Forms of Goodpasture's syndrome
Based on the speed of development of symptoms, two forms of the disease are distinguished:
- rapid progression: renal and pulmonary symptoms predominate;
- death occurs after 11–12 months as a result of pulmonary hemorrhage or renal failure.
- periods of progression alternate with periods of complete absence of symptoms;
Methods of treating the disease
With Goodpasture's syndrome, inflammation of the renal and pulmonary capillaries of immune origin develops, resulting in glomerulonephritis and hemorrhagic pneumonitis. The disease is named after the American pathophysiologist who first described it a little over a hundred years ago. This syndrome is diagnosed predominantly in men, with a frequency of approximately 1:1000000. Lack of timely treatment is associated with an extremely negative prognosis and mortality for the majority of patients.
The causes of the disease have not been precisely clarified, but it has been associated with viral pathologies, including influenza and hepatitis A, long-term use of certain medications, inhalation of gasoline and varnish vapors, and smoking. There is also a hereditary predisposition. The influence of negative factors stimulates the production of autoantibodies to the membranes of the alveoli of the lungs and renal glomeruli. Studies have shown that the development of an autoimmune inflammatory process is largely influenced by the activation of T lymphocytes, proteolytic enzymes and free radicals, and the synthesis of cytokines such as interleukin-1 and platelet-derived growth factor.
There are malignant, moderate and slow variants of the pathology. Clinical signs of the malignant variant include pulmonary hemorrhage and acute renal failure. Moderate and slow variants are manifested by characteristic symptoms of lung damage (cough, shortness of breath, hemoptysis), low-grade fever, weakness, weight loss, and symptoms of renal pathologies (hematuria, swelling of the extremities, increased blood pressure).
Treatment tactics depend on the type of Goodpasture syndrome, the severity of symptoms and the general condition of the patient.
In the acute form of the malignant variant, intensive therapy is carried out:
- artificial pulmonary ventilation (ALV);
- oxygen inhalation;
- blood transfusion;
- hemodialysis;
- replenishment of lost fluid and normalization of water and electrolyte balance.
Patients are also prescribed:
- pulse therapy with methylprednisolone - the patient is briefly administered certain types of glucocorticosteroids in increased doses, which helps reduce the production of autoimmune antibodies and the frequency of developing complications;
- combined pulse therapy - the administration of a combination of corticosteroid hormonal drugs and cytostatic drugs to the patient also has an immunosuppressive effect, after the laboratory and radiological tests return to normal, the patient is transferred to a maintenance regimen of therapy;
- monoclonal antibodies are an innovative method based on the ability of drugs to attach to the CD20 protein expressed on the surface membrane of B-lymphocytes and inhibit their activity, thus renewing the population of lymphocyte cells and stopping tissue destruction by autoimmune antibodies;
- plasmapheresis is a safe way to purify plasma from circulating immune complexes by centrifugation; blood taken from the patient is placed in a centrifuge, where the plasma is separated from the red blood cell mass, which, in combination with plasma replacement solutions, is injected back into the patient’s bloodstream.
- Hemodialysis in Israel
- Plasmapheresis in Israel
Goodpasture's syndrome
The classic triad expressing the clinical and pathogenetic essence of this disease is pulmonary hemorrhage, glomerulonephritis and antibodies to antigens of the main membrane of the capillaries of the lungs and kidneys. The disease is rare and can affect any age, but young men are more often affected. The specific reasons are unknown; The development of Goodpasture's syndrome has been described more than once after recent influenza or inhalation of hydrocarbons. In this regard, it is possible that such influences thus change the chemical structure of the above-mentioned main membrane antigens, such that they acquire autoantigenic properties and cause the production of corresponding antibodies with pathogenic properties.
In kidney tissue, using the immunofluorescent method, linear deposits of antibodies to basement membranes are detected, combined in some cases with deposits of the C3 complement fraction. At the same time, electron microscopic examination does not reveal deposits of immune complexes. Circulating antibodies to the basement membranes of the tubules, glomeruli and pulmonary alveoli are detected in the blood serum in more than 90% of patients (especially in the early stages of the disease), but they do not reflect the severity of organ changes or the overall prognosis, thus having mainly diagnostic value. Serum complement and circulating immune complex levels were normal. On histological examination, the renal glomeruli in some patients may appear normal, but in most cases there is obvious pathology, ranging from focal proliferative changes to necrotizing glomerulonephritis. Extracapillary “crescents” develop most often. In the lungs, hemorrhages are found in the cavity of the alveoli with or without a picture of alveolitis.
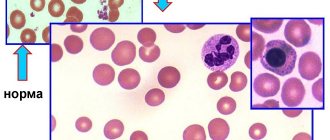
At the onset of the disease, clinical manifestations are associated primarily with damage to the lungs - cough, slight shortness of breath and especially hemoptysis; mild cyanosis is less common. On auscultation, moist rales are possible. Radiologically, infiltrates of varying sizes are characteristic in both lungs, especially in the hilar areas. Macrophages containing iron are usually found in sputum. Increased iron deposition in the lung tissue can be detected by scanning with IgP. Many patients have fever, joint pain, and severe general weakness, but in some cases these symptoms are mild or absent. In most patients, signs of glomerulonephritis are recorded from the first days or weeks of the disease. Blood tests reveal increased ESR and leukocytosis; later, as a result of pulmonary hemorrhages, hypochromic anemia is possible.
The course of the disease is generally unfavorable, although heterogeneous. In the early stages, the main threat is pulmonary hemorrhages, and often the patient dies as a result of the first and only profuse bleeding. A number of survivors of this bleeding may develop a relative remission of the pulmonary process, but in many cases, hemoptysis and pulmonary hemorrhages recur. Kidney damage in some patients remains relatively mild, but in most cases progresses rapidly with the development of oliguric renal failure, leading to death within a few months or even weeks. The average life expectancy for inadequately treated patients is less than six months.
Advantages of treatment in Israel
- Highly qualified specialists with extensive experience in treating rare autoimmune diseases.
- Equipping medical centers with modern equipment.
- Accurate diagnostics using modern techniques.
- Inclusion of progressive methods and the latest medications into a comprehensive treatment program.
- Reasonable prices.
Timely completion of a treatment course can significantly improve the prognosis and eliminate painful symptoms. Don’t waste time, contact the clinic of your choice and start treatment immediately.
- 5
- 4
- 3
- 2
- 1
(0 votes, average: 5 out of 5)
Causes
Causes of Goodpasture's syndrome:
- the cause of the syndrome is unknown, but a direct connection has been identified with bacterial and viral infections, as well as taking certain drugs: immunosuppressive, anti-inflammatory, cytostatics;
- Goodpasture syndrome can develop under the influence of chemical and physical environmental factors (organic solvents, the action of hydrocarbons, varnish vapors, gasoline), against the background of cancer;
- with systematic use of cocaine, cases of the development of this disease have also been described;
- HIV infection;
- The autoimmune cause of the disease is the most common; it involves the production of antibodies to certain structures of the lungs and kidneys.
Symptoms
Symptoms of Goodpasture syndrome include the following:
- the main symptom of the disease is a combination of symptoms of glomerulonephritis with hemoptysis (a sign of the collapse of lung tissue);
- peripheral edema appears (swelling of the face, abdomen, legs);
- anemia is noted;
- progressive chest pain, cough, shortness of breath;
- severe malaise, weakness, weight loss;
- an increase in body temperature is periodically observed;
- eye inflammation;
- decrease in urine volume;
- the appearance of blood in the urine;
- blood pressure rises from 140/90 mm Hg. Art. and higher.
Diagnostics
- analysis of the medical history and complaints - what symptoms appeared and when, whether the patient consulted a doctor, how symptoms changed over time, what examinations and treatments were carried out and what their results were;
- analysis of life history, which clarifies data on the presence of bad habits, chronic diseases and previous diseases;
- analysis of family history, which clarifies whether a similar disease has occurred in relatives (for example, rapidly progressive glomerulonephritis);
- general blood test - will detect any signs of an inflammatory process in the body (a significant increase in the level of erythrocyte sedimentation rate, an increase in the level of leukocytes, a high content of reticulocytes);
- biochemical blood test - will detect an increased level of residual nitrogen and a decrease in serum iron;
- a urine test that will detect the following changes: proteinuria, in which protein is detected in the urine;
- hematuria, in which blood is found in the urine;
- cylindruria;
- As a rule, erythrocytes, leukocytes, erythrocyte and granular casts are found in urine sediment.
Treatment
Treatment for Goodpasture syndrome includes the following:
- early administration of large doses of immunosuppressants and corticosteroids;
- plasmapheresis - for the purpose of immediate removal of antibodies circulating in the blood (this is a procedure during which a portion of blood is taken from the patient, from which plasma is removed, and then the blood cells are returned back to the vessels);
- hemodialysis, which purifies and filters blood outside the body;
- symptomatic therapy, which includes the administration of iron supplements and repeated blood transfusions.
Complications
If a patient is diagnosed with Goodpasture syndrome, currently all available treatment methods cannot provide a complete cure or prevent exacerbation:
- in many ways, the prognosis of the syndrome remains extremely unfavorable;
- development of acute renal failure;
- repeated pulmonary hemorrhages;
- death.