems with the heart muscle or heart valves.
Left-sided heart failure may present acutely or develop over time. It is usually first noticed by shortness of breath from physical activity. When severe, it can even lead to hypotension (low blood pressure) at rest.
Right-sided heart failure
The right side of the heart is responsible for returning low-oxygen blood back to the lungs. In right-sided heart failure, the right ventricle does not work properly. This causes increased pressure in the veins, forcing fluid into the surrounding tissue. This leads to swelling, especially in the feet, toes, ankles and legs. This can also lead to an urgent need to urinate at night when the kidneys receive better blood circulation.
The cause is most often an acute or chronic increase in pulmonary circulatory resistance. Caused by pulmonary diseases such as pulmonary embolism, asthma, severe emphysema, chronic obstructive pulmonary disease (COPD, most commonly due to tobacco use), or left-sided heart failure. Rare causes include heart valve problems or heart muscle disease.
Global heart failure
When both the left and right sides of the heart are affected, it is called global heart failure. There are symptoms of left and right heart failure.
Systolic and diastolic heart failure
Systolic heart failure is associated with loss of normal functioning of heart muscle cells or external impairment of pumping function. Blood enters the lungs, and the organs do not receive enough oxygen.
In diastolic heart failure, the elasticity of the ventricle is lost, causing it to not relax and fill appropriately. One of the most common causes of diastolic dysfunction is high blood pressure. Due to increased resistance in the arteries, the heart must work harder. The elasticity of the heart muscle decreases, and less blood can be pumped from the ventricles to the body between contractions. This results in the body not receiving enough blood and nutrients.
Heart valve disease can also cause the heart muscle to thicken. The heart muscles become stiffer and less elastic due to the accumulation of proteins. Symptoms range from cough to shortness of breath.
Chronic and acute heart failure
Chronic heart failure is a progressive disease that takes months or years to develop and is more common than acute heart failure. In chronic heart failure, symptoms are often not taken seriously because the body is able to compensate over a long period of time or symptoms are associated with increasing age. Symptoms reflect either left- or right-sided heart failure.
Acute heart failure occurs suddenly, minutes or hours after a heart attack, when the body can no longer compensate. Some symptoms include:
- severe difficulty breathing and/or coughing;
- Gurgling sound when breathing;
- Heart rhythm disturbances;
- Pallor;
- Cold sweat.
Preventive measures
For preventive purposes, to prevent the occurrence of such a disease, it is necessary to prevent the development of diseases that lead to it. Among them is ischemia, hypertension, heart defects. In addition, it is necessary to prevent as much as possible the emergence of factors that favor the appearance.
If you have heart failure, the symptoms of which have already appeared, you must first of all try to prevent its progression. To do this, you should not exceed the recommended physical activity, take all medications prescribed by your doctor, and be regularly examined by a cardiologist. The doctors of the Clinical Hospital “RZD-Medicine” in Nizhny Novgorod will help you monitor your health.
OTHER INFORMATION
Please note that if our company (or any part thereof) is sold or placed into receivership, information we hold may be part of the assets transferred; however, such information will continue to be used solely in accordance with the terms of the Policy on the processing and protection of personal data.
For quality control or training purposes, we may monitor or keep a record of your correspondence with us.
•Policy of AstraZeneca Industries LLC in the field of processing and ensuring the security of personal data • Policy of AstraZeneca Pharmaceuticals LLC in the field of processing and ensuring security of personal data
Nutrition and daily routine
Meals should be fractional: 5-6 times a day in small portions. Limit the consumption of meat, salt, exclude smoked foods, chocolate, and alcohol. To replenish their strength, patients should eat foods high in potassium: buckwheat and oatmeal, bananas, dried apricots, Brussels sprouts, etc. A protein and vitamin diet is prescribed.
The daily routine depends on the form of the disease. In the acute form, only rest is necessary. In chronic cases, on the contrary, rest is contraindicated. The patient is advised to exercise in moderation, and a special system of exercises is developed to prevent the disease.
Clinical manifestations
The syndrome usually develops suddenly
The clinical picture of AHF is always accompanied by a decrease in blood pressure and directly depends on the severity of the condition; this is presented in more detail in the table.
Table 1. Clinical forms of pathology
| Name | How does it manifest clinically? |
| Fainting woman fainting | The patient suddenly feels weak, dizzy, and has “floaters” flashing before his eyes. Consciousness may be preserved or absent. If after 5 minutes the patient does not come to his senses, then fainting is accompanied by convulsions; as a rule, this rarely happens and with properly organized help the person’s condition quickly normalizes |
| Collapse Retardation during collapse | This condition is much more severe than fainting. The patient's consciousness can be preserved, but there is severe inhibition and disorientation in space. Blood pressure is sharply reduced, the pulse is weak and thready, breathing is shallow and rapid. The skin is pale, acrocyanosis and sticky cold sweat are observed. |
Shock State of shock | Clinically, shock is not much different from collapse, but in this condition a sharp depression of the heart and other vital organs develops. Due to severe hypoxia, the brain suffers, against the background of which degenerative changes can develop in its structure |