The mortality rate of the working-age population from unnatural causes - accidents, poisonings and injuries - in Russia is almost 2.5 times higher than similar indicators in developed countries, and 1.5 times higher than in developing countries of Eastern Europe.
According to statistics, in the Russian Federation in 2009, more than 10 million adult victims sought medical help for injuries, poisoning and some other consequences of external causes. The injury rate was 86.6 per 1000 adults.
The most common injuries reported among the adult population are bruises and superficial injuries without damage to the skin (30.6%). The second place in the structure of injuries is occupied by bone fractures (21.5%). Of all fractures, 86.6% are localized on the extremities, including 61.8% on the lower ones.
About 15-20% of all victims with severe combined trauma die from complications of traumatic disease. One of these complications is fat embolism syndrome (FES).
This syndrome can be defined as a clinical condition characterized by dysfunction of the lungs and central nervous system due to obstruction of microvessels by large globules of fat, which occurs mainly after severe injuries with fractures of long tubular bones or pelvic bones.
Even R. Lowel in 1669 established that when milk or fat is introduced into the bloodstream, the death of animals occurs, but the reasons were not clarified. Later, F. Magendief (1821), during experiments on dogs that were injected with olive oil into a neck vein, discovered the causes of death of the animals: within a day the dogs developed pneumonia.
In 1861, F. A. Zenker described fat droplets in the lung capillaries of a railroad worker who suffered a fatal thoracoabdominal compression injury. In 1863, E. Bergmann first established the clinical diagnosis of FFE. After liquid pork fat was injected into the femoral vein of cats in animals that lived for 6-24 hours, autopsy revealed drops of fat in the vessels of the lungs, liver and kidneys. In subsequent years, much attention was paid to the issues of etiology, pathogenesis, clinical forms, as well as treatment of FES.
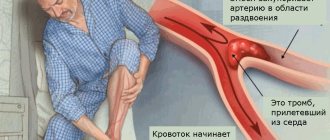
Fat embolism syndrome most often develops with closed fractures of long tubular bones and pelvic bones. In patients with a fracture of one long bone, the probability of developing the syndrome is 1-3%, and this number increases with the number of fractures. In bilateral femoral fractures, FFE is detected in 33% of cases.
The syndrome occurs mainly in adults and rarely in children. This may be due to the fact that in children the bone marrow contains more hematopoietic tissue and less fat.
Pathophysiology
There is considerable disagreement in the current literature on the pathogenesis of fat embolism. Three main theories have been proposed.
Mechanical theory
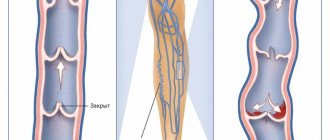
In 1924, Gauss suggested that after a fracture of long tubular bones, drops of fat from the damaged adipose tissue enter the venous bed. This occurs when intramedullary pressure is higher than venous pressure. Fat emboli are then transported into the pulmonary vasculature.
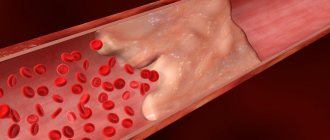
When emboli are more than 8 µm in diameter, capillary embolization occurs; when the size is up to 7 µm, they can pass through the pulmonary capillaries and reach the systemic circulation, causing embolization of the brain, skin, kidneys and retina.
Sometimes fat globules enter the systemic circulation through pulmonary precapillary shunts or in the presence of an intracardiac arteriovenous defect (foramen ovale). However, this theory does not explain the rather long delay (24-72 hours) in the development of fat embolism after acute trauma. Fat globules in the peripheral bloodstream are found in almost 90% of patients, while only 2-5% of them have a clinical picture of FFE.
Biochemical theories
Lehmann and Moore (1927) first proposed the idea that there are a number of biochemical mechanisms potentially involved in the development of FFE. It is now widely believed that fat emboli are broken down into free fatty acids in the plasma. In some patients, plasma lipase concentrations increase.
It has been shown that serum from patients with acute injuries under the influence of lipase has the ability to glue chylomicrons, low-density lipoproteins, and liposomes of food fat emulsions. C-reactive protein, which increases in such patients, causes an increase in calcium-dependent agglutination of all these substances with subsequent endothelial damage.
The delay in the development of symptoms may be explained by the time required for the production of toxic metabolites. Symptoms may coincide with agglutination and degradation of fat emboli. Circulating levels of free fatty acids are moderately elevated in patients with fractures.
However, the evidence for these mechanisms of FFE remains largely indirect. According to this theory, fat embolism due to the simultaneous disimulsification of lipids in the entire bloodstream should develop simultaneously in both circles of the blood circulation, and the clinical picture appears first in the lesser circle and then in the greater. It was not possible to reproduce the experimental model of fat embolism by introducing lipase.
Coagulation theory
According to this theory, tissues with a high content of thromboplastin with elements of bone marrow after a fracture of long tubular bones enter the veins. In this case, the complement system and external coagulation cascades are initiated through direct activation of factor VII, which leads to intravascular coagulation by fibrin and fibrin degradation products.
They act along with leukocytes, platelets and fat globules in conjunction with an increase in pulmonary vascular permeability. They may also act directly on the endothelium through the release of numerous vasoactive substances.
Reasons for the development of the problem
There are several reasons why this type of blood flow may develop. One of them is injuries. Moreover, we are talking about fractures of the femur, tibia and pelvis. If bone tissue is crushed, the risk of developing pathology increases.
Question answer
What is known about the driver Sergei Zakharov who died in an accident with Efremov?
Another reason is shock and post-resuscitation illness. Due to a metabolic storm, emboli form in the body. Most often in this situation, symptoms appear within 2-3 days.
Risk factors also include sepsis, tumors, diabetes mellitus, severe burns, and acute pancreatitis. Excessive blood loss aggravates the situation.
Clinical picture
Quite conventionally, pulmonary, cerebral and the most common mixed form are distinguished. The clinical picture of FFE develops, as a rule, after a “lucid interval” lasting from 12 to 72 hours after injury. The duration of the latent period is less than 12 hours in 3% of patients, from 2 to 24 hours in 10%, from 24 to 48 hours in 45%, from 48 to 72 hours in 33%, and over 72 hours in 9%.
The classic triad of fat embolism syndrome includes respiratory manifestations (95%), cerebral symptoms (60%), and skin petechiae (33%).
Pulmonary manifestations (shortness of breath, tachypnea and hypoxemia) are often the first clinical symptoms of the disease. Their severity varies, but respiratory failure similar to acute respiratory distress syndrome may develop. Approximately half of patients with FES caused by long bone fractures develop severe hypoxemia and respiratory failure requiring mechanical ventilation.
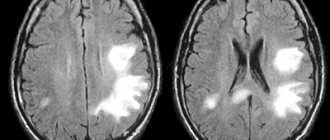
Neurological symptoms resulting from cerebral embolism are often present in the early stages and usually occur after the development of respiratory failure. Their range can be varied: motor restlessness, development of convulsions, lethargy, confusion, up to severe coma. Focal neurological symptoms have been described, including hemiplegia, aphasia, apraxia, visual impairment and anisocoria. Fortunately, almost all neurological symptoms are transient and completely reversible.
Petechiae are considered a pathognomonic sign of fat embolism in the systemic circulation. The characteristic pinpoint rash may be the last component of the triad, a symptom that develops in 60% of cases and is due to cutaneous capillary embolism leading to extravasation of red blood cells.
Petechiae are most often localized on the conjunctiva, skin folds on the upper body, especially the neck, and in the axillary areas. Petechiae usually appear within the first 36 hours and disappear completely within 7 days.
Ocular manifestations . Fat globules are sometimes found in the retinal vessels. With ophthalmoscopy, retinopathy (Purcher's symptom) can be detected - the detection of white-gray round spots located on the fundus near the retinal vessels.
Early persistent tachycardia , although not specific, is almost invariably present in all patients with fat embolism. Rarely, systemic fat embolism can affect the heart and lead to myocardial infarction and the development of acute cor pulmonale.
Systemic fever is very often an early nonspecific sign of FFE. The temperature may rise to 39-40°C. The development of hyperthermia is associated with irritation of the thermoregulatory structures of the brain by fatty acids and inflammatory mediators, as well as with impaired blood supply and hypoxia of the hypothalamus.
According to the classification proposed by A.Yu. Pashchuk and A.V. Ivanova in 1982, there are three forms of fat embolism:
- fulminant, which leads to the death of the patient within a few minutes;
- acute, developing in the first hours after injury;
- subacute - with a latent period from 12 to 72 hours.
Symptoms
Manifestations of fat embolism depend on the location of the lesion, the number and size of lipid compounds in the blood, and the degree of damage to internal organs. Symptoms of the pathology are nonspecific - it is impossible to distinguish this disease from other diseases and emergency conditions. Fat embolism occurs with damage to the respiratory system and central nervous system. There is also a mixed form involving the skin and mucous membranes. It has the most severe course.
The pulmonary form has a serious prognosis and a high degree of mortality, even with timely treatment. Patients experience:
- discomfort and tightness in the chest,
- painful sensations of a bursting, stabbing, burning nature,
- rapid breathing,
- shortness of breath up to asphyxia,
- tachycardia,
- cough with foamy pink sputum,
- large-caliber wet rales, audible at a distance,
- cyanosis of the tip of the nose, ears, nasolabial triangle, fingers on marble-pale skin,
- rapid heartbeat, cardiac arrhythmia, cardialgia.
The cerebral form of the pathology occurs when there is a blockage of the blood vessels in the brain. Multiple hemorrhages appear in the tissue. Clinically, embolism manifests itself as signs of a stroke:
- irritability, anxiety, agitation;
- lethargy, drowsiness, lethargy;
- constant, unbearable headache of a pressing, pulsating, shooting nature;
- dyspeptic symptoms - nausea and vomiting that does not bring relief;
- confusion, fainting, disorientation,
- depression of the central nervous system, coma,
- mental disorders - delusions, visual and auditory hallucinations,
- nystagmus,
- paresis and paralysis,
- loss of sensation, paresthesia,
- convulsions,
- aphasia, apraxia, anisocoria,
- decreased muscle tone.
Neurological disorders gradually progress. Foci of necrosis appear in the brain tissue. This is accompanied by additional symptoms and cognitive impairment. The clinical picture resembles manifestations of TBI, which significantly complicates the diagnostic process.
The mixed form is difficult and often complicated by life-threatening conditions. The clinical picture includes signs of cerebral and pulmonary forms. Patients develop febrile fever with chills, difficulty urinating, pain in the projection of the kidneys and multiple pinpoint rashes on the skin of the neck, front and side surfaces of the chest, shoulder, armpits, mucous membrane of the mouth, vagina, and eyes. Hemorrhagic signs are caused by overstretching of capillaries by emboli and destruction of blood vessels. Fever is associated with the effect of fatty acids on the thermoregulatory center. The temperature does not return to normal even after taking antipyretics. The pathological prognosis in this case is extremely unfavorable.
Diagnostics
Diagnosis is usually made based on clinical findings. Laboratory diagnosis is of secondary importance. The most commonly used set of major and minor diagnostic criteria proposed by AR Gurd. The diagnosis is made when at least one major and four minor signs are present.
Big criteria include :
- axillary or subconjunctival petechiae,
- hypoxemia (paO2 < 60 mm Hg; fractional concentration of O2 in the inhaled gas mixture FiO2 = 0.4),
- disorders of the central nervous system,
- pulmonary edema.
Small criteria are:
- tachycardia (more than 110 per minute),
- fever (temperature above 38.5°C),
- embolism in the retina of the eye fundus during fundoscopy,
- the presence of fatty droplets in the urine,
- sudden unexplained decrease in hematocrit and platelets,
- increase in ESR,
- detection of fat droplets in sputum.
A.Yu. Pashchuk proposed a point index SZHE . He assigned a score to each symptom: petechial rash has the highest score, and diffuse alveolar infiltration, hypoxemia, confusion, pyrexia, tachycardia, and tachypnea have lower scores of progressively decreasing diagnostic significance.
SA Schoufeld criteria are also known . They include seven clinical signs, each of which is assigned points: petechial rash - 5, diffuse infiltration of the lungs on X-ray examination - 4, hypoxemia - 3, fever (>38°C) - 1, tachycardia (>120 per minute) - 1, tachypnea (>30 per minute) - 1, disturbances of consciousness - 1. To establish a diagnosis, a score of more than 5 is required.
Fat embolism
According to WHO, injuries rank third in terms of frequency and overall mortality in the population. Trauma, as a cause of mortality, is the leading one in the age group from 20 to 60 years, exceeding it twice as much from cardiovascular diseases and cancer combined. The average age of patients with polytraumas is 38.5 years.
Fat embolism (FE) is a serious complication of the early period of injury, increasing mortality. But there is still no clear understanding of the pathogenesis, clinical picture, prevention and treatment of PVCs. The incidence of PVCs varies, according to various authors, from 0.5 to 30% in injuries with multiple fractures of long tubular bones and fractures of the pelvic bones. Mortality, despite intensive modern therapy, ranges from 3 to 67%. According to ICD 10, PVCs are classified as T79.1 - fat embolism (traumatic).
History and pathogenesis
The first description of fat embolism in humans was made in 1862 by E. A. Zenker, who, during the autopsy of a person who died from severe thoracoabdominal trauma, discovered fat drops in small vessels and capillaries of the lungs. In 1873, E. Bergman made the first lifetime diagnosis of fat embolism in a victim with a femur fracture. In 1866, F. Buch noticed that fat embolism develops most often with fractures of long tubular bones, and suggested that the source of fat droplets in the bloodstream is the bone marrow.
There are several hypotheses explaining the mechanism of development of fat embolism, but none of them is generally accepted to date.
In 1893, L. Aschoff first formulated the mechanical theory of the pathogenesis of fat embolism, which for a long time was considered the only one. When long tubular bones are fractured, drops of fat, due to increased pressure in the bone cavity as a result of injury, displacement of fragments or intraosseous interventions, enter the venous bed, from where they are transported through the bloodstream into the pulmonary vascular bed, where they create a mechanical obstacle to blood flow. With a size of up to 7 microns, they can pass through the pulmonary capillaries and reach the systemic circulation, causing embolization of the brain, skin, kidneys and retina.
However, this theory does not explain why PVCs usually develop with a delay of 24–72 hours after injury. Why are fat globules in the peripheral bloodstream found in 90-100% of patients with fractures of long tubular bones or after orthopedic surgeries, while only 2-5% of them have a clinical picture of PVCs, and also how exactly fat enters the bloodstream.
The biochemical (enzyme, enzymatic) theory, first proposed by E. Kronke in 1956, calls the cause of the development of fat embolism an increase in the activity of serum lipase, which leads to the mobilization of fat from the fat depot, an increase in the concentration of total lipids in the blood and a sharp increase in the amount of disemulsified fat . An increase in lipase activity in the blood can occur in two ways. The first is as an attempt by the body to process and absorb fat that has penetrated into the bloodstream from the sites of bone fractures. The second is as a result of the release of catecholamines due to injury and a decrease in circulating blood volume.
However, according to this theory, fat embolism due to the simultaneous disemulsification of lipids throughout the entire bloodstream should develop simultaneously in both circulation circles, but characteristic changes occur first in the pulmonary and then in the systemic circulation. Moreover, the degree of increase in lipase activity does not correspond to the size and number of fat globules identified in the victims. It was not possible to reproduce the experimental model of fat embolism by introducing lipase.
According to the colloid chemical theory , first expressed by Lehman E. in 1929, the occurrence of fat embolism is associated with a violation of the dispersion of physiological plasma fats, which occurs under the influence of traumatic influences with microcirculation disorders and changes in the rheological properties of blood in the form of hypercoagulation, resulting in small The emulsified fat forms droplets. Since slow blood flow and microcirculatory disorders are characteristic features of any critical condition, PVCs can complicate any of them.
The coagulation theory was proposed by T. S. Lavrinovich. According to this theory, all types of post-traumatic disorders of blood coagulation and lipid metabolism disorders are in pathogenetic unity and represent components of a pathological condition called post-traumatic dyslipidemic coagulopathy. Tissues with a high content of thromboplastin with elements of bone marrow after a fracture of long tubular bones enter the veins. This initiates the complement system and extrinsic coagulation cascades, leading to intravascular coagulation.
Existing concepts reflect only certain aspects of the complex mechanism of fat embolism formation. Currently, most researchers, when studying the pathogenesis of PVCs, consider it from the standpoint of a systemic inflammatory reaction - a universal reaction of the body to an extreme factor of any origin.
Etiology
Most often, PVC occurs with multiple skeletal trauma, especially with fractures of the diaphysis of the femur, shin bones, pelvis and massive damage to fatty tissue, often complicates the course of post-resuscitation illness, occurs in sepsis, tumors, diabetes mellitus, burns, pancreatitis, toxic liver necrosis, shock states.
The occurrence is described in sickle cell anemia, with the erroneous administration of fat-soluble drugs. PVCs can complicate operations of repositioning fragments, intramedullary osteosynthesis, joint replacement, and frequent attempts to reposition fragments after liposuction. Cases of fat embolism after maxillofacial plastic surgery have been described.
Risk factors for fat embolism include a long period of hypotension and a large volume of blood loss, inadequate pain relief and immobilization at the prehospital stage, transportation of the patient during the acute period of injury without proper immobilization, and frequent attempts to reduce fractures. According to some data, the risk of PVCs is higher in males and patients under 40 years of age.
M.V. Borisov and S.V. Gavrilin studied the patterns of development of fat embolism in 1718 victims with severe combined injuries. The result of the analysis was the creation of a prognostic scale. When determining the severity of injuries, they used the “VPKh-P(MT)” scale for assessing the severity of injuries developed at the military field surgery clinic; when assessing the severity of the condition of the victims, they used the “VPKh-SP(MT)” scale for objective assessment of the severity of the condition.
When predicting the risk of developing fat embolism, this scale is used for fractures of long tubular bones. The 8 signs included in the scale are determined in victims immediately upon admission to the hospital. With an index value of 5 points, the probability of developing PVCs is 7.9%, 10 points 13.3%, 15 points 18.2%, 20 points 22.1%. Based on the scale, 3 groups of victims are distinguished, for each of which the authors developed an algorithm for the prevention of PVCs.
Fat Embolism Prediction Scale
Presence of damage to two long tubular bones of the lower extremities
- No – 0 points
- Yes – 4
The severity of the pelvic injury on the VPH-P (MT) scale is more than 7 points
- No – 0
- Yes – 2
The overall severity of injuries on the VPH-P (MT) scale is more than 9.5 points
- No – 0
- Yes – 2
The severity of the chest injury on the VPH-P (MT) scale is more than 4 points
- No – 0
- Yes – 3
The severity of the condition upon admission according to the VPH-SP scale is more than 35 points
- No – 0
- Yes – 2
The volume of blood loss is more than 1500 ml
- No – 0
- Yes – 1
The duration of the period of arterial hypotension is less than 90 mm Hg. Art. upon admission more than 40 minutes
- No – 0
- Yes – 4
Inadequate immobilization upon admission
- No – 0
- Yes – 2
Classification and clinical manifestations
There are pulmonary, cerebral and, the most common, mixed forms of fat embolism.
Based on the duration of the latent period, it is proposed to distinguish the following forms of PVCs:
- fulminant, which leads to the death of the patient within a few minutes;
- acute, developing in the first hours after injury;
- subacute - with a latent period from 12 to 72 hours.
The detailed dynamics of the development of fat embolism over time varies among different authors. According to M. B. Borisov, the duration of the latent period is:
- less than 12 hours in 3% of patients;
- from 12 to 24 hours - in 10%;
- from 24 to 48 hours - in 45%;
- from 48 to 72 hours - in 33%;
- over 72 hours - in 9%.
PVCs may develop 14 or more days after injury.
The acute course is characterized by the development of a clinical picture of fat embolism in the first hours after injury. A fulminant form is considered as a variant of the acute course, when death develops within minutes after injury. Under these conditions, massive damage to the musculoskeletal system, as a rule, leads to the rapid entry of a huge amount of fat globules into the vascular bed and lungs. Occlusion of the pulmonary microcirculation by fat emboli, platelet and fibrin clots received the figurative name of “embolic shower”, reflecting the speed and prevalence of the process.
The subacute development of fat embolism is characterized by a latent period lasting from 12 hours to 3 days and less severe clinical manifestations.
Symptoms of fat embolism include nonspecific manifestations that occur in various diseases: respiratory, cerebral and skin (petechiae on the skin).
Pulmonary abnormalities with fat embolism are observed in 75% of patients and are often the first clinical symptoms of the disease. Victims experience a feeling of tightness and pain in the chest, increasing anxiety, shortness of breath, facial cyanosis, and acrocyanosis. The severity of symptoms and the degree of respiratory failure characterize the severity of lung damage. Respiratory symptoms include dyspnea, cough, hemoptysis, and pleural pain; Wheezing and pleural friction noise may be heard.
The severity of respiratory failure directly depends on the degree of vascular occlusion. However, pulmonary manifestations are associated not only with mechanical obstruction of the pulmonary capillaries with fat emboli, which leads to increased pressure in the pulmonary artery, disruption of the perfusion-ventilation ratio, and discharge of unoxygenated blood due to intrapulmonary shunting, but also damage to the endothelium of the pulmonary capillaries due to exposure to free fatty acids, in particular , the most toxic, oleic, which is found in large quantities in the bone marrow of adults. Damage to the endothelium of the pulmonary microvessels and the leakage of fluid, electrolytes and protein into the interstitium leads to its overhydration, decreased elasticity of the pulmonary parenchyma and surfactant synthesis, edema and collapse of the alveoli and the formation of acute respiratory distress syndrome.
Neurological symptoms resulting from cerebral embolism and hypoxic brain injury are often observed in the early stages and usually occur after the development of respiratory failure. Sometimes these symptoms are observed in patients without lung damage. General cerebral symptoms predominate: motor restlessness, development of epileptiform seizures or lethargy, impaired consciousness. Disturbances of consciousness may range from drowsiness and mild irritability to disorientation, stupor and coma.
Both local and generalized convulsions have been described during fat embolism. Focal neurological symptoms, including hemiplegia, aphasia, apraxia, visual disturbances and anisocoria, occur. Neurological symptoms may be transient and reversible. Diagnosis of fat embolism in the presence of traumatic brain injury is particularly difficult.
Petechial rashes of the type of small hemorrhages (1-2 mm) on the skin of the neck, anterolateral surfaces of the chest, inner surfaces of the shoulder, in the armpits (sometimes on the sclera, upper palate) are found in 50-60% of patients. Their occurrence is based on embolism of skin capillaries and coagulation disorders (first, capillaries are overstretched by fat emboli, and then damaged by released fatty acids).
Typically, petechial rashes last from several hours to several days. The presence of petechiae is considered a highly pathognomonic symptom of fat embolism, and the increase in their distribution over time may indicate the severity of the course of PVCs. They appear on days 2-3 (or 12-18 hours after the patient’s condition worsens) and undergo reverse development by the end of 1 week.
When examining the fundus of the eye, retinal damage occurs in 50-60% of cases of PVCs and are combined into Patcher syndrome, described in 1910. These changes include: exudate, edematous plaques, whitish-silver spots of irregular shape such as “cotton balls” located on the fundus near the retinal vessels, often between the nipple and the corpus luteum, perivascular or petechial hemorrhages, intravascular fat globules.
Diagnosis of fat embolism
Intravital PVCs are recognized only in 1-2.2% of cases. In some cases, it passes under the guise of other diseases: pneumonia, acute respiratory distress syndrome, etc. There are currently no specific methods for diagnosing the disease; it is carried out by excluding other possible causes of the developed clinical symptoms.
The most commonly used set of major and minor diagnostic criteria for fat embolism, in which the diagnosis is made if at least one major and four minor signs are present.
Big criteria include:
- axillary or subconjunctival petechiae;
- hypoxemia (paO2<60 mmHg);
- fractional concentration of O2 in the inhaled gas mixture (FiO2>0.4);
- dysfunctions of the central nervous system;
- pulmonary edema.
Small criteria are:
- tachycardia (> 110 per minute);
- fever (temperature above 38.5°C);
- embolism in the retina of the fundus during fundoscopy;
- the presence of fatty droplets in the urine;
- sudden unexplained decrease in hematocrit and platelets, increase in ESR;
- detection of fat droplets in sputum.
SA Schoufeld criteria are also known . They include seven clinical signs, each of which is assigned a score:
- petechial rash - 5;
- diffuse infiltration of the lungs during X-ray examination - 4;
- hypoxemia - 3;
- fever (>38°C) - 1;
- tachycardia (>120 per minute) - 1;
- tachypnea (>30 per minute) - 1;
- disturbances of consciousness - 1.
A score of more than 5 is required to make a diagnosis.
There is a score for the subclinical form of fat embolism according to A. Yu. Pashchuk -
- tachycardia over 90 beats. per minute — 20 points;
- hyperthermia over 38° C - 10 points;
- signs of shock lung syndrome - 20 points;
- change of consciousness - 20 points;
- hyper- or hypocoagulation - 5 points;
- oliguria - 5 points;
- cylindruria - 1 point;
- increase in ESR - 1 point.
With a score of 10-20, a latent form of fat embolism was determined, and with a score of more than 20, a manifest form of fat embolism was determined.
N. M. Borisov et al. proposed a diagnostic scale for fat embolism. With an index value of 20 points, PVCs are diagnosed with an accuracy of 89.3%.
Fat embolism diagnostic scale
Petechiae
- No – 0 points
- Yes – 9
PaO2/FiO2 < 140
- No – 0
- Yes – 6
Fat globules in blood plasma more than 7 microns or more than 5 globules in the field of view
- No – 0
- Yes – 4
State of consciousness according to the Glasgow coma scale < 5 points
- No – 0
- Yes – 2
Mental disorders
- No – 0
- Yes – 2
The alveolar dead space is 18%, or PaCO2 >7.3 kPa
- No – 0
- Yes – 7
Pulmonary artery systolic pressure > 35 mm Hg. Art.
- No – 0
- Yes – 7
Sudden decrease in hematocrit <0.28
- No – 0
- Yes – 5
Sudden decrease in platelet count < 160 x10x9/l
- No – 0
- Yes – 6
Increased body temperature > 38.5 °C
- No – 0
- Yes – 2
Despite the fact that the presence of fat globules in the blood serum in a significant percentage of patients with severe skeletal trauma is not accompanied by the development of fat embolism, these methods continue to be widely used in diagnosis. Normally, fat globules are rare, their diameter does not exceed 2-3 microns. Post-traumatic disturbances of homeostasis lead to an increase in diameter up to 40 microns. The presence of fat globules with a diameter of more than 7-8 microns is a harbinger of clinical manifestations of fat embolism.
There is a special technique (Garda method) for determining fat droplets. Microscopy and dark-field ultramicroscopy are used to detect fat in peripheral blood; fluorescence microscopy; filtration and ultrafiltration. In this case, both conventional (sudan, nil blau sulfate, oil red) and fluorescent (phosphine 3 K) dyes are used to detect fat. There is a method for determining fat globules in the blood of patients using infrared spectroscopy.
More informative is the study of fatty globulemia simultaneously in two vascular areas - in the central vein and the main artery. The need to determine the presence of fat globules in the urine to confirm the diagnosis has not been proven. The determination of the percentage of fat in alveolar macrophages obtained in bronchial washings on the 1st day after injury is also used, which, according to some authors, is an early diagnostic sign of fat embolism. Changes in general and biochemical blood tests and coagulogram are nonspecific and depend on the severity of organ dysfunction.
In severe cases of fat embolism, changes are observed on a plain chest x-ray within 48–72 hours after injury. An X-ray picture similar to a “blizzard” may occur, characteristic of the development of acute respiratory distress syndrome. These changes are the result of the development of pulmonary edema due to increased permeability of the pulmonary endothelium.
The ECG often shows nonspecific changes in the ST-T segment and deviation of the electrical axis to the right, especially in fulminant forms of PVCs. CT scan of the brain allows one to detect petechial microhemorrhages in the gray matter and cerebral cortex, cerebral edema, perivascular infarctions, foci of necrosis and myelin degeneration. MRI can reveal diffuse hyperechoic areas in the white matter and gray matter sulci, in areas of large vascular beds: a “starry sky picture.”
If a fat embolism is suspected, an ophthalmoscopy is required to identify characteristic changes in the retina.
Prevention and treatment of fat embolism
Surgical methods . Early surgical stabilization of fractures in high-risk patients is the most important aspect in the treatment and prevention of the development of fat embolism. Skeletal traction does not provide adequate stability of fragments, therefore the optimal treatment for fractures of long tubular bones, especially with combined injuries, is surgical fixation. Currently, transosseous pin osteosynthesis using pin-rod devices is most often used. It is low-traumatic and blood loss during surgery is minimal.
A number of authors give preference to intramedullary osteosynthesis with a pin. However, this type of osteosynthesis, especially when performed with drilling of the medullary canal, is accompanied by a significant increase in intramedullary pressure, therefore it is often recommended to be performed in a delayed manner.
Drug treatment . Unfortunately, to date, effective drug prevention and treatment of fat embolism have not been proposed, so treatment measures should be aimed at relieving the main clinical manifestations of injury or disease: blood loss, hypovolemia, shock, coagulopathy, acute respiratory failure and others.
Replenishment of blood volume and correction of water-electrolyte balance is carried out depending on the type of dyshydria using colloid and crystalloid solutions. The correct selection of infusion and rheological therapy, eliminating spasm of peripheral vessels, helps reduce the risk of reperfusion complications, which are an important pathogenetic link in fat embolism.
In the absence of the phenomenon of “capillary leakage” and normal indicators of pulmonary vascular permeability, determined by transthoracic thermodilution using Picco+ technology, the use of albumin, which is capable of binding fatty acids and thereby reducing the degree of globulemia, is recommended. A number of authors recommend the use of anticoagulants, in particular heparin, which, along with anticoagulant and disaggregant properties, has the ability to activate plasma lipoproteins and accelerate the enzymatic reactions of triglyceride hydrolysis, thus helping to cleanse the lungs of fat globules.
Multi-level analgesia, differentiated depending on the type of injury, is of great importance in prevention and treatment. Adequate pain relief reduces hypercatecholaminemia, and therefore the concentration of free fatty acids. The use of narcotic analgesics, long-term epidural, retropleural blockade after correction of hypovolemia, conduction anesthesia of the extremities also normalizes microcirculation.
Drug therapy for brain hypoxia and the fight against pathological impulses includes antihypoxants (GHB), opiates, and barbiturates. There is sufficient data on the use of corticosteroids in fat embolism, based on their ability to stabilize cell membranes, inhibit the neutrophil response to fatty acids, inhibit the release of phospholipase A2, arachidonic acid and platelet aggregation. Currently, the use of corticosteroids for the treatment and prevention of PVCs is questioned.
In recent years, many publications have appeared on the use of plasma exchange exchange in the treatment of fat embolism. Exchange plasmapheresis operations normalize hemodynamic parameters, rheological properties of blood, coagulation system, morphological, biochemical and electrolyte composition of blood. The main indications for exchange plasmapheresis for traumatic fat embolism are: progressive deterioration of the condition, disruption of vital body functions, increased activity of the kinin system, changes in lipid metabolism, immune status and ineffectiveness of intensive therapy. Contraindications are: agonal state, severe cardiopulmonary failure, severe concomitant diseases.
Due to the fact that the main target organ for fat embolism is the lungs, respiratory therapy is important. This is one of the few therapeutic interventions that have a high degree of evidence of effectiveness in the treatment of PVCs. In mild cases of PVC, inhalations using a mask and a high flow of oxygen are possible. As respiratory failure progresses, mask CPAP is used, and if it is ineffective, tracheal intubation and mechanical ventilation are required. The selection of ventilation modes should be carried out individually, in accordance with the indicators of gas exchange and biomechanical properties of the lungs.
Drugs for the specific prevention and treatment of fat embolism, aimed at reducing the concentration of fat globules in the blood, include lipostabil and Essentiale, the action of which is aimed at restoring the dissolution of disemulsified fat in the blood. These drugs are recommended for use by almost all domestic authors. However, in studies involving the creation of experimental PVCs, the use of Essentiale N solution did not have a preventive or therapeutic effect.
It is known that in patients who have been injured while intoxicated, fat embolism occurs much less frequently or occurs in a mild or moderate form, since alcohol is able to inhibit serum lipase, being a good emulsifier, and also has anti-ketogenic, sedative and analgesic properties. actions. This is the basis for intravenous administration of 5% ethyl alcohol in a 5% glucose solution for the purpose of preventing and treating PVCs. Experiments on rats have proven that a solution of 5% ethyl alcohol is an effective means of preventing and treating experimental PVC.
In the last decade, publications have appeared indicating the effectiveness of the use of perftoran in fat embolism. It has been shown that early use of perftoran in the complex treatment of patients with severe trauma and blood loss helps to optimize the parameters of central hemodynamics and oxygen status. In addition, the presence of the emulsifier proxanol-286 in perftoran can help reduce the size of fat globules. Its ability to bind lipids, which form the basis of fat globules, has also been proven. These properties of perftoran make it possible to classify it as a specific means of treating PVCs. The use of perftoran for the treatment of PVCs is accompanied by an increase in the proportion of mild degrees of damage to lung tissue by fat emboli and a significant decrease in the number of severe cases of PVCs.
There is evidence of the preventive effect of the drug Hepasol A, which reduces the risk of developing fatty globulemia during surgery and in the postoperative period. The drug Gepasol A stabilizes lipid metabolism and reduces the activity of lipid peroxidation. However, there is no convincing evidence that it improves results in the treatment of fat embolism.
Recently, data have emerged on the preventive effect of sodium hypochlorite, which causes oxidation of the lipid components of the fat globule, the formation of their water-soluble forms, which leads to the destruction of the fat drop itself and a decrease in the severity of fat globulemia.
Conclusion
Thus, the complexity and relevance of the problem of fat embolism becomes obvious, and the mortality rate from this complication remains high. There is still no consensus on the pathogenesis, prevention and treatment of PVCs. Particularly difficult is the early diagnosis of PVCs, due to the lack of a clear clinical picture and pathognomonic symptoms, and laboratory diagnostics are not very specific. Fat embolism is much more common than diagnosed and can occur in any critical condition.
Prevention and treatment regimens vary among different authors. Based on this, it is necessary to highlight the following areas of scientific and practical research:
- development of prognostic criteria for the development of severe forms of PVC;
- development of new directions for the prevention of severe forms of PVC;
- development of an algorithm for diagnosing and treating PVCs;
- individualization (personification) of diagnostic and treatment criteria for PVCs.
V. N. Yakovlev, Yu. V. Marchenkov, N. S. Panova,
V. G. Alekseev, V. V. Moroz
2013
Research methods
A wide range of tests have been proposed for the diagnosis of FES, but none of them has 100% specificity. Laboratory and instrumental studies are usually carried out to confirm a clinical diagnosis or to monitor therapy.
Blood research and biochemistry . Fatty hyperglobulinemia can be considered a pathognomonic sign of FFE. However, in a number of studies, the presence of fat globules was found in the serum of more than 50% of patients with fractures who did not have symptoms suggestive of FES. Unexplained anemia (in 70% of patients) and thrombocytopenia (<150,000/mm3 in 50% of patients) are common.
The concentration of lipids in the blood is not informative for diagnosis, since the level of circulating fats does not correlate with the severity of the syndrome. Hypocalcemia (due to the binding of free fatty acids and calcium) and increased lipase levels are possible.
Abnormalities in coagulation tests may include prolongation of prothrombin and partial thromboplastin times, hypofibrinogenemia, and increased fibrinogen degradation products.
Urine examination . The need to determine the presence of fat globules in the urine to confirm the diagnosis has not been proven.
Arterial blood gases show low partial pressure of oxygen (paO2 - 50 mm Hg or less) and low partial pressure associated with respiratory alkalosis (paCO2).
Chest X-ray . Chest X-ray with FFE shows a “blizzard” picture. Radiological signs may persist for up to three weeks.
CT scan of the chest . As a rule, thickening of the interlobular septa is visible. Centrilobular and subpleural nodules may be present due to alveolar edema, microbleeding, and inflammatory response.
Lung scan . May show ventilation-perfusion mismatch. At the initial stage, the V/Q ratio is often increased.
ECG . As a rule, remains unchanged, with the exception of nonspecific sinus tachycardia. However, nonspecific ST-T segment changes and right axis deviation can be seen in fulminant forms.
Transesophageal echocardiography . It can be used to assess the presence of fat globules during osteosynthesis operations, however, the data obtained do not correlate with the actual development of FFE.
Bronchoalveolar lavage . The use of bronchoscopy and bronchoalveolar lavage to detect fat droplets in alveolar macrophages as a means of diagnosing fat embolism has been described in trauma patients. However, the sensitivity and specificity of diagnostic criteria are unknown.
CT scan of the brain . Performed due to a change in the patient's mental state. Diffuse pinpoint white matter hemorrhages may be seen, consistent with microvascular injury from cerebral fat embolism.
MRI of the brain . Can identify areas of high intensity on T2-weighted images. Useful in patients with neurological symptoms of fat embolism and normal CT images.
Treatment
Therapeutic measures include adequate oxygenation, ventilation, hemodynamic stabilization, infusion of blood products according to clinical indications, and prevention of deep vein thrombosis.
Various drugs have also been proposed for the treatment of FES, but the results are inconclusive.
Corticosteroids . These drugs have been well studied and recommended for the treatment of FES. The proposed mechanism of their action is the reduction of inflammation, reduction of perivascular hemorrhages and edema. There is sufficient evidence for the use of steroid therapy for FES, but experimental studies have not shown much benefit. In addition, there have been no prospective, randomized, or controlled clinical studies that have shown significant benefits of their use.
Aspirin . A prospective study of 58 patients with uncomplicated fractures showed that treatment with Aspirin resulted in significant normalization of blood gases, protein coagulation, and platelet counts compared with controls.
Heparin . The drug is known to stimulate lipase activity and is used to treat FES. However, lipase activation may be potentially harmful if the increase in free fatty acids is considered to be an important part of the pathogenesis. There is also the possibility of an increased risk of bleeding in patients with multiple traumas.
There are studies showing the positive effect of using N-acetylcysteine for the treatment of FFE.
Lipostabil and Essentiale are drugs for restoring the physiological dissolution of disemulsified fat. Their active principle is essential phospholipids. They can correct protein and fat metabolism in the body.
In order to inhibit serum lipase, intravenous administration of 90% alcohol in a 5% glucose solution is recommended, which also has a high calorie content, anti-ketogenic, sedative and analgesic effects.
There is evidence of the preventive effect of the drug Gepasol A , which reduces the risk of developing fat globulinemia during surgery and in the postoperative period. However, there is currently no convincing evidence from multicenter prospective studies that this drug improves the prognosis of FES.
Detoxification and detoxification therapy consists of the use of forced diuresis and plasmapheresis. Ultraviolet and laser irradiation of blood is also recommended.
Treatment of hypoxia and respiratory failure includes the following procedures:
- oxygen inhalation - the initial treatment of hypoxia during FFE is oxygen inhalation using a mask and a high gas flow, with an oxygen content of 50-80%;
- spontaneous breathing with pressure support;
- mechanical ventilation and positive end expiratory pressure (CPAP) support. If FiO2>60% and CPAP>10 cmH2O are required to achieve adequate gas exchange. Art., tracheal intubation is required. CPAP and mechanical ventilation require careful monitoring of arterial blood gases and hemodynamic status.
Surgical methods . Early immobilization of fractures reduces the incidence of FFE. However, there is some difference of opinion regarding the best method for fixation of long bone fractures.
Transosseous osteosynthesis with external fixation devices has a number of advantages due to low trauma and low blood loss during surgery. External osteosynthesis with plates does not have such advantages.
Intramedullary osteosynthesis with a pin, performed with reaming of the medullary canal, is accompanied by a significant increase in intramedullary pressure, but when a hole is placed between the greater and lesser trochanter, transesophageal echocardiography revealed a decrease in fat globulinemia (20 versus 85%).
To limit intraosseous pressure, cementless fixation of femoral prostheses and intramedullary osteosynthesis of the femur without drilling are also used.
External fixation devices and plate osteosynthesis produce less damage to the lungs than intramedullary osteosynthesis.
Prevention
Preventive measures for SFE begin at the prehospital stage. These include: adequate immobilization of injured limbs; gentle transportation with specialized transport, early disaggregant infusion therapy, adequate pain relief, immobilization of fractures.
Replenishing the volume of circulating blood is of great importance. Infusion therapy should be started as early as possible. A good effect was obtained with the infusion of saline solutions, albumin and other colloidal plasma substitutes, in particular hydroxyethyl starch.
Albumin . Recommended for replenishing circulating blood volume, especially in cases of hypoproteinemia, because it not only restores the required volume, but also binds fatty acids and can reduce the degree of lung damage.
Corticosteroids . Their use for prevention is controversial. However, a number of studies show a reduction in the incidence and severity of FFE with prophylactic use of corticosteroids. However, in all the studies showing the beneficial effects of prophylactic steroid use, no significant changes in mortality were noted.