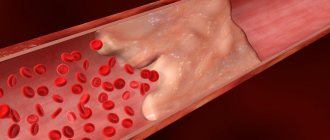
Arterial embolism is the transfer of a blood clot (embolus) from the central parts of the bloodstream through an artery, which gets stuck in some of its branches and can block or limit blood flow. Emboli typically block blood flow to an arm or leg. Embolism is a very dangerous disease, since a sudden cessation of blood flow below the site where it is stuck causes acute circulatory failure and leads to the death of an organ or part of the body.
One clot can cause more than one embolism if it breaks into pieces and is carried further down the artery by the bloodstream. Embolism requires immediate treatment, as irreversible damage to the affected organ or limb can develop in a short time.
Causes of arterial embolism
A number of diseases can lead to arterial embolism. The most common cause of embolism is atrial fibrillation, when the atria do not contract, causing blood stagnation and the formation of blood clots. At some point, a fragment of this thrombus breaks off and is carried through the bloodstream to some organ, blocking blood flow in it and causing acute ischemia.
Other less common causes of blood clots and embolism include:
- Arterial aneurysms (pathological expansion of the diameter of the vessel)
- Artery injury
- Hypertensive crisis, with dissection of a section of the artery and the formation of a blood clot
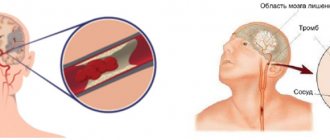
Ischemic stroke by the mechanism of paradoxical embolism
One of the possible mechanisms of IS in young patients is paradoxical embolism (PE) - migration of a thrombus (rarely air or fat) from the venous system through an open foramen ovale, atrial septal defect or pulmonary arteriovenous malformations with subsequent embolism in the branches of the aortic arch, which is clinically manifested as transient ischemic attack (TIA) or ischemic stroke [3].
Patent foramen ovale (PFO) is most common in the population (about 25%) and is regarded as the dominant path of PE [4]. Among people who have suffered a cryptogenic stroke, the probability of identifying PFO is 3 times higher than among patients with an established cause of stroke [5].
LLC is a form of interatrial communication, anatomically representing a “probe” hole located in the central part of the interatrial septum (AS), which is formed from the overlapping parts of the primary and secondary septa. The LLC is a rudiment of the normal blood circulation of the embryo; normally it should close by the first year of the child’s life, but remains open in ¼ of the population.
Morphological variability concerns both the size and shape of the oval window - from a simple opening covered by a flap to a long winding passage [6]. The structure of the LLC determines the degree of shunt blood flow passing through the opening, which can vary from small to significant. The combination of PFO with hypermobility and aneurysm of the right atrium promotes the opening of the foramen ovale with each cardiac cycle and increased shunt blood flow, especially with increased pressure in the right atrium (Valsalva maneuver), thereby increasing the likelihood of developing paradoxical embolism.
Another way to perform PE is through atrial septal defects (ASDs). The most common of them are ASDs of the ostium secundum type (secundum septum defects), located in the middle part of the ASD in the area of the fossa ovale. As a rule, the risk of PE is associated with small, hemodynamically insignificant ASDs that do not lead to overload of the right side of the heart and pulmonary hypertension and are detected in adulthood during ultrasound examination of the heart in the process of determining the cause of a stroke. According to Hoffman and colleagues, the incidence of stroke in patients with ASD is 4% among people with congenital heart defects [7].
A rare way of implementing PE is pulmonary arteriovenous malformations (PAVM) - pathological communications between the pulmonary arteries and veins, bypassing the capillary bed, bypassing the process of filtration and oxygenation of blood. The incidence of PAVM in the population is 0.03%. Synonyms for this name in the literature are: pulmonary arteriovenous fistulas/aneurysms. Most PAVMs are congenital and in the vast majority of cases (47-90%) are associated with hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber disease) [8].
Mechanism of paradoxical embolism
The main sources of thrombosis are the veins of the lower extremities, often the deep veins of the legs, and the veins of the small pelvis. Less commonly, thrombosis occurs in situ in the oval window tunnel or in the area of the atrial septal aneurysm, as well as as a result of atrial arrhythmias.
Factors contributing to thrombus formation are:
- Recent immobilization (long travel or flight, immobilization due to illness).
- The presence of genetic markers of thrombophilia - homo- or heterozygous mutations in the gene of factors II and V (Leiden mutation), in the fibrinogen gene.
- Antiphospholipid syndrome.
- Insufficient indicators of the anticoagulant system and fibrinolysis - deficiency of protein C, S, antithrombin III.
- An increase in factor 8 in combination with an increase in the activity of von Willebrand factor.
- Taking oral contraceptives in women, natural prothrombotic states (pregnancy, early postpartum period) [9].
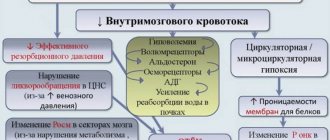
Current of NMC
Features of cerebrovascular disorders include the young age of patients who do not have concomitant pathology from the cardiovascular system. When analyzing the cause of a stroke, it is important to take into account the development of the disease. PE is characterized by the acute development of symptoms in the daytime or immediately after waking up, during or after a long trip (flight). A history may indicate recent thrombosis of the leg veins or pulmonary embolism (PE), the presence of migraine with aura, or sleep apnea syndrome.
The Valsalva maneuver is characterized by forced expiration with the epiglottis closed, when there is an immediate increase in pressure in the right side of the heart and an increase in shunt blood flow. The presence of a Valsalva maneuver at the onset of the development of stroke symptoms increases the likelihood of PE, therefore, when collecting an anamnesis, it is necessary to pay attention to factors such as heavy lifting, straining during bowel movements, coughing, sneezing, laughter and vomiting.
RoPE scale
The Risk of Paradoxal Embolism (RoPE) score was created to help clinicians assess the relationship between cryptogenic stroke and patent foramen ovale. The scale is easy to use - one point is awarded for the absence of vascular risk factors, one point for the presence of IS of cortical localization according to the results of neuroimaging, and one point if a real stroke or transient ischemic attack is new. The younger the patient, the more points he is assigned. A high total score on the scale indicates a high probability of a relationship between PFO and cryptogenic stroke [10].
Neuroimaging
Neuroimaging of the brain is characterized by the detection of cortical or cortical-subcortical infarcts of small or medium size. Particularly suspicious for PE are infarcts located within different vascular territories – carotid and/or vertebrobasilar. Along with “acute” foci of ischemia, the presence of “silent” cerebral infarctions is possible.
Ultrasound diagnostics
Ultrasound methods are the main ones for identifying interatrial communications and assessing shunt blood flow. Transthoracic (TT-EchoCG) and transesophageal (TE-EchoCG) echocardiography are used to visualize structural abnormalities of the heart. TE-EchoCG is a more sensitive method, as it allows you to visualize in detail the area of the oval fossa and detect even small defects in it [11]. To identify shunt blood flow, the most informative method is contrast transcranial Doppler ultrasound (TCDS) with embolodetection. In the presence of a right-to-left shunt associated with PFO, it has been shown to have a sensitivity of 70–100% and a specificity of more than 95% [12].
The technique is carried out according to a standardized protocol accepted in the world: two ultrasound sensors installed on a head helmet monitor blood flow in both middle cerebral arteries. Next, a contrast agent is injected into the patient’s cubital vein, which is a shaken mixture of 9 ml of 0.9% saline solution and 1 ml of air. The appearance of microembolic signals in the blood flow spectrum at rest and during the Valsalva maneuver is monitored. The test is an obligatory component of the study, leading to a sharp short-term increase in pressure in the right atrium and the reflux of contrast bubbles into the left atrium, which is important for the functioning of both poorly visualized small and significant left-to-right shunts. After counting microemboli, the degree of shunt blood flow is determined. Significant for paradoxical embolism is the presence of a shunt of medium (>20 microembolic signals (MES)) or large (“curtain” of MES, where a single signal cannot be recognized in the spectrum) size [11].
Treatment
In 2021, European guidelines for the management of patients with patent foramen ovale were presented [13]. For secondary prevention, patients with cryptogenic ischemic stroke and PFO, depending on the clinical situation, are recommended to use drug therapy with antiplatelet agents or anticoagulants and/or endovascular closure of the defect using a special device - an occluder.
Data from randomized controlled trials in recent years suggest that PFO closure effectively reduces the risk of recurrent stroke for a certain category of patients with cryptogenic stroke. Thus, endovascular PFO closure is indicated for patients under 60 years of age in whom PFO is associated with an aneurysm or hypermobility of the quadrant, as well as a large or medium-sized shunt.
After percutaneous closure of the foramen ovale, it is recommended to take dual antiplatelet therapy (acetylsalicylic acid 75 mg/day + clopidogrel 75 mg/day) for three months, with further transition to long-term therapy with aspirin (75 mg/day). For patients with cryptogenic stroke and PFO who are over 60 years of age, secondary prevention of stroke with the help of antiplatelet agents is recommended. Anticoagulants are indicated for most patients in whom the development of cerebrovascular accident is associated with acute deep vein thrombosis, pulmonary embolism, or a hypercoagulable state [13].
Bibliography
- Dobrynina L.A., Kalashnikova L.A., Pavlova L.N. Ischemic stroke at a young age. Journal of Neurology and Psychiatry. S.S. Korsakov. 2011;111(3): 4-8.
- Adams HP, Bendixen BH, Kappelle LJ et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke; 24(1): 35–41.doi:10.1161/01.str.24.1.35
- Fu Q., Guo X., Mo D., Chen B. Young Paradoxical Stroke Treated Successfully with Mechanical Thrombectomy Using Solitaire and Transcatheter Closure of Patent Foramen Oval. Int Heart J. 2017;58(5):812-815. https://doi:10.1536/ihj.16-461
- Homma S., Messé S., Rundek T. et al. Patent foramen ovale. Nature Reviews Disease Primers. 2016;2(1). https://doi:10.1038/nrdp.2015.86
- Homma S., Sacco R. Patent Foramen Ovale and Stroke. Circulation. 2005;112(7):1063-1072. doi:10.1161/circulationaha.104.524371
- Davison P., Clift PF, Steeds RP The role of echocardiography in diagnosis, monitoring closure and post-procedural assessment of patent foramen ovale. J. Echocardiogr. 2010; 11 (10): 27-34. doi:10.1093/ejechocard/jeq120
- Hoffman JIE Atrial Septal Defect (Secundum). The Natural and Unnatural History of Congenital Heart Disease, 131–156. doi:10.1002/9781444314045.ch14
- Contegiacomo A, del Ciello A, Rella R et al. Pulmonary arteriovenous malformations: what the interventional radiologist needs to know. Radiol Med. 2019;124(10):973-988. doi:10.1007/s11547-019-01051-7
- Kulesh A.A., Shestakov V.V. Patent foramen ovale and ischemic stroke. Neurology, neuropsychiatry, psychosomatics. 2019;11(2):4–11.doi:14412/2074-2711-2019-2-4-11
- Kent DM, Ruthazer R., Weimar Ch. et al. An index to identify stroke-related vs incidental patent foramen ovale in cryptogenic stroke. Neurology. 2013;81:619-25. doi: 1212/WNL.0b013e3182a08d59
- Chechetkin A.O. Methodological aspects of diagnosing a patent foramen ovale using contrast transcranial Dopplerography (literature review). Ultrasound and functional diagnostics. 2007;1:102-118.
- Sloan MA, Alexandrov AV, Tegeler CY et al. Assessment: transcranial Doppler ultrasonography: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. 2004;6:1468–1481. doi: 1212/wnl.62.9.1468
- European position paper on the management of patients with patent foramen ovale. General approach and left circulation thromboembolism. EuroIntervention 2019;14:1389-1402. doi: 4244/EIJ-D-18-00622
Symptoms of arterial embolism
Symptoms of embolism depend on where the clot stops in the artery. Thromboembolism can be suspected if the following signs are present:
- Sudden coldness of the extremity
- No pulse
- Difficulty in movement
- Tingling or numbness
- Decreased sensitivity
- Pain or spasms in the muscles of the affected limb
- Sharp pallor of the skin of the affected limb
If blood flow is not restored in a timely manner, the following symptoms occur:
- Blue or marbled skin color
- Formation of blisters filled with bloody contents
- Absence or sharp decrease in range of motion
- Lack of sensation in the affected limb
- Impossibility of even passive movement in the joints (contracture)
- Signs of ischemic gangrene - tissue breakdown
A comment
The team of authors provides a clinical observation of the development of venous and paradoxical air embolism in a patient with a brain stem tumor. This is a very serious and sometimes fatal complication of neurosurgical operations performed on patients in a sitting position. The article discusses various approaches and methods previously published by domestic and foreign researchers, aimed at both preventing the development of air embolic complications and their treatment. Algorithms for pre- and intraoperative examination and patient management are discussed. During the discussion of this clinical observation, the authors provide literature data on the possible causes of venous and paradoxical air embolisms in neurosurgical practice.
In the presented clinical case, a paradoxical air embolism that developed during neurosurgical intervention in a sitting position led to the formation of acute myocardial infarction and cerebrovascular accident, which ultimately caused the death of the patient. The authors focus readers' attention on methods for pre- and intraoperative diagnosis of these complications, pointing out that effective methods for treating venous and paradoxical air embolism have not currently been developed. The authors come to a conclusion, one of which indicates the need to switch to performing neurosurgical interventions in the supine position in all technically possible cases and to avoid surgery in the sitting position as much as possible to reduce the risk of developing air embolic complications.
The article may be useful not only to neurosurgeons and anesthesiologists-resuscitators, but also to all related specialists involved in the treatment of patients with brain damage.
S.V. Sviridov (Moscow)