Lisinopril: active ingredients
The name of the drug is identical to its active substance - lisinopril dihydrate. Separately, you can find the drug under other trade names. As a rule, its cost under other names is significantly higher.
The following can be used as auxiliary components by various manufacturers:
- corn starch or pregelatinized;
- calcium hydrogen phosphate;
- mannitol;
- magnesium stearate;
- colloidal silicon dioxide;
- microcrystalline cellulose;
- talc.
The drug is produced in the form of oblong white tablets. Its edges are rounded and there is a risk in the center. Each tablet contains 5 mg, 10 mg or 20 mg of active ingredient. The medicine is packaged in 10 tablets in a blister. The package contains 30 doses (3 blisters).
Lisinopril analogs
The original Lisinopril has an affordable price, but there are still many generics (analogs of the drug from different manufacturing countries) on the market.
Substitutes (synonyms) for Lisinopril in Russia
- Lisinopril-Ratiopharm;
- Diroton (Hungary);
- Diropress (Germany, Slovenia);
- Iruzid (Croatia);
- Ko-Diroton (Poland, Hungary);
- Lysigamma (Germany);
- Rileys-Sanovel (Türkiye);
- Scopril (Macedonia);
- Equator (Hungary, Russia).
Lisinopril is available in the form of tablets of 5, 10 and 20 mg.
There are also many medications on the market that combine Lisinopril with other groups of antihypertensive substances:
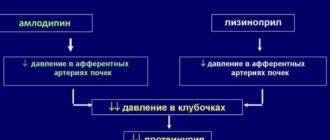
- with Amlodipine (Equator, Tenliza);
- with Hydrochlorothiazide (Co-Diroton, Lisinopril-H,HL, Lizoretik);
- with Indopamide (Diroton-Plus).
Such combinations were created to simplify the regimen and reduce the number of tablets, which increases the likelihood of systematic use of the drug.
How does Lisinopril work?
The drug acts on the renin-angiotensin system of the heart, interfering with dilatation of the left ventricle. At the same time, there is a decrease in the load on the myocardium. The substance reduces pressure in the capillaries of the lungs, as well as in peripheral vessels. When treated with Lisinopril, the tolerance of the cardiac myocardium to increased stress increases. In addition, the activity of renil in plasma increases.
After taking a single dose, the first positive effect occurs after 50-60 minutes. The manifestation of the therapeutic effect intensifies within 7 hours and persists throughout the day. Therapy lasting for several weeks achieves the maximum possible hypotensive effect.
Eating does not interfere with the absorption of the active substance, but at the same time does not contribute to it. Therefore, taking the medicine does not depend on the time of eating. Absorption of Lisinopril reaches 25%. The drug molecules bind weakly to blood proteins. Half-life occurs after 12 hours. Substances are excreted unchanged by the kidneys. Lisinopril does not form metabolites.
conclusions
Lisinopril is a long-acting ACE inhibitor that is highly effective. The drug is considered the “gold standard” in the treatment of hypertension and circulatory failure (together with diuretics, statins, angiotensin-II antagonists and Ca2+ channel blockers). The combined use of Lisinopril and Indapamide reduces the likelihood of recurrent episodes of ischemic stroke by 29% and intracranial hemorrhage by 50%.
It is worth remembering that the antihypertensive effect reaches a plateau no earlier than 10-14 days from the start of treatment.
Before using the drug, you must carefully read the instructions! Lisinopril should not be taken without a doctor’s prescription, and you should not replace it with an analogue yourself.
What is lisinopril prescribed for?
The name of the drug suggests that it belongs to the so-called group of “by-catch”, the action of which is primarily aimed at lowering blood pressure in the fight against hypertension. However, a doctor may prescribe treatment with Lisinopril in other cases:
- for chronic heart failure;
- in acute myocardial infarction not accompanied by arterial hypotension;
- to combat nephropathy of diabetic etiology, both type 1 and type 2.
- with arterial hypertension.
Self-administration of the drug is unacceptable. The dose, frequency of doses and duration of treatment are determined only by the doctor.
Possible side effects
Like other medicines, lisinopril can cause side effects, although not everyone gets them.
Tell your doctor immediately if you notice any of the following effects.
- Severe allergic reactions (rare, affecting 1-10 in 10,000 people).
Symptoms may include sudden onset:
- Swelling of the face, lips, tongue, or throat. This may cause difficulty swallowing.
- Severe or sudden swelling of the arms, legs, and ankles.
- Difficulty breathing
- Severe itching of the skin (with blisters).
- Severe skin problems such as a sudden, unexpected rash or burning, redness or peeling of the skin (very rare, affecting less than 1 in 10,000 people).
- Infection with symptoms such as fever and severe deterioration of general condition, or fever with local symptoms of infection such as sore throat/pharynx/mouth or urinary problems (very rare, affecting less than 1 in 10,000 people).
Other side effects:
Common (occurs in 1-10 out of 100 people)
- Headache
- Feeling dizzy, especially when standing up suddenly.
- Diarrhea
- Dry cough that doesn't go away.
- Vomit
- Kidney problems (confirmed by a blood test)
Uncommon (occurs in 1-10 out of 1,000 people)
- Mood changes
- Change in color of fingers or toes (pale blue accompanied by redness) or numbness or tingling in fingers or toes.
- Change in taste sensations
- Drowsiness
- Dizziness (vertigo)
- Sleep problems
- Stroke
- Cardiopalmus
- Runny nose
- Nausea
- Abdominal pain or indigestion
- Skin rash or itching
- Lack of erection (impotence)
- Feeling tired or weak (loss of strength)
- Excessive low blood pressure may occur in people with the following conditions: coronary heart disease, narrowing of the aorta (heart artery), renal artery, or heart valves; increase in the thickness of the heart muscle. If this happens to you, you may feel dizzy, especially if you stand up suddenly.
- Changes in blood test values that show the functional state of the liver and kidneys.
- Heart attack
- Visual and auditory hallucinations
Rare (affects 1-10 in 10,000 people)
- Confusion
- Skin rash (urticaria)
- Dry mouth
- Hair loss
- Psoriasis (skin problem)
- Impaired sense of smell
- Breast enlargement in men
- Changes in some cells or other elements of the blood. Your doctor may need to take blood samples periodically to check whether lisinopril has any effect on your blood composition. Signs of an effect may include feeling tired, pale skin, sore throat, high temperature (fever), joint and muscle pain, swelling of the joints or glands, or sensitivity to sunlight.
- Low sodium levels in the blood (symptoms may include: fatigue, headache, nausea, vomiting).
- Sudden renal failure.
Very rare (affects less than 1 in 10,000 people)
- Sinusitis (pain and congestion behind the cheek and eyes).
- Wheezing
- Low blood sugar (hypoglycemia). Symptoms: feeling hungry or weak, sweating and rapid heartbeat.
- Pneumonia. Symptoms: cough, feeling short of breath and high temperature (fever)
- Yellowing of the skin or whites of the eyes (jaundice)
- Inflammation of the liver. May cause loss of appetite, yellowing of the skin and eyes, and dark urine
- Inflammation of the pancreas. It causes moderate to severe stomach pain
- Severe skin damage. Symptoms include: redness, blistering and peeling
- Sweating
- Oliguria or anuria
- Liver failure
- Swelling
- Intestinal inflammation
Unknown (frequency cannot be estimated from available data)
- Symptoms of depression
- Fainting
Side effects in children were comparable to those in adults.
If you experience any side effects, talk to your doctor or pharmacist. This also applies to side effects not listed in this leaflet.
Reporting Adverse Events
If you notice any side effects, tell your doctor, pharmacist or pharmacist, including any side effects not listed in this leaflet. You can also report side effects by going to the website www.arpimed.com and filling out the appropriate form “Report a side effect or ineffectiveness of a drug” and to the Scientific Center for Expertise of Medicines and Medical Technologies named after. Academician E. Gabrielyan by going to the website www.pharm.am to the “Report a side effect of a drug” section and fill out the form “Card of reporting a side effect of a drug.” Scientific center hotline phone number: +37410200505; +37496220505 By reporting side effects, you help gather more information about the safety of this drug.
How to store Lisinopril
- Lisinopril, 5 mg tablets.
The drug should be stored out of the reach of children, protected from moisture and light at a temperature of 150C -250C.
- Shelf life – 3 years. Do not take lisinopril after the expiration date indicated on the drug package. When indicating the expiration date, we mean the last day of the specified month.
- Medicines should not be disposed of in wastewater or sewer systems. Ask your pharmacist how to dispose of a drug you no longer need. These measures are aimed at protecting the environment.
Package contents and additional information
One tablet of Lisinopril 5 mg contains:
active substance: lisinopril (in dihydrate format) – 5 mg
excipients: sodium starch glycolate, microcrystalline cellulose, magnesium stearate.
What Lisinopril looks like and contents of the pack:
Lisinopril 5 mg tablets: Round, flat, white or almost white tablets with a score on one side and a bevel on both sides, odorless.
Cardboard packaging containing 24 tablets (1 blister of 24 tablets) along with an insert.
Vacation conditions
Available with prescription
Contraindications to the use of Lisinopril
Contraindications to the use of Lisinopril are pregnancy and breastfeeding. If the expectant mother suffers from hypertension, her condition is monitored in a hospital setting. High blood pressure in such cases is corrected with safe doses of diuretics.
If replacing the drug during breastfeeding is not possible, you should definitely transfer the child to artificial feeding or feeding with donor milk.
Other contraindications are:
- excess potassium in the blood;
- renal dysfunction;
- gout;
- renal artery stenosis;
- elderly age;
- cerebrovascular insufficiency;
- hypotension;
- childhood;
- tissue obstruction that interferes with normal outflow;
- availability of a donor kidney.
Lisinopril: instructions for use
The drug is taken once a day. It is important to observe the time interval between medication doses. Superimposing the effect of one dose on another threatens severe hypotension, up to loss of consciousness.
If the first tablet was taken at lunch, then the second tablet should not be taken in the morning hours of the next day. It is important to keep taking your medication at lunchtime.
A single dose is prescribed by the attending physician based on the following studies:
- blood pressure conditions;
- heart function;
- vascular health;
- risk factors.
If an increase in the single dose is not required, as a rule, a single dose of 2.5 mg of Lisinopril is sufficient to normalize the patient's condition. Dose adjustments can be made no earlier than after 4 weeks of continuous use of the drug, since it is after this time that the maximum possible therapeutic effect is achieved.
If increasing the dose does not give the required result, a similar drug from a different pharmacological group is prescribed, the action of which in a different way will help normalize blood pressure.
If treatment of an insulin-dependent patient is required, Lisinopril is taken under the strict supervision of a specialist in a hospital setting.
Fixed combination of lisinopril and hydrochlorothiazide in the treatment of arterial hypertension
It should be remembered that the simultaneous prescription of several antihypertensive drugs increases the likelihood of non-compliance with the drug regimen (especially in the elderly and in patients suffering from several chronic diseases requiring drug therapy). An alternative to complex therapeutic regimens are fixed combinations of drugs. The use of such combination drugs significantly increases adherence to treatment and, as a result, increases the effectiveness of antihypertensive therapy [4]. Among combination antihypertensive drugs, one of the most common are tablets containing an angiotensin-converting enzyme (ACE) inhibitor and a thiazide diuretic (most often hydrochlorothiazide). The components of this combination affect different parts of the pathogenesis of hypertension. Thus, the antihypertensive effect of ACE inhibitors is based on their ability to suppress the activity of angiotensinogen-I-converting enzyme, thereby reducing the activity of the renin-angiotensin-aldosterone system. ACE inhibitors reduce the formation of circulating and tissue angiotensin II, thereby weakening its vasoconstrictive and proaggregant effects (decreasing the release of endothelin from the endothelium and increasing the content of vasodilating agents in the blood - bradykinin and prostacyclin), and also reducing the secretion of aldosterone. Thus, the basis of the antihypertensive effect of ACE inhibitors is not only their effect directly on the regulation of vascular tone and the volume of circulating blood, but also indirectly - through the improvement of the rheological parameters of the latter, such as viscosity, aggregation activity of platelets and erythrocytes. Thiazide diuretics reduce the reabsorption of sodium, potassium, chlorine, magnesium ions, as well as water molecules in the distal nephron (at the same time, the excretion of calcium ions and uric acid is delayed), thus increasing the amount of urine excreted. It is believed that increased natriuresis leads to a decrease in circulating plasma volume, reduces venous return to the heart, and reduces cardiac output and peripheral vascular resistance. In addition, the hypotensive effect of thiazide diuretics may be associated with a decrease in the reactivity of the cardiovascular system to the effects of circulating catecholamines [2]. Among the numerous representatives of ACE inhibitors, the leading position is occupied by lisinopril, a lysine analogue of enalaprilic acid [7]. Unlike most other representatives of the pharmacological group under consideration, lisinopril is not a prodrug, does not undergo biotransformation in the liver and is excreted unchanged by the kidneys. The drug has fairly variable bioavailability - from 6 to 60% (on average about 25%). In elderly patients, an increase (approximately 2 times) in the concentration of lisinopril in the blood and AUC is noted compared to younger patients. The complete absorption of the drug does not depend on food intake. Lisinopril is not lipophilic, practically does not bind to plasma proteins, penetrates to a small extent through the blood-brain barrier and does not accumulate in tissues (primarily in adipose tissue). The maximum serum concentration is reached after approximately 6–7 hours and persists for 24 hours. The half-life is 12 hours. Decreased renal function slows down elimination, but the slowdown becomes clinically significant only when the glomerular filtration rate decreases below 30 ml/min. [5]. The hypotensive effect begins an hour after oral administration, the peak effect develops after 4–6 hours, and the duration of action reaches 24 hours, which provides a convenient administration regimen - once a day. Hydrochlorothiazide is also currently one of the most widely used thiazide diuretics. The drug is absorbed quite quickly, but not completely, from the gastrointestinal tract; in the blood it is 40–60% bound to proteins. Penetrates through the hematoplacental barrier and into breast milk. Excreted by the kidneys. The diuretic effect of the drug develops within 30–60 minutes, reaches a maximum after 4–6 hours and persists for 6–12 hours [3]. The hypothetical effect of hypothiazide becomes noticeable after 3–4 days of therapy, and the optimal antihypertensive effect in most cases develops after 3–4 weeks. taking the drug regularly. The high effectiveness of lisinopril in hypertension has been proven in a number of controlled studies. It has been established that in its hypotensive effect, lisinopril is not inferior or superior to other ACE inhibitors (captopril, enalapril, quinapril) [13,15,40], calcium antagonists (nifedipine, felodipine, isradipine) [16,21,34], beta-blockers (atenolol, metoprolol, nebivolol) [10,35,39] and angiotensin II receptor blockers (candesartan, valsartan) [25,31]. It should be noted that the vast majority of the above studies indicate that lisinopril is well tolerated and that it is rarely discontinued due to adverse events. It is now considered proven that lisinopril not only effectively lowers blood pressure, but also has a protective effect on the target organs of arterial hypertension. In particular, the multicenter study SAMPLE (Study on Ambulatory Monitoring of Blood Pressure and Lisinopril Evaluation) found that the use of lisinopril leads to regression of left ventricular hypertrophy [27,33]. Similarly, the comparative randomized controlled trial ELVERA (Effects of amlodipine and lisinopril on Left Ventricular mass) demonstrated a significant reduction in left ventricular mass and improvement in diastolic function during long-term (median follow-up 2 years) treatment with lisinopril [42]. Finally, in the randomized CALM (Candesartan And Lisinopril Microalbuminuria study) study, it was found that lisinopril reduces urinary albumin excretion in patients with arterial hypertension and diabetes mellitus [31]. A modern antihypertensive drug should not only effectively reduce blood pressure, but also have a positive effect on long-term prognosis, reducing the risk of cardiovascular events and reducing mortality. Thus, a multicenter randomized open masked study STOP-hypertension 2 (Swedish Trial in Old Patients with Hypertension 2) showed no differences between ACE inhibitors (lisinopril, enalapril), beta-blockers (atenolol, metoprolol CR, pindolol), diuretics (hydrochlorothiazide, amiloride ) and calcium antagonists (felodipine, isradipine) for their effect on reducing the risk of myocardial infarction, stroke and reducing overall mortality in elderly patients with arterial hypertension [19]. The results of the well-known large-scale controlled trial ALLHAT (Antihypertensive and Lipid-Lowering Treatment to prevent Heart Attack Trial) indicate no significant differences in the ability to prevent the primary composite endpoint (myocardial infarction and death from cardiovascular causes) and the effect on overall mortality between lisinopril, amlodipine, chlorthalidone and doxazosin [9]. The hypotensive effect of hydrochlorothiazide and its effectiveness in preventing cardiovascular events have also been confirmed by the results of many controlled clinical trials. One of the earliest placebo-controlled studies, MRFIT (Multiple Risk Factor Intervention Trial), found that long-term therapy with hydrochlorothiazide significantly reduces the incidence of myocardial infarction in patients with hypertension [32]. The placebo-controlled STOP-Hypertension (Swedish Trial in Old Patients with Hypertension) study showed that hydrochlorothiazide therapy effectively reduces blood pressure in elderly patients, and also reduces the risk of cardiovascular, cerebrovascular and all-cause mortality [12]. In the randomized clinical trial HAPPHY (Heart Attack Primary Prevention in Hypertension trial), it was found that hydrochlorothiazide is comparable to beta-blockers (atenolol, metoprolol) in its hypotensive effect, as well as in its beneficial effect on overall mortality, the incidence of coronary and cerebrovascular events [44] . It has also been established that hydrochlorothiazide is as effective in lowering blood pressure as modern drugs from the group of angiotensin II receptor blockers candesartan (ALPINE study [24]) and telmisartan (ARAMIS study [28]). The combined use of lisinopril and hydrochlorothiazide (in the form of separate tablet dosage forms) for the correction of arterial hypertension is highly effective [11,37]. However, of particular interest are studies that examined the effect of a fixed combination of these pharmacological agents. It should be noted that this combination is very favorable from the point of view of clinical pharmacology. Studies conducted on healthy volunteers [41] and in elderly patients with hypertension and impaired renal function [22] showed that lisinopril and hydrochlorothiazide, contained in one tablet, do not interact with each other and do not change the pharmacokinetic characteristics of each other . The results of the studies indicate the high effectiveness of such drugs [26]. In particular, Gerc V. et al. It was found that tablets containing lisinopril and hydrochlorothiazide normalize blood pressure in 81.5% of patients with mild to moderate arterial hypertension [18]. According to Vegazo Garcia O. et al., a fixed combination of lisinopril and hydrochlorothiazide in more than half of the cases can persistently reduce blood pressure to normal levels in patients with high arterial hypertension, poorly controlled by other drugs [43]. It has been established that the combination in question has a protective effect on the target organs of arterial hypertension. Already after 12 weeks. Taking a fixed combination of lisinopril and hydrochlorothiazide reduces left ventricular hypertrophy [17]. In addition, against the background of this therapy, normalization of lipid and carbohydrate metabolism parameters is noted [43]. The fixed combination of lisinopril and hydrochlorothiazide has a more pronounced hypotensive effect than each of the components separately [20,23,36]. Several studies have compared the effectiveness of the fixed combination of lisinopril and hydrochlorothiazide with other combination drugs. It has been established that drugs containing 10 mg of lisinopril and 12.5 mg of hydrochlorothiazide are comparable in their hypotensive effect to dosage forms containing 8 mg of candesartan cilexetil and 12.5 mg of hydrochlorothiazide [29]. According to other studies, the combination of 20 mg of lisinopril and 12.5 mg of hydrochlorothiazide provides more stable control of blood pressure during the day than the combination of 50 mg of captopril and 25 mg of hydrochlorothiazide [30,38], and has a comparable hypotensive effect with fixed combinations of atenolol 100 mg + chlorthalidone 25 mg" and "verapamil 180 mg (in sustained release dosage form) + trandolapril 2 mg". In all studies described, the tolerability of the combination of lisinopril with hydrochlorothiazide was comparable to that of other combinations of antihypertensive drugs. Thus, a fixed combination of lisinopril and hydrochlorothiazide (on the domestic market this combination is represented by the drug “Co-Diroton”® (Gedeon Richter)) can be used as initial therapy in patients with mild and moderate arterial hypertension [6], in persons with severe left ventricular hypertrophy, excess weight and carbohydrate metabolism disorders [4]. In addition, the combination drug in question can be successfully used for high arterial hypertension, refractory to other antihypertensive drugs. Favorable tolerability profile and possibility of administration 1 time/day. make the fixed combination of lisinopril and hydrochlorothiazide a very valuable tool in the hands of a practicing cardiologist. Literature 1 Belousov Yu.B., Leonova M.V., Belousov D.Yu., et al. Results of a pharmacoepidemiological study of patients with arterial hypertension in Russia (PITHAGORUS II). Qualit Clinical Practice 2004;1:17–27. 2 Galyavich A.S. Fixed combinations of antihypertensive drugs. Consilium Medicum 2011 13; 1:24–27. 3 Hydrochlorothiazide: instructions and use. https://www.rlsnet.ru/ mnn_index_id_89.htm 4 Karpov Yu.A. New recommendations on arterial hypertension RMOAG/VNOK 2010: issues of combination therapy. Russian Medical Journal 2010; 18 (22): 1290–1297. 5 Lisinopril: instructions and use. https://www.rlsnet.ru/ mnn_index_id_1758.htm 6 Russian Medical Society for Arterial Hypertension (RMAS), All-Russian Scientific Society of Cardiologists (VNOK). Diagnosis and treatment of arterial hypertension. Russian recommendations (fourth revision), 2010. Systemic hypertension 2010; 3:5–26. 7 Savenkov M.P., Ivanov S.N., Solomonova L.A., Savenkova A.M., Ivanova S.V. Selection of a fixed combination of lisinopril and hydrochlorothiazide in the treatment of arterial hypertension. Russian Medical Journal 2011; 19(4): 196–199. 8 2007 Guidelines for the management of arterial hypertension. The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2007; 28:1462–1536. 9 ALLHAT Officers and Coordinators Major outcomes in high–risk hypertensive patients randomized to angiotensin–converting enzyme inhibitor or calcium channel blocker vs diuretic. JAMA 2002;288:2981–97. 10 Barenbrock M., Spieker C., Hoeks AP, et al. Effect of lisinopril and metoprolol on arterial distensibility. Hypertension. 1994; 23(1 Suppl):I161–3. 11 Chrysant SG Antihypertensive effectiveness of low-dose lisinopril-hydrochlorothiazide combination. A large multicenter study. Lisinopril–Hydrochlorothiazide Group. Arch Intern Med. 1994; 154(7): 737–43. 12 Dahlof B., Hansson L., Lindholm L.H., et al. Swedish trial in old patients with hypertension (STOP–Hypertension): analyzes performed up to 1992; Clin Exp Hypertens 1993;15:925–39. 13 De Cesaris R., Ranieri G., Andriani A., et al. . Minerva Med 1990;81(7–8):541–6. 14 de Leeuw PW, Notter T., Zilles P. Comparison of different fixed antihypertensive combination drugs: a double-blind, placebo-controlled parallel group study. J Hypertens 1997;15(1):87–91. 15 Diamant M., Vincent HH Lisinopril versus enalapril: evaluation of through: peak ratio by ambulatory blood pressure monitoring. J Hum Hypertens 1999;13(6):405–12. 16 Fagard R., Bielen E., Staessen J., et al. Response of ambulatory blood pressure to antihypertensive therapy guided by clinic pressure. Am J Hypertens 199; 6(8):648–53. 17 Gerc V., Begovic B., Vehabovic M., et al. Effects of fixed combination of lisinopril plus hydrochlorothiazide on regression of left ventricular hypertrophy in patients with essential hypertension: an opened, multi–centre, prospective clinical trial. Bosn J Basic Med Sci 2008;8(3):214–9. 18 Gerc V., Begovic B., Vehabovic M., et al. Fixed combination lisinopril plus hydro-chlorothiazide in the treatment of essential arterial hypertension: an opened, multi-centre, prospective clinical trial. Bosn J Basic Med Sci. 2007;7(4):377–82. 19 Hansson L., Lindholm L.H., Ekbom T., et al. Randomized trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension–2 study Lancet 1999;354:1751–6. 20 Hart W. Lisinopril–hydrochlorothiazide combination compared with the monocomponents inelderly hypertensive patients. J Hum Hypertens. 1991;5 Suppl 2:85–9. 21 Jensen HA Efficacy and tolerance of lisinopril compared with extended release felodipine in patients with essential hypertension. Danish Cooperative Study Group. Clin Exp Hypertens 1992;14(6):1095–110; 22 Laher MS, Mulkerrins E, Hosie J, et al. The effects of age and renal impairment on the pharmacokinetics of co-administered lisinopril and hydrochlorothiazide. J Hum Hypertens. 1991;5 Suppl 2:77–84. 23 Lang H. The results of a large multicentre study comparing low-dose lisinopril-hydrochlorothiazide with the monocomponents. J Hum Hypertens. 1991;5 Suppl 2:73–6. 24 Lindholm LH, Persson M, Alupovic P, et al. Antihypertensive treatment and Lipid Profile In a North of Sweden Efficacy evaluation. J Hypertens 2003;21:1563–74 25 Malacco E, Santonastaso M, Vari NA, et al. Comparison of valsartan 160 mg with lisinopril 20 mg, given as monotherapy or in combination with a diuretic, for the treatment of hypertension: the Blood Pressure Reduction and Tolerability of Valsartan in Comparison with Lisinopril (PREVAIL) study. Clin Ther 2004;26:855–65 26 Mancia G, Grassi G. Antihypertensive effects of combined lisinopril and hydrochlortiazide in elderly patients with systolic hypertension: results of multicenter trial. J.Cardivasc.Pharmacol. 1997, 30(5) 548–553. 27 Mancia G., Zanchetti A., Agabiti-Rosei E., et al. Ambulatory blood pressure is superior to clinic blood pressure in predicting treatment–induced regression of left ventricular hypertrophy. Circulation 1997;95:1464–70. 28 Manolis AJ, Reid JL, de Zeeuw D., et al. Angiotensin II receptor antagonist telmisartan in isolated systolic hypertension (ARAMIS) study: efficacy and safety of telmisartan 20, 40 or 80 mg versus hydrochlorothiazide 12.5 mg or placebo. J Hypertens 2004;22:1–5. 29 McInnes GT, O'Kane KP, Istad H, et al. Comparison of the AT1–receptor blocker, candesartan cilexetil, and the ACE inhibitor, lisinopril, in fixed combination with low dose hydrochlorothiazide in hypertensive patients. J Hum Hypertens. 2000 Apr;14(4):263–9. 30 Milon H., Baleydier A. . Therapie. 1997; 52(3):195–205. 31 Mogensen CE, Neldan S, Tikkanen I, et al. Randomized controlled trial of dual blockade of renin–angiotensin system in patients with hypertension, microalbuminuria, and non–insulin dependent diabetes: the candesartan and lisinopril microalbuminuria (CALM) study BMJ 2000;321:1440–4. 32 MRFIT research group. Multiple Risk Factor Intervention Trial. Risk factor changes and mortality results. JAMA 1982;248:1465–77. 33 Omboni S., Fogari R., Palatini P., et al. Reproducibility and clinical value of the through–to–peak ratio of the antihypertensive effect. Evidence from a sample study Hypertension 1998;32:424–9. 34 Os I., Bratland B., Dahlof B. at al. Lisinopril or nifedipine in essential hypertension? A Norwegian multicenter study on efficacy, tolerability and quality of life in 828 patients. J Hypertens 1991; 9(12): 1097–104 35 Pannier BE, Garabedian VG, Madonna O., et al. Lisinopril versus atenolol: decrease in systolic versus diastolic blood pressure with converting enzyme inhibition. Cardiovasc Drugs Ther. 1991; 5(4):775–81. 36 Pathe M. Lisinopril–hydrochlorothiazide combination vs lisinopril for the treatment of hypertension. J Hum Hypertens. 1991 Dec;5 Suppl 2:53–4. 37 Pool JL, Gennari J., Goldstein R. ea Controlled multicenter study of the antihypertensive effects of lisinopril, hydrochlorthiazide and lisinopril plus hydrochlorthiazide in the treatment of 349 patients with mild to moderate hypertension. J.Cardiovasc.Pharmacol. 1987 9(suppl.3) S 36–54. 38 Rappelli A. Controlling hypertension: lisinopril–hydrochlorothiazide vs captopril–hydrochlorothiazide. An Italian multicentre study. J Hum Hypertens. 1991 Dec;5 Suppl 2:55–7; discussion 57–8. 39 Rosei E. A., Rizzoni D., Comini S. et al. Evaluation of the efficacy and tolerability of nebivolol versus lisinopril in the treatment of essential arterial hypertension: a randomized, multicentre, double-blind study. Blood Press Suppl. 2003; 1:30–5. 40 Rumboldt Z., Simunic M., Bagatin J., et al. Controlled multicentre comparison of captopril versus lisinopril in the treatment of mild–to–moderate arterial hypertension. Int J Clin Pharmacol Res. 1993;13(1):35–41. 41 Swaisland AJ The pharmacokinetics of co-administered lisinopril and hydrochlorothiazide. J Hum Hypertens. 1991;5 Suppl 2:69–71. 42 Terpstra WF, May JF, Smit AJ Long–term effects of amlodipine and lisinopril on left ventricular mass and diastolic function in elderly, previously untreated hypertensive patients: the ELVERA trial J Hypertens 2001;19:303–9 43 Vegazo Garcia O., Llisterri Caro JL, Jimenez Jimenez FJ, et al... Aten Primaria. 2003 28;31(3):163–9. 44 Wilhelmsen L., Berglund G., Elmfeldt D. et al Beta-blockers versus diuretics in hypertensive men: main results from the HAPPHY trial J Hypertens 1987;5:561–72.