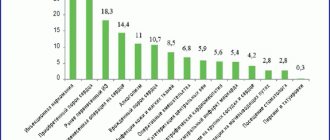
Causes of infective endocarditis
Infectious endocarditis can be caused by various bacteria and microscopic fungi, the biological properties of which allow them to grow and multiply by attaching to the tissues of the heart.
Infective endocarditis is one of the most dangerous cardiac diseases. Mortality even with intensive treatment in a specialized hospital is very high (according to various sources, from 15 to 25%). And if endocarditis is not treated, it is guaranteed to “eat” the heart valves, blood circulation will become impossible and the patient will die.
Routes of infection
The first way is infection of the natural “channels” leading into the body - skin, teeth, urinary tract, female reproductive system. The entry of a microorganism into any blood vessel gives it a chance to travel through the bloodstream to the heart.
The second way is artificial. Any violation of the integrity of the skin and mucous membranes (usually with the help of medical instruments or needles) can lead to infection entering a blood vessel. Hence the increased incidence of infective endocarditis in drug addicts and patients who have undergone various types of surgical interventions - from tooth extraction to operations to replace heart valves. It is clear that the greater the volume of intervention, the higher the potential threat of infection. In this regard, during surgical interventions one or another antibiotic prophylaxis regimen is used.
Symptoms
The disease may develop asymptomatically for some time. It is also characterized by acute and chronic stages. There is an extensive list of symptoms, which makes it difficult to make a correct diagnosis.
The clinical picture of endocarditis is expressed in the following symptoms:
- elevated temperature;
- chills;
- sweating;
- enlarged lymph nodes;
- signs of intoxication (weakness, headaches);
- change in skin color (pallor, spots);
- changing the shape of nails;
- arthritis of large joints;
- damage to the heart valves;
- increased thrombus formation;
- signs of pericarditis;
- systemic damage to organs (kidneys, central nervous system, etc.);
- progressive heart failure.
The manifestation of the disease is individual and depends on the general condition of the patient’s body and the severity of the pathological process.
Clinical picture of the disease
The clinic of infective endocarditis is formed by three components.
The first is septic (when any infection enters the bloodstream, a high temperature, severe weakness, increased heart rate, and disorders of the blood coagulation system develop).
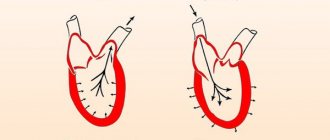
The second component is the manifestation of local infection. Microorganisms form colonies on the inner lining of the heart, most often on the valves - the so-called vegetations. Vegetations can be detected by ultrasound examination of the heart. Sometimes they are not visible with conventional echocardiography, and then an ultrasound examination through the esophagus (similar to gastroscopy, only with a special ultrasound probe) is necessary for diagnosis.
The third component is the consequences of the separation of vegetations from the valves - blockage of blood vessels by vegetations (embolism). Pieces of vegetation can “fly away” into any blood vessels - the brain, heart, kidneys, limbs, lungs, causing the death of the corresponding tissues due to impaired blood flow, which is accompanied by clinical manifestations of damage to a specific organ.
If a patient with a high temperature (fever) of unknown origin lasting more than a week, which does not respond to conventional treatment with antibiotics, has additional symptoms (heart murmurs or disturbances in organs into the vessels of which a torn piece of vegetation has “flown”), examination for the presence of infective endocarditis is necessary .
- Magazine archive /
- 2010 /
Kidney damage and disturbances in the hemostatic system in subacute infective endocarditis
A.A. Demin, V.P. Drobysheva, E.S. Friedman
Department of Hospital Therapy and Clinical Pharmacology, Faculty of Medicine, State Educational Institution of Higher Professional Education “Novosibirsk State Medical University”, Novosibirsk
Purpose of the study. To determine the features of kidney damage (RD) and the role of disturbances in the hemostatic system in the development of RP in subacute infective endocarditis (IE). Material and methods. In 120 patients with subacute IE, blood, urine, serum creatinine levels, parameters characterizing the hemostatic system were examined, and blood and urine cultures were performed. We performed two-dimensional transthoracic and transesophageal echocardiography, color Doppler blood flow mapping, and ultrasound examination of the kidneys. Results. PP was observed in 77% of patients with subacute IE. Changes in urinary sediment were noted in 90.3% of patients, hematuria in 87%, proteinuria in 50%, and leukocyturia in 55%. Chronic renal failure (CRF) developed in 33.3% of patients. Ultrasound examination revealed signs of renal infarction (RI) in 10% of patients. An analysis of 10 fatal cases of subacute IE with PP showed that all deceased patients had glomerulonephritis (GN), more often mesangiocapillary; 6 have IP. In 43 (46.2%) patients, PP was combined with severe hemostasis disorders. Correlation analysis revealed a connection between the parameters of urinary sediment and the hemostatic system. Conclusion. Kidney damage in subacute IE is characterized by the development of urinary syndrome with moderate hematuria, leukocyturia, and proteinuria. Renal failure is a common complication of subacute IE. The most common morphological variant of GN in IE is mesangiocapillary. In subacute IE with kidney damage, more pronounced disturbances are observed in all parts of hemostasis, which is confirmed by data from laboratory research methods. The degree of disturbances in the hemostatic system correlates with the severity of changes in urinary sediment. With an increase in the degree of activity, the role of the vascular component decreases and the importance of disorders of the coagulation component of hemostasis in the development of kidney damage in subacute IE increases.
Key words: disorders in the hemostatic system, infective endocarditis, kidney damage
Read the article in the Doctor's Library
Literature
1. Moreillon P., Que YA Infective endocarditis. Lancet 2004; 363:139–49. 2. Tattevin P., Donal E., Revest M. Can we really achieve a 1-year mortality rate lower than 10% in patients with infective endocarditis? Arch Intern Med 2010; 170(2): 211–12. 3. Alonso-Valle H., Farinas-Alvarez C., Bernal-Marco JM et al. The changing face of prosthetic valve endocarditis at a tertiary-care hospital: 1986-2005. Rev Esp Cardiol 2010; 63(1): 28–35. 4. Chopra T, Kaatz GW. Treatment strategies for infective endocarditis. Expert Opin Pharmacother 2010; 11(3): 345–60. 5. Golovacheva T.V., Skvortsov V.V., Filatova I.I. et al. Infective endocarditis // Current issues in heart and vascular diseases. 2009; 4 (1): 69–82. 6. Tyurin V.P. Infectious endocarditis. M., 2001. 7. Georg DK, Maria K., Thomas B. et al. Complicated infective endocarditis necessitating ICU admission: clinical course and prognosis. Critical Care 2002; 6: 149–54. 8. Kozower BD, Windels MH, Gallagher RC A complicated case of acute bacterial endocarditis. Conn Med 2001; 65(7): 391–93. 9. Mylonakis E., Calderwood SB Infective endocarditis in adults. N Engl J Med 2001; 345(18): 1318–30. 10. Drobysheva V.P. Infectious endocarditis: clinical picture, diagnosis, treatment. Author's abstract. diss. doc. Honey. Sci. Novosibirsk, 2003. 11. Lowes JA, Hamer J., Williams G. et al. Ten years of infective endocarditis at St. Bartholomew's Hospital: Analysis of clinical features and treatment in relation to prognosis and mortality. Lancet 1980; 1: 133–36. 12. Demin A.A. Infectious endocarditis In the book: Oganov R.G. (ed.) Cardiology. Guide for doctors. M., 2004. pp. 728–759. 13. Chipigina N.S., Vinogradova T.L., Timofeev V.T. and others. Kidney damage in infective endocarditis // Clinician. 2008; 4: 16–23. 14. Sinyachenko O.V., Anikeeva T.V., Ignatenko G.A. and others. Glomerulonephritis as a factor determining the severity of infective endocarditis // Nephrology. 2003; 7 (1): 46–50. 15. Brusina E.B., Kolomyshchev A.B., Barabash O.L. and others. Infective endocarditis - evolution of the disease // Ter. archive 2000; 72(9): 47–50. 16. Revilla A., Lopez J., Vilacosta I. et al. Clinical and prognostic profile of patients with infectious endocarditis who need urgent surgery. Eur Heart J 2007; 28:65–71. 17. John L. Brusch. Infective Endocarditis: Management in the era of Intravascular Devices. Informa Healthcare. 2007. 18. Egoh Y., Ogura K., Anbe J. et al. A case report of active infectious endocarditis caused by MRSA with chronic renal failure. Kyobu Geka 1996; 49(8): 677–79. 19. Kessavane A., Marticho P., Zogheib E. et al. Septic coronary embolism in aortic valvular endocarditis. J Heart Valve Dis 2009; 18(5): 572–74. 20. Satsu T., Onoe M., Kajiwara M. et al. Infective endocarditis complicated with ruptured mycotic intracranial aneurysms. Kyobu Geka 2010; 63(1): 82–85. 21. Ulanova V.I. Infective endocarditis: diagnosis, clinical course, treatment // Attending physician. 2003; 6:46–49. 22. Thuny F., Avierinos J. F., Tribouilloy C. et al. Impact of cerebrovascular complications on mortality and neurological outcome during infective endocarditis: a prospective multicentre study. Eur Heart J 2007; 28:1155–61. 23. Di Salvo G., Habib G., Pergola V. et al. Echocardiography predicts embolic events in infective endocarditis. J Am Coll Cardiol 2001; 37:1069–76. 24. Li JS, Sexton DJ, Mick N. et al. Proposed modification to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 2000; 30: 633–38. 25. Demin A.A., Drobysheva V.P. Kidney damage due to infective endocarditis (hematuria) // Therapeutic archive. 1991; 9: 121–25. 26. Mazurov V.I., Ulanova V.I. The course of infective endocarditis in injection drug addicts and persons with predisposing heart diseases // Clinical Medicine 2001; (8): 23–28. 27. Kannan S, Mattoo TK Diffuse crescentic glomerulonephritis in bacterial endocarditis. Pediatr Nephrol 2001; 16:423–28. 28. Majumdar A., Chowdhary S., Ferreira M. et al. Renal pathological findings in infectious endocarditis. Nephrol Dial Transplant 2000; 15: 1782–87. 29. Demin A.A., Drobysheva V.P., Welter O.Yu. Infectious endocarditis in “injection drug addicts” // Clinical medicine. 2000; 8:47–51. 30. Tyurin V.P., Dubinina S.V. Infectious endocarditis in elderly and senile people // Clinical medicine. 2001; 78(4): 53–56. 31. Komarov V.T., Tatarchenko I.P., Savchenko R.P. and others. Clinical and laboratory characteristics of kidney damage in infective endocarditis // Nephrology. 2000; 4:52–57. 32. Mouli S., Ruimy R., Launay O. et al. The changing clinical aspects of infectious endocarditis. Descriptive review of 90 episodes in a French teaching hospital and risk factors for death. J Infect 2002; 45(4): 246–56.
About the authors / For correspondence
Demin A.A. – Professor, Head of the Department of Hospital Therapy and Clinical Pharmacology, Faculty of Medicine, State Educational Institution of Higher Professional Education “NSMU”, Doctor of Medical Sciences. Email; Drobysheva V.P. – Professor of the Department of Hospital Therapy and Clinical Pharmacology of the Medical Faculty of the State Educational Institution of Higher Professional Education “NSMU”, Doctor of Medical Sciences. Tel.; Fridman E.S. – Assistant at the Department of Hospital Therapy and Clinical Pharmacology, Faculty of Medicine, State Educational Institution of Higher Professional Education “NSMU”, Ph.D. Tel.
Similar articles
- HCV-associated cryoglobulinemic vasculitis with severe kidney damage and the development of B-cell lymphoma. Modern possibilities of changing the prognosis using monoclonal antibodies to CD20 and antiviral therapy
- Selective screening for Fabry disease: review of literature data and experience in the Russian Federation
- Kidney damage in Fabry disease: possibilities for radically improving prognosis
- Kidney damage in polycythemia vera as a problem of interdisciplinary interaction
- Heroin and cocaine induced nephropathy
Diagnosis of infective endocarditis
An accurate diagnosis of endocarditis is made by positive blood culture results and reliable visualization of intracardiac vegetations. In all other cases, the diagnosis of endocarditis is made with varying degrees of probability.
The following types of research are used:
- Laboratory diagnostics;
- Electrocardiography (ECG);
- Echocardiography;
- X-ray of the chest organs.
1 Consultation with a MedicCity cardiologist
2 ECG as a method for diagnosing infective endocarditis
3 Full description of the picture
Prevention
Preventive measures to prevent endocarditis include giving up bad habits, paying close attention to health, and timely treatment of emerging infections.
If you have a chronic form of the disease, you should regularly visit a cardiologist and undergo examination.
Endocarditis is a serious heart disease that can occur in both children and adults. Therefore, if your health condition worsens, it is necessary to seek help from a qualified specialist as soon as possible. At the medical center you can undergo a full examination of the body in the shortest possible time. Based on the clinical picture, the doctor will make a diagnosis and prescribe effective treatment.
Treatment of infective endocarditis
Treatment for infective endocarditis begins with high doses of serious antibiotics, usually intravenous. Treatment continues, depending on the specific type of pathogenic microorganism, from two to six weeks. If treatment is ineffective (high temperature, further growth of vegetations according to echocardiography), a decision is made on surgical treatment (the heart is opened, vegetations are cleaned out, and, if necessary, the affected valve is replaced with an artificial one). However, as previously described, treatment is not always successful, and despite medical advances, the mortality rate of infective endocarditis has not been significantly reduced.
Measures to prevent infective endocarditis
If you need any surgical intervention (from tooth extraction to abdominal surgery), be sure to ask your doctor if any action on your part is needed for antibiotic prophylaxis for infective endocarditis (sometimes preventive antibiotic therapy is already included in the hospital treatment plan). If the doctor gives recommendations for taking antibiotics at home, be sure to follow them.
If you accidentally slightly damage the skin (cut), be sure to treat the wound with an antiseptic (alcohol, brilliant green or iodine). If the cut or puncture is deep, you should immediately take an antibiotic (for example, if you are not allergic to penicillin, Augmentin 1 gram once).
At MedicCity you can undergo a comprehensive cardiological examination and treatment of identified cardiovascular diseases. Reception is carried out by highly qualified cardiologists using expert equipment.