Possible reasons
The reasons for the formation of blood clots and emboli in the arteries can be divided into several groups:
· pathological changes in the walls of the arteries (endarteritis, atherosclerosis, vasculitis);
· changes in blood flow that occur with aneurysms, vascular stenosis, as well as their damage (bending, compression, etc.);
· diseases that negatively affect blood clotting.
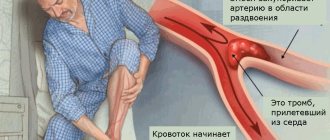
The source of arterial thromboembolism often becomes the heart in the presence of pathologies associated with cardiac arrhythmias, left ventricular aneurysm, endocarditis, etc.
Also, the formation of blood clots may be preceded by a surgical operation to replace the valve apparatus with an artificial prosthesis.
Another common source of the disease are vessels with atherosclerotic plaques.
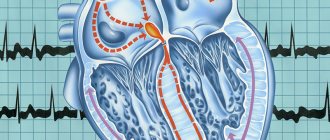
In the development of arterial thrombosis and embolism, special attention should be paid to the functional neurovascular factor. The human central nervous system is directly involved in the regulation of blood circulation in certain areas, which is why nervous shocks and disorders often cause disturbances in coronary and cerebral circulation.
Thrombosis of arteries and veins: symptoms, causes, treatment and prevention
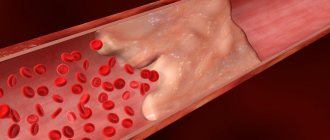
Thrombosis is a dangerous condition in which a blood clot forms in a vessel. Such a thrombus can grow, clogging the vessel until it completely occludes, but under certain conditions it can also “break off”, becoming a thromboembolus.
Treatment of this pathology is still difficult, after which relapses are possible1. Therefore, it is important to know the causes of thrombosis so that, if you discover them in yourself, you can begin prevention in time. We will talk about this, as well as about the manifestations of the disease.
Causes of blood clots
Blood clots in blood vessels occur under the influence of a complex of factors that could change:
- blood viscosity;
- the speed of its movement;
- the condition of the wall of blood cells, especially platelets, which also affected their electrical charge.
The main causes of thrombosis include:
A. Conditions in which the blood coagulation system becomes overactive, and its antagonist - proteins and enzymes of the blood anticoagulation system - cannot prevent this
These can be hereditary or acquired diseases, the most common of which are:
- antiphospholipid syndrome;
- hemophilia;
- increased blood levels of the amino acid homocysteine;
- systemic lupus;
- decreased concentration of proteins C or S in the blood;
- antithrombin deficiency;
- DIC syndrome is an acute condition that develops in many serious diseases (including infectious ones), after operations, during complications of pregnancy: preeclampsia and eclampsia, incompatibility of mother and fetus by blood type, and others.
B. Vascular injuries
They occur during the placement of venous catheters (then symptoms of venous thrombosis of the upper extremities are observed), operations - especially during the installation of prostheses and consolidation of fractures, and surgical treatment of the pelvic organs.
B. Providing conditions for blood stagnation
This leads to:
- long-term immobilization: in the treatment of fractures, as well as other serious diseases;
- paralysis;
- paresis;
- long journeys;
- air travel - especially in the presence of concomitant pathologies, for example, rhythm disturbances or previous myocardial infarction;
- anesthesia, when it lasted more than 60 minutes and involved the use of artificial ventilation and, accordingly, the use of drugs that relax the muscles.
D. Certain diseases
Another reason for the development of thrombosis are pathologies that affect blood clotting or the flow of blood vessels. This:
- tumors: any malignant, including leukemia;
- acute myocardial infarction;
- inflammation of the colon;
- obesity;
- stroke;
- heart failure;
- kidney diseases in which nephrotic syndrome develops (edema, loss of proteins in the urine, increased cholesterol levels);
- paroxysmal hemoglobinuria;
- systemic vasculitis, including those accompanying joint diseases;
- previous thromboembolism;
- decreased platelet levels associated with the need for long-term use of heparin;
- vascular atherosclerosis.
In addition, a fairly common cause of thrombosis is pregnancy, especially its second half, as well as the postpartum period. This is due to an increase in progesterone levels, which increases blood viscosity. An enlarged uterus can compress the veins of the pelvis, as a result of which the speed of blood flow in them decreases by 2–3 times1. Thrombosis can also begin when, in the postpartum period, physiological thrombosis of the veins of that part of the uterus that previously communicated with the placenta begins1.
D. Taking medications
Contraceptives, hormonal drugs - including those for the treatment of malignant neoplasms, chemotherapy drugs, including tamoxifen - increase the risk of intravascular blood clots.
Difference between the causes of arterial and venous thrombosis
In general, the reasons for the development of thrombosis in the venous bed are listed above. Venous vessels are distinguished by the fact that their muscular wall is poorly developed, and the movement of blood in them occurs slowly. This promotes stagnation and the formation of blood clots.
In this regard, the vessels of the inferior vena cava system are the most vulnerable: the blood in them is forced to rise against gravity - only with the help of the muscles of the lower leg, the suction pressure of the lungs and the pericardium. Therefore, symptoms of thrombosis of the lower extremities and pelvic veins - namely, they are part of the inferior vena cava system - occur in 95% of cases of venous thrombosis (phlebothrombosis)2.
Most often, blood clots form in the deep veins of the leg. This is facilitated by conditions in which the “second heart” of the body, the calf muscles, is switched off. The main one is anesthesia with the use of muscle relaxants, drugs to relax all muscles, making many abdominal operations possible. Muscle relaxants cause much deeper muscle relaxation than is possible during sleep or even with muscle paralysis. This is why it is important to wear compression garments before surgery: it supports the “second heart” in artificial tone.
Now about the causes of arterial thrombosis. In arterial vessels of large and medium caliber, the blood flow speed is high3. Therefore, blood clots can occur:
- On atherosclerotic plaques: these lipid deposits occur mainly in areas of uneven blood flow, so it is easier for a blood clot to stay here.
- In arteries of small diameter, where the speed of blood flow is low.
- On the walls of an aneurysm - a pathological expansion of the vessel. Consequently, with Marfan syndrome, Ehlers-Danlos syndrome, neurofibromatosis, Erdheim tumor and other pathologies in which aneurysms are formed very often - due to a violation of the structure of the vascular walls.
- In the area of the artery wall that is inflamed or damaged by its own immunity.
- In a place where the artery is compressed: by bone, tumor, cyst.
- In a place where the wall of an artery (mostly of small diameter) consists of “wrong” proteins that attract platelets to themselves, although they should repel them due to the difference in electrical charges. This occurs with collagenosis.
- With generalized DIC, when the blood coagulation system practically no longer stops the speed of blood flow.
Factors predisposing to angiothrombosis
Not everyone who has the above causes of thrombosis necessarily develops the disease. Often external influences are also needed, which will trigger the pathological formation of blood clots in the vessels.
These factors become:
- Smoking. In this case, thrombosis mainly develops in the arteries - and the vessels of the lower extremities suffer from smoking 2-3 times more often4 than this bad habit causes cardiac ischemia. The reason is a prolonged spasm of blood vessels (vasa vasorum), small vessels that supply arteries and veins.
- Diabetes. This pathology leads to disruption of the properties of the vascular wall, mainly arterial. As a result, although diabetes is not the direct cause of thrombosis, it increases the risk of its development by 2–4 times1. In addition, pathology is also a factor that will worsen the prognosis after surgical treatment of arterial thrombosis, therefore, if it is present, it is necessary to maintain blood glucose within normal limits.
- Violation of fat metabolism. Each increase in total cholesterol concentration by 10 mg/dL increases the risk of obliterating atherosclerosis, and with it thrombosis of the lower extremities, by 5–10%1.
- Impact of local factors. If there is a cause for the development of thrombosis, its risk is higher in those people whose limbs are more often injured (minor scratches and cuts count), hypothermia or overheating.
- Stress. Psychogenic stress leads to the production of increased levels of cortisol, and it leads to prolonged spasm of the arteries with disruption of normal blood flow through the vessels.
Risk factors for angiothrombosis - venous and arterial - also include those circumstances that cannot be changed, but can be taken into account by starting prevention in time. This:
- Age: the older a person is, the more attention he should pay to his health, including the condition of his lower extremities. The symptoms of thrombosis described below are not normal at any age.
- Male gender: this increases the risk of clots in both veins and arteries.
How does angiothrombosis manifest?
In general, the symptoms of thrombosis depend on three factors:
- where the blood clot formed - in an artery or vein;
- in which vessel and at what level did the thrombus appear;
- whether the clot blocked the vessel, how quickly it happened.
Manifestations of phlebothrombosis are swelling and pain in the limb, which intensifies when walking. In this case, the swollen skin becomes bluish, this color becomes brighter when standing. The affected limb is warmer than the healthy one. Under the swollen skin you can feel a painful cord - this is the affected vein. Active palpation or squeezing of a limb is dangerous for the development of pulmonary embolism.
The level of swelling depends on the location of the blood clot: the lower it is, the less surface area of the leg or arm will swell. In some cases, the disease occurs hidden. Then thrombosis of the lower extremities is detected after symptoms of pulmonary embolism: a sharp feeling of lack of air, shortness of breath, fainting, strong heartbeat and cough.
With arterial thrombosis, the symptoms are different. While the clot grows and blocks the artery by 25% or less, the limb will develop:
- numbness;
- tingling;
- chilliness that comes in “hot flashes” and is localized closer to the fingers;
- heaviness in the legs - when exercising.
As the blood clot increases, more noticeable symptoms of thrombosis are observed: the limbs begin to tire faster, become more sensitive to cold, and “pins and needles” and numbness occur more often and last longer. One limb becomes paler, drier and colder than the other. It often develops pustules and inflammations that do not heal for a long time.
As the disease progresses, pain occurs in the affected leg or arm, and with thrombosis of the arteries of the lower limb, lameness appears. And in an advanced stage, if acute thrombosis does not develop, trophic ulcers appear - first as superficial wounds that do not heal, and then as deep “potholes” with uneven edges. The final symptoms of thrombosis, which develops gradually, are the development of wet gangrene, the appearance of signs of general intoxication: nausea, weakness, loss of appetite, headaches. Along with this, body temperature often also rises. If the affected part of the limb is not amputated, the functioning of the kidneys, cardiac and respiratory systems is disrupted.
If the blood clot in the artery grows quickly, acute symptoms of limb thrombosis appear:
- skin swelling;
- severe pain in the leg or arm;
- pain when touching a limb;
- rapid development of gangrene.
Changes are observed below the artery blocked by the thrombus. This is where the pulse disappears, which is noted at the very beginning of the disease.
Complications
Regardless of the cause of thrombosis, its main complications are thromboembolic. This term refers to the detachment of a blood clot from the wall of a vessel and its blockage of an artery of suitable diameter, as a result of which the part of the organ that fed from this artery does not receive nutrition and dies.
Most often, thromboembolus enters the arteries extending from the aortic arch (this includes the arteries supplying the brain), in second place are the large arteries of the pelvis and lower extremities, then the arteries going to the internal organs. Thromboembolism of the upper limb arteries very rarely develops1.
One of the common complications of the most common thrombosis - deep vein thrombosis of the lower extremities - is PE (pulmonary embolism), when a larger or smaller area of the lungs ceases to be supplied with blood. PE does not develop in every case of phlebothrombosis, but, unfortunately, risk factors for this dangerous disease have not been identified. It is believed that the greatest danger of pulmonary embolism exists in the early stages after the onset of symptoms of thrombosis of the extremities - while the thrombus is still loosely fixed to the vein wall and can come off. However, thromboembolism can occur after a long period of time after phlebothrombosis, especially if no preventive measures are taken.
In addition to thromboembolism, phlebothrombosis can be complicated by the growth of a blood clot and its spread to nearby veins. For example, from the deep veins of the leg, a clot can “grow” to the popliteal vein, and from the superficial femoral vein to the common femoral vein. In this case, the outflow of blood from the limb worsens, and the risk of blood clot rupture increases.
Treatment
Therapy should be started as early as possible. In acute thrombosis - both venous and arterial - it consists of administering those drugs that can dissolve the blood clot. If drug thrombolysis is ineffective, surgery is performed to remove the blood clot from the vessel. After this, anticoagulant therapy continues under the control of coagulation parameters.
Treatment is often performed in the intensive care unit, under the supervision of a vascular surgeon.
For chronic symptoms of thrombosis of the upper limbs or legs, treatment is also prescribed by a vascular surgeon. In the initial stages, it is conservative and consists of prescribing vasodilators, angioprotectors, B vitamins, and cholesterol-lowering agents; for phlebothrombosis - venotonics.
Prescription of blood thinning medications is mandatory. Thrombo ACC is a drug of acetylsalicylic acid that blocks the deposition of platelets on the walls of blood vessels, including the affected one, thereby preventing the blood clot from growing. Thrombo ACC tablets are coated with an enteric film coating, which reduces the likelihood of developing local irritant effects on the stomach.
In case of advanced chronic thrombosis, it is necessary to restore the patency of the vessel. The decision on surgical treatment to restore the patency of the vessel is made by the doctor. Regardless of the cause of thrombosis, after surgery, anticoagulants and/or antiplatelet drugs are prescribed for a long period.
Prevention
It consists of improving blood flow in the extremities. To do this you need:
- maintain blood pressure, cholesterol and blood glucose within normal limits;
- undergo preventive examinations, respond in a timely manner to pathological changes in the heart and blood vessels;
- walk more;
- avoid standing for long periods of time;
- reduce salt intake;
- enrich the diet with foods rich in fiber, as well as polyunsaturated fatty acids, vitamins E and P;
- protect limbs from injury, hypothermia and overheating.
If you have one or more risk factors, you need to get your doctor’s recommendations for preventive use of Thrombo ACC.
The drug is adapted for long-term use. Acetylsalicylic acid in cardiac dosages has been actively used by specialists for many years to prevent thrombosis and their thromboembolic complications. * There are contraindications, before use you must consult a specialist 1 Zatevakhin I.I. Treatment tactics for acute thrombosis of the arteries of the lower extremities // Materials of the fourth international surgical congress “Scientific research in the implementation of the Russian Population Health program” - M., 2012. 2 Arterial thrombosis and embolism of the extremities / Under. ed. IN AND. Lupaltsova, S.S. Miroshnichenko, I.A. Dekhtyaruk / Kharkov, KhNMU, 2010 3 Ministry of Health of the Russian Federation. Clinical recommendations. Diseases of the arteries of the lower extremities. 2021 (reviewed every 3 years). 4 A. K. Lebedev, O. Yu. Kuznetsova. Deep vein thrombosis of the lower extremities. Clinical recommendations. / M, 2015. RUS-GPS-THR-NON-01-2019-1486
Symptoms of the disease
With arterial thrombosis or embolism, an acute cessation of blood circulation occurs in those tissues for which the affected vessel is responsible for the blood supply. In this case, you may feel severe pain in one or another organ (limb, abdomen, etc.). Gradually, in the absence of medical care, the tissues in the affected area die and gangrene develops.
If there are no alternative routes for bypass blood flow, as, for example, with damage to the femoral artery, the disease will be severe. The disturbances will not be so severe if there are other vessels capable of supplying blood to the affected organ.
Thromboembolism in most cases is characterized by a sudden onset . If we are talking about damage to the arteries of the lower extremities , you will feel acute pain and gradually increasing numbness. As sensitivity is lost, the limb becomes immobile. Embolism of large arteries is accompanied by a state of shock with cold sweat, nausea and vomiting. The skin on the affected area first turns pale, but then the pallor gives way to patchy cyanosis. The pulse of the peripheral arteries located below the affected area is not determined. With long-lasting spasm and lack of blood circulation, gangrene .
With thromboembolism of the abdominal aorta, the clinical picture is determined by the completeness and speed of its blockage. The first sign of pathology is a sharp and very severe pain in the abdomen, radiating to the lower extremities. The skin turns pale, the patient falls into a state of shock. The pulse in the vessels of the lower extremities cannot be felt, and rapidly developing gangrene can lead to death within a few days. If the disease develops gradually, the symptoms do not appear so clearly and do not develop so rapidly.
Blockage of the mesenteric artery is accompanied by an infarction of the affected area of the intestine, which manifests itself with signs characteristic of an acute surgical abdomen: acute pain, increased body temperature, shock, vomiting.
What it is?
Thrombosis
is a pathological condition in which dense blood clots (thrombi) form in the vessels, slowing down or completely stopping the normal flow of blood. As a result, a lack of organ nutrition (ischemia) may occur, which in turn can lead to tissue death (necrosis, infarction) and death. There are two types of thrombosis: venous and arterial. From the names it is clear where the formation of blood clots occurs. In the first case - in the veins, in the second - in the arteries. The disease can occur in acute and chronic form. Arterial thrombosis is the most dangerous.
Diagnosis of arterial thrombosis and arterial embolism
In our department of vascular surgery, the diagnosis of arterial thrombosis and arterial embolism is performed in accordance with the highest medical standards. Diagnostic measures include:
· collection of anamnesis and analysis of patient complaints;
· visual inspection;
· a number of laboratory tests;
· performing ultrasound examination of blood vessels;
angiography;
· computed tomography using a contrast agent.
Based on the results of the studies, the degree of the disease is determined: first degree (A, B), second degree (A, B) or third degree (A, B). After making an accurate diagnosis, our specialists decide on further treatment tactics.
Diagnosis of deep venous thrombosis
Diagnosis of thrombosis is extremely difficult. This is primarily due to the absence of clinical symptoms. According to some data, out of 1000 venous thromboses, only 100 have any clinical manifestations. Of these, 60 patients will develop PE, but only 10 will have clinical signs. It should be recognized that today there is not a single clinical symptom, laboratory or instrumental sign that would indicate with absolute certainty the presence of PE and DVT. Clinical manifestations of thrombosis and ultrasound results can be the basis for the correct diagnosis of venous thrombosis. The clinical picture of deep vein thrombosis consists of a complex of symptoms that characterize a sudden disturbance of venous outflow with preserved arterial blood flow to the limb. Swelling, cyanosis of the limb, bursting pain, local increase in skin temperature, overflow of the saphenous veins, pain along the vascular bundle are characteristic to one degree or another for thrombosis of any localization. Movements in the joints of the limb and sensitivity remain virtually unchanged. General signs, such as low-grade fever, weakness, adynamia, and slight leukocytosis, occur in most patients. The diagnosis of thrombosis largely depends on the location of the lesion, i.e. on the level of distribution of thrombotic masses.
Treatment methods
Arterial thrombosis and embolism require hospital treatment , which is selected depending on the severity of the pathology.
Conservative therapy with the use of anticoagulants, angioprotectors, intra-arterial drug block and other drugs is prescribed for the first degree of the disease. Non-surgical treatment may be possible for the second degree A, but more often doctors still advise resorting to surgical removal of blood clots.
In our department, highly qualified specialists perform surgical removal of blood clots (direct and indirect thrombectomy) and perform shunt operations. If a patient experiences muscle contraction due to swelling under the fascia, a fasciotomy is indicated in addition to vascular surgery.
If we are talking about arterial thrombosis of the limb of the third degree, then it will no longer be possible to avoid the formation of a gangrenous focus. In some cases, surgery on the affected vessels can be performed to improve blood flow, which makes it possible to avoid amputation. In case of third degree B, high limb amputation is prescribed.
Treatment of blood clots in the arteries of the brain
It is necessary to immediately begin a set of therapeutic measures.
Medication
Drugs that directly affect the rheological properties of blood:
- Anticoagulants - have an effect on the coagulation process, inhibiting the adhesion of platelets to each other and preventing small clots from forming one large one. Clopidogrel, indobufen, ditazol, ticlopidine;
- Thrombolytics – used for moderate and higher degrees of thrombosis: they dissolve the clot and initiate fibrinolysis. Streptokinase, tenecteplase;
- Antiplatelet agents – suppress blood clotting, reduce thrombus formation. Warfarin, heparin, dicoumarin, hirudin and drugs from other medicinal groups. Aspirin (acetylsalicylic acid) is the most popular of these.
Drugs acting on the walls of the vessel:
- Vasodilators;
- Antihypertensives – reduce blood pressure;
- Pentoxifylline derivatives enhance microcirculation in brain tissue.
- Nootropics are medications that stimulate metabolism in nervous tissue, increase resistance to oxygen deficiency, and help improve intellectual abilities and memory.
Surgical
To prevent a stroke, the following can be done:
- Carotid endarterectomy – removal of blood clots and atherosclerotic plaques on the carotid artery when 70% stenosis is detected and in patients who have suffered a transient ischemic attack (TIA). Surgery is often used to prevent future strokes.
- Stenting and angioplasty is an expansion of the diameter of narrowed sections of arteries, with atherosclerotic changes in those that are located in hard-to-reach areas. A balloon is inserted into the narrowing areas, which, when inflated, increases the diameter of the vessel. A mesh element, a stent, is placed in the artery to prevent the narrowing of the vessel. Allows you to avoid dangerous consequences such as stroke and ischemic attack.
Prevention measures
Thromboembolism prevention is based on timely detection and treatment of heart and vascular diseases, so we recommend undergoing a comprehensive examination at least once a year.
It is also necessary to lead a healthy and active lifestyle, exercising moderately and adhering to the principles of a healthy diet. The diet should be dominated by foods of plant origin, but it is advisable to exclude foods containing cholesterol.
In the summer, you should avoid dehydration by following a drinking regime. Bad habits, such as smoking, increase the risk of blood clots - give them up.
Forecast
The prognosis for treatment of thrombosis depends on the following factors:
- Where is the carotid artery located and what is its role in the human circulatory system?
- competently prescribed therapy and the patient’s adherence to the doctor’s recommendations, lack of self-medication and ignoring symptoms;
- how quickly medical care was provided after a blood clot formed;
- the presence of concomitant diseases, including those associated with blood vessels (especially cerebral);
- patient's age;
- the degree of severity and nature of changes in brain tissue caused by deterioration of blood supply due to thrombosis (if any).
The timeliness and correctness of medical care is very important.
Syndromes of thrombosis of the anterior artery of the choroid plexus
The anterior artery of the choroid plexus of the brain begins from the internal carotid artery and supplies blood to the posterior thigh of the internal capsule, as well as the white matter of the brain to the side and behind it, through which part of the optic fibers passes from the lateral geniculate body to the calcarine groove. This area of the brain is also supplied with blood by:
- penetrating vessels coming from the trunk of the middle cerebral artery (arteries of the lenticular nucleus and striatum)
- penetrating branches of the posterior communicating artery
- posterior choroid plexus artery
Therefore, the full clinical syndrome in the form of contralateral hemiplegia (paralysis of the muscles of the body on the opposite side), hemianesthesia (hypoesthesia) and homonymous hemianopsia (loss of half the visual field on the side of the brain lesion) may not develop. Instead, syndromes with minimal severity of neurological focal disorders are observed.
Indeed, in cases of surgical occlusion of the anterior artery of the choroid plexus for the purpose of treating the symptoms of Parkinson's disease, some patients do not show signs of circulatory deficiency in the area of its basin. Patients who initially presented with advanced clinical symptoms often recover fully or partially, apparently due to sufficient levels of collateral arterial blood flow in this part of the brain.
Clinical picture
Common complaints:
- persistent or persistent increasing headaches;
- impaired sensitivity and motor skills of the muscles of the face, arms and legs, right or left half of the body;
- persistent distortion of speech and its understanding;
- blurred vision;
- loss of body balance, dizziness;
- feverish condition;
- excessive sweating;
- blood pressure surges;
- uncontrolled acts of defecation and urination;
- loss of consciousness;
- convulsive contractions, muscle twitching;
- nausea, vomiting.
Thrombosis of the basilar artery
Complaints regarding thrombosis of the basilar artery supplying the brain stem:
- throbbing occipital pain;
- dizziness, patients are “stormy, rocking on the waves”;
- blurry visual perception;
- impaired sensitivity of the skin around the mouth;
- gaze paresis – the inability to move both eyes simultaneously in vertical or horizontal directions;
- impaired sensitivity of half of the face;
- fainting;
- noise in ears.
Thrombosis of the carotid artery (internal, external)
Complaints characteristic of deterioration of blood supply to the brain through the internal carotid arteries :
- serious weakening of visual perception, even blindness;
- inability to speak, speech confusion;
- deterioration of motor function of the upper extremities;
- tremor;
- fainting;
- paresis of one or both halves of the body.
Complaints characteristic of deterioration of blood supply to the cerebral cortex, tissues of the neck and face through the external carotid arteries :
- dry mucous membranes;
- neck pain;
- distortion of facial expressions, paralysis of facial muscles;
- fainting;
- slurred speech;
- constant pain in the head.
Suspicion of thrombosis
To properly treat thrombosis, you need to make an accurate diagnosis. Different methods are used for this:
- Duplex scanning. With its help, visualization of blood vessels is created and blood flow is examined.
- X-ray contrast venography. In this case, a contrast agent is injected into the vessel.
- In case of doubt, MR-CT angiography is performed when making a diagnosis.
- If there is a risk of pulmonary thromboembolism, the patient undergoes a chest x-ray and scintigraphy.
- Impedance plethysmography is performed if there are signs of leg thrombosis. This method uses a cuff that compresses the lower leg for subsequent short-term occlusion of the veins. The new vessel volume after blood flow is then measured. This analysis provides an accurate diagnosis (up to 90%) and allows one to recognize the presence of deep venous thrombosis in the area above the knee.
At the first suspicion of thrombosis, you should immediately consult a doctor. Self-medication at home is very dangerous.
Anterior cerebral artery thrombosis syndromes
The anterior cerebral artery of the brain has two segments:
- precommunal (A1) segment of the circle of Willis, or stem, segment that connects the internal carotid artery with the anterior communicating artery
- postcommunal (A2) segment, originating from the connection of the A1 segment with the anterior communicating artery
Segment A2 of the anterior cerebral artery, through its cortical branches, supplies blood to the anterior 2/3 of the medial surface of the orbital part of the frontal lobe, the pole of the frontal lobe, the strip of cortex along the superomedian border and the anterior 2/3 of the corpus callosum. On the other hand, the A1 segment of the anterior cerebral artery gives off many deep penetrating branches, going mainly to the anterior femur of the internal capsule, the anterior perforated substance, the amygdala, the anterior hypothalamus and the lower part of the head of the caudate nucleus of the brain.
Cerebral infarctions (strokes) in the anterior cerebral artery territory are rare. Blockage (occlusion) of the trunk or segment of the A1 anterior cerebral artery is usually well compensated due to the possibility of collateral blood flow from the opposite side. The most severe disorders occur in cases where both anterior cerebral arteries originate from a single trunk (in the case of a congenital anatomical feature of its structure in the patient), blockage (occlusion) of which leads to the occurrence of an extensive infarction in the anterior cerebral arteries of both hemispheres of the brain.
Clinical manifestations of blockage (occlusion) in the basin of both anterior cerebral arteries include bilateral pyramidal disorders with paraplegia (paralysis of the muscles of the left and right half of the body) and pronounced changes in the psyche due to bilateral damage to the frontal lobes of the brain.
Components of a typical syndrome that develops when the anterior cerebral artery is blocked:
Clinical manifestations | Affected brain structures |
| Contralateral foot and leg paralysis | Motor projection of the leg |
| Less severe contralateral arm paresis | Involvement of the area of the cortical projection of the hand and the fibers coming from it in the corona radiata |
| Cortical lesion leading to loss of sensation in the toes, foot, and leg | Sensory projection of the foot and leg |
| Urinary incontinence | Sensorimotor area of the paracentral lobule |
| Contralateral grasping and sucking reflexes, paratonic rigidity | Inner surface of the posterior part of the frontal lobe - supplementary motor area |
| Abulia (akinetic mutism), slowness, retardation, periodic sudden hesitations, spontaneity, whispered speech, motor inactivity, reflex animation when exposed to visual and sound stimuli | Localization is unclear - probably the cingulate gyrus and the medial parts of the parietal and temporal lobes |
| Impaired walking and standing (gait apraxia) | Frontal cortex near the motor projection of the leg |
| Dyspraxia in the left limbs, left-sided tactile aphasia | Corpus callosum |