Hemorrhagic rash can be the cause of various diseases. It occurs as a result of capillaries rupturing and red blood cells leaking out of the vessels. Most often, the rashes do not rise above the surface of the skin and cannot be felt. The exception is inflammation of the capillary walls.
Such pathology can be expressed in a variety of forms, each of which has certain distinctive features. If any rash occurs, you should immediately consult a doctor, who will determine the underlying cause and prescribe the correct treatment.
Features of the rash
A hemorrhagic rash, a photo of which is in the article, refers to the formation of small non-inflammatory rashes on the skin of different parts of the body. This is how the body reacts to the rupture of capillaries, the subsequent penetration of red blood cells into the upper layers of the skin.
When it appears, a person does not experience any discomfort at all, since the rash does not itch and does not cause pain. When pressing on the affected area, the color of the rash does not change. The number of points largely depends on the cause of the lesion and the severity.
In a child under 5 years of age, the disease can be triggered by vascular pathologies, and in a child from 5 to 15 years old - by colds and infectious diseases. In addition, the hereditary factor is important.
What kind of disease is this
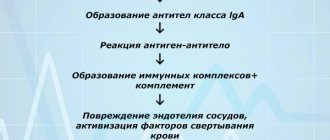
This disease is of an infectious-allergic nature: the main cause of hemorrhagic vasculitis is the presence in the blood of patients of immune complexes and active components of the protective system of proteolytic enzymes. Immune complexes accumulate in the bloodstream, and with an excessive amount of antigens or a lack of antibodies, protein formations are deposited on the endothelium of the microvascular wall. Factors contributing to the development of the disease are:
- bacterial and viral respiratory infections suffered 2-4 weeks before the onset of the disease, which account for up to 60-80% of all cases of the disease;
- foci of chronic infection (sinusitis, tonsillitis, caries, etc.);
- some medications, mainly of antibiotic action;
- potentially allergenic foods (strawberries, citrus fruits, chocolate, eggs, etc.);
- administration of a vaccine or serum;
- hypothermia and dampness or prolonged exposure to the sun.
There is evidence of a hereditary predisposition to the disease. In some cases, it is impossible to find out which factor served as the “trigger” for the patient’s body.
Classification
According to the nature of the spread, hemorrhagic rash is divided into primary and secondary. Primary is characterized by the fact that spots form on clean skin. It is divided into cavity and cavityless. The secondary form is a consequence of the development of elements of the primary rash.
According to its appearance and size, the hemorrhagic rash, a photo of which shows the features of the disorder, is divided into:
- petechiae;
- purples;
- ecchymoses.
Petechiae are small round spots. Their shade can vary from bright red to dark brown. When an insect bites, the middle of the petechia takes on a brighter shade when compared with the rest of the surface.
Purpura is a subcutaneous spot, the diameter of which is 2-5 mm, but sometimes it can be 1 cm. Often the spots merge with each other, forming one large one. May also be accompanied by burning and itching. The rash is localized on the arms, stomach, and legs. It has a purple tint, but in some cases changes to dark red or even brown.
Ecchymoses are the largest hemorrhagic rash. It consists of shapeless spots, the diameter of which ranges from 5 mm to several centimeters. Their shade can range from pink to blue-black. Elements of the rash can connect with each other, forming a large affected area, with necrotic elements in the center.
If the pathological process develops severely, then tissue necrosis can spread even further, causing rejection of a large area of skin. This can lead to gangrene.
Causes
The causes of hemorrhagic rash can be very different. It occurs at any age, regardless of gender. In adults, this condition is accompanied by liver damage. This may be due to:
- chemicals;
- alcoholic drinks;
- viruses;
- injuries;
- medications;
- junk food.
When the liver is damaged, the ability to clot blood is impaired. The cause of the rash may be a genetic predisposition. Hemophilia, a chronic bleeding disorder, is often identified among genetic diseases.
A hemorrhagic rash can be infectious. In this case, it is provoked by:
- meningococcus;
- scarlet fever;
- tick bites.
With an immunocomplex origin of the disorder, there are many different provoking factors. That is why a rash can occur against the background of a bacterial infection, a virus, a burn, vaccinations, hypothermia, or the use of certain medications.
The exact cause of rashes is not always determined. In this case, diagnosis and treatment should be carried out by qualified specialists.
Pigment
Pigment spots on the skin are spots that appear as a result of an increase or decrease in the amount of melanin pigment. In case of increased pigmentation, the spots are called hyperpigmented, in case of lack of pigment or its absence, depigmented or hypopigmented.
Hyperpigmented spots on the skin are divided into:
- congenital (these include birthmarks, lentigo);
- acquired (freckles, chloasma).
Depigmented spots are divided into:
- congenital (for example, albinism);
- acquired (vitiligo, leucoderma).
Secondary depigmentation can occur in patients with psoriasis, eczema, rosea or pityriasis versicolor at the site of the primary painful rash. These rashes turn pale against the background of tanned areas of the skin because in the area of inflammation, the ability of melanocytes to produce pigment is weakened. Such areas of depigmentation are called secondary leukoderma, or pseudoleukoderma.
Main symptoms
The hemorrhagic rash itself is not the only symptom. With each type of disease, the spots have their own characteristics. One of them is hemosiderosis. The rashes merge into one common hematoma and acquire a reddish tint. Such a disorder can be provoked by the destruction of red blood cells outside the vessels, during which iron-containing pigment begins to be released.
With liver problems, toxic substances accumulate, which provokes severe skin itching. When this organ is infected, a hemorrhagic rash on the skin appears in the form of small dots. This occurs as a result of the liver not producing enzymes that help blood clot.
Another important sign is joint damage. A similar symptom is observed quite often. A similar lesion occurs in the ankle and knee joints. This condition can be painful. Sometimes an inflammatory process begins.
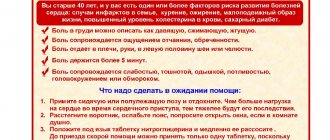
Hemorrhagic rash is a serious disease. It can also cause severe abdominal pain. Other symptoms include:
- diarrhea;
- nausea;
- temperature increase.
Some people experience internal bleeding. Depending on the cause that triggered the formation of the rash, its manifestations can vary significantly. In some cases, a hemorrhagic rash occurs on the legs, which is characteristic of other diseases, which greatly complicates diagnosis.
When a tick bites, the rashes are quite profuse and are accompanied by severe fever. With meningococcus, a stellate hemorrhagic rash with a necrotic lesion in the center is formed. In this situation, the patient must be urgently hospitalized. At the peak of the disease, fresh blood may appear in the area of the rash. After the patient’s well-being has stabilized, the skin gradually clears.
About the development of the disease
Hemorrhagic vasculitis or Schenelein-Henoch disease is a disease in which autoimmune damage to small arteries occurs - they become fragile, their permeability increases, which causes impaired microcirculation, microthrombosis, multiple small hemorrhages (hemorrhages) as in the skin (hemorrhagic rashes on the skin and mucous membranes) , and in internal organs (gastrointestinal tract, kidneys, joints).
Most often the disease develops in childhood (6-7 years), but can also affect adults. Boys get sick 1.5 times more often than girls.
Rash in a child
Among the many causes of hemorrhagic rash on children's legs, we highlight:
- hemophilia;
- vasculitis;
- purple
In some cases, the rash may cover the torso and elbows. The spots are symmetrical, do not disappear or fade during palpation. After recovery, age spots often remain. If the stage of the disease is severe, the points gradually merge with each other, forming large areas with ulcers.
Among the first signs: a sharp increase in temperature, severe headache and vomiting. In addition, there is increased weakness or anxiety, and loss of appetite. If a hemorrhagic rash forms, various types of disorders may occur on the child’s face, which is why it is important to consult a doctor in a timely manner.
The rash can also occur on internal organs; spots formed on the adrenal glands are especially dangerous. The star form is treated strictly on an inpatient or outpatient basis under the strict supervision of a doctor.
By looking at a photo of a hemorrhagic rash in children, you can determine the characteristics of the course of the disease. Especially often, such a pathology occurs in a child aged 4-12 years, if he has previously suffered from infectious diseases. With severe hemorrhagic rash in children, individual elements can merge with each other, forming ulcerative areas. After treatment, pigmentation may remain on the affected area of the skin.
Diagnostic methods
Since in children the disease manifests itself with bright, acute symptoms from the very beginning, there are, as a rule, no problems with making a diagnosis. Diagnosis of hemorrhagic vasculitis in adults is much more difficult, especially in the absence of a characteristic rash at the onset of the disease. As a rule, it is based on laboratory tests, which include:
- blood tests - general, biochemical, coagulogram;
- urine examination for hematuria, proteinuria, cylindruria, Nechiporenko and Zimnitsky tests, biochemical analysis;
- stool test for the presence of blood.
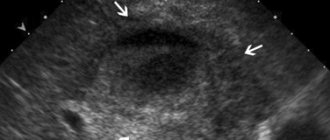
An important stage of diagnosis, which allows us to establish the degree of damage to internal organs, is instrumental studies - ultrasound of the abdominal cavity and kidneys, ultrasound of the renal vessels, gastroscopy. In severe cases of the disease, a biopsy of the skin and kidneys is prescribed to determine the size of immunoglobulin deposits and the permeability of the vascular wall.
Features of treatment
The main task of treating a hemorrhagic rash in an adult or child is to eliminate the main cause of such a disorder, that is, the primary disease. If the pathology was caused by meningococcus, then its treatment is carried out only in a hospital setting. If a child has been in contact with such a patient, he needs to be given immunoglobulin for prophylaxis to reduce the risk of developing an infection.
If measures are not taken in a timely manner, the patient may develop various kinds of complications. Internal bleeding, gangrene, kidney failure, and impaired functioning of the liver and heart can be dangerous to health and life.
If the first rash appears, you need to undergo a comprehensive diagnosis, as well as undergo the required tests that the doctor will prescribe. Treatment is aimed at eliminating the source of the rash, which is why therapy includes the use of certain drugs, which, depending on the diagnosis, are divided into groups:
- antibacterial agents - to eliminate infectious diseases;
- hormonal drugs - for the treatment of vascular and some congenital diseases;
- immunosuppressants - the action is aimed at eliminating cells that suppress the immune system.
As additional means, you can use drugs that saturate the blood with all the required microelements, eliminate pathogens, and also increase the level of blood clotting. In the presence of congenital pathologies, treatment is required throughout life, as irreversible changes may begin.
A hemorrhagic rash on the face requires the patient to remain in the hospital under the supervision of doctors until complete recovery. In some cases, not only the use of medications is required, but also a special diet.
YOU can call us: 8 (8452) 98-84-68 and +7-967-500-8468 or
Hemorrhagic vasculitis (synonyms: Henoch-Schönlein purpura, Henoch-Schönlein disease, rheumatic purpura, allergic purpura) is the most common disease from the group of systemic vasculitis. It is based on aseptic inflammation of the walls of microvessels, multiple microthrombotic formation, affecting the vessels of the skin and internal organs (most often the kidneys and intestines).
The main reason that causes this disease is the circulation of immune complexes and activated components of the complement system in the blood. In a healthy body, immune complexes are removed from the body by special cells - cells of the phagocytic system. Excessive accumulation of circulating immune complexes under conditions of predominance of antigens or insufficient formation of antibodies leads to their deposition on the endothelium of the microvasculature with secondary activation of complement system proteins along the classical pathway and secondary changes in the vascular wall.
As a result, microthrombovasculitis develops and changes occur in the hemostatic system: activation of platelets, circulation of spontaneous aggregates in the blood, pronounced hypercoagulation, decrease in plasma antithrombin III, thrombopenia, increased level of von Willebrand factor, depression of fibrinolysis.
In 1837, the famous German physician JL Schönlein described “anaphylactic purpura.” In 1874 his compatriot E.N. Henoch published a valuable work on the same disease.
The name “ hemorrhagic vasculitis ,” used only in Russia, was introduced in 1959 by the outstanding rheumatologist V. A. Nasonova. Henoch-Schönlein purpura still prevails .
Etiology
In the majority of patients (66-80%), the development of the disease is preceded by an upper respiratory tract infection.
The manifestation of the disease after typhus, paratyphoid A and B, measles, and yellow fever is described.
Other potential triggers for the disease may include:
- medications (penicillin, ampicillin, erythromycin, quinidine, enalapril, lisinopril, chlorpromazine)
- food allergy
- insect bites
- hypothermia
Sometimes hemorrhagic vasculitis complicates the development of pregnancy, periodic illness, diabetic nephropathy, liver cirrhosis, and malignant neoplasms.
Classification
By form
- cutaneous and skin-articular:
- simple
- necrotic
- with cold urticaria and swelling
- abdominal and cutaneous-abdominal
- renal and cutaneous-renal
- mixed
With the flow
- fulminant course (often develops in children under 5 years of age)
- acute course (resolved within 1 month)
- subacute (allowed up to three months)
- prolonged (allowed up to six months)
- chronic.
By degree of activity
- I degree of activity - the condition is satisfactory, body temperature is normal or subfebrile, skin rashes are not abundant, all other manifestations are absent, ESR is increased to 20 millimeters per hour.
- II degree of activity - a state of moderate severity, severe skin syndrome, body temperature rises above 38 degrees (fever), severe intoxication syndrome (headache, weakness, myalgia), severe articular syndrome, moderate abdominal and urinary syndrome. In the blood, the number of leukocytes, neutrophils, eosinophils is increased, ESR will be increased to 20-40 millimeters per hour, albumin content decreases, dysproteinemia.
- III degree of activity - the condition will be severe, symptoms of intoxication are pronounced (high fever, headache, weakness, myalgia). Skin syndrome, articular, abdominal (paroxysmal abdominal pain, vomiting, mixed with blood), severe nephritic syndrome will be expressed, and there may be damage to the central nervous system and peripheral nervous system. In the blood there is a pronounced increase in leukocytes, an increase in neutrophils, an increase in ESR above 40 millimeters per hour, there may be anemia, a decrease in platelets.
Clinical picture As a rule, hemorrhagic vasculitis is benign. Usually the disease ends in spontaneous remission or complete recovery within 2-3 weeks from the moment the first skin rash appears. In some cases, the disease becomes relapsing. Severe complications due to damage to the kidneys or intestines are possible.
There are several clinical forms of hemorrhagic vasculitis:
Simple (cutaneous) form; Articular (rheumatoid) form; Abdominal form; Kidney form; Lightning form; Combined lesion (mixed form). Clinically, the disease manifests itself with one or more symptoms:
Skin lesions are the most common symptom[7] and are one of the diagnostic criteria for the disease. A characteristic hemorrhagic rash is observed - the so-called palpable purpura, the elements of which rise slightly above the surface of the skin, which is invisible to the eye, but is easily identified by touch. Often individual elements merge and can form continuous fields of significant area. Sometimes individual elements become necrotic. At the onset of the disease, the rash may be petechial in nature.
At the onset of the disease, the rashes are always localized in the distal parts of the lower extremities. Then they gradually spread to the thighs and buttocks. Very rarely the upper limbs, abdomen and back are involved in the process.
After a few days, the purpura in most cases fades, acquires a brown color due to pigmentation and then gradually disappears. With a recurrent course, areas of pigmentation may persist. There are never scars (with the exception of isolated cases with necrotization of elements and the addition of a secondary infection).
Joint syndrome - often occurs together with skin syndrome, occurs in 59-100% of cases[5]. Joint damage develops more often in adults than in children.
The favorite localization is the large joints of the lower extremities; the elbow and wrist joints are less often involved.
Characterized by migrating pain in the joints, occurring simultaneously with the appearance of skin rashes. In about a quarter of cases (especially in children), joint pain or arthritis precedes skin lesions.
A combination of articular syndrome with myalgia (muscle pain) and swelling of the lower extremities is possible.
The duration of articular syndrome rarely exceeds one week.
Abdominal syndrome, caused by damage to the gastrointestinal tract, occurs in approximately 2/3 of all patients. It manifests itself as spastic abdominal pain, nausea, vomiting, gastrointestinal bleeding (moderate, non-dangerous bleeding occurs frequently - up to 50% of cases; severe - less often, life-threatening - in no more than 5% of cases). Severe complications such as intussusception, perforation, and peritonitis are possible. An endoscopic examination reveals hemorrhagic or erosive duodenitis, less often erosion in the stomach or intestines (any localization is possible, including the rectum).
Renal syndrome: the prevalence has not been precisely established; there is a significant range of data in the literature (from 10 to 60%). More often it develops after the appearance of other signs of the disease, sometimes one to three weeks after the onset of the disease, but in isolated cases it may be its first manifestation. The severity of renal pathology, as a rule, does not correlate with the severity of other symptoms. Clinical manifestations of kidney damage are varied. Usually isolated micro- or macroglobulinuria is detected, sometimes combined with moderate proteinuria. In most cases, these changes pass without a trace, but some patients may develop glomerulonephritis[7]. Nephrotic syndrome may develop.
Morphological changes in the kidneys range from minimal to severe nephritis with crescents. Electron microscopy reveals immune deposits in the mesangium, subendothelium, subepithelium, and glomeruli of the kidneys. They include IgA, mainly the 1st and less often the 2nd subclass, IgG, IgM, C3 and fibrin.
Lung damage: occurs in isolated cases. Patients with pulmonary hemorrhage and pulmonary hemorrhages are described. Damage to the nervous system: occurs in isolated cases. Patients with the development of encephalopathy, with minor changes in mental status, are described; there may be severe headaches, seizures, cortical hemorrhages, subdural hematomas and even cerebral infarction. The development of polyneuropathy has been described. Damage to the scrotum: occurs in children, no more than 35%, and boils down to swelling of the scrotum (which is associated with hemorrhages in its vessels). Lightning form. It is based on a hyperergic reaction, the development of acute necrotizing thrombusculitis. The disease most often develops in the first or second year of life, 1-4 weeks after a childhood infection (chickenpox, rubella, scarlet fever, etc.). Characterized by symmetrical extensive hemorrhages, necrosis, and the appearance of cyanotic areas of the skin (hands, feet, buttocks, face), which are confluent in nature. In the future, gangrene of the hands and feet, coma, and shock may develop.
Features of hemorrhagic vasculitis in children:
The severity of the exudative component; Tendency to generalize; Limited angioedema; Development of abdominal syndrome; Acute onset and course of the disease; Tendency to relapsing course.
Laboratory signs Nonspecific. An important sign to suspect the disease is an increase in the concentration of IgA in the blood serum.
RF is detected in 30% - 40% of patients. In children, an increase in ASL-O titer is observed in 30% of cases. Increases in ESR and CRP correlate with the degree of vasculitis activity.
Diagnostic criteria[edit | edit wiki text] There are classification criteria for hemorrhagic vasculitis recognized by the international community of rheumatologists, which have been successfully used in diagnosis for many years (since 1990)[8].
There are four of them, each given a clear definition.
Palpable purpura. Slightly raised hemorrhagic skin changes not associated with thrombocytopenia. Age less than 20 years. The age of onset of the disease is less than 20 years. Stomach ache. Diffuse abdominal pain, worse after eating. or intestinal ischemia (there may be intestinal bleeding). Detection of granulocytes during biopsy. Histological changes revealing granulocytes in the wall of arterioles and venules. The presence of 2 or more of any criteria in a patient allows a diagnosis to be made with a sensitivity of 87.1% and a specificity of 87.7%.
Other systems of classification and differential diagnostic criteria have also been proposed [9] [10].
Treatment First, a diet is necessary (allergenic foods are excluded). Secondly, strict bed rest. Thirdly, drug therapy (antiplatelet agents, anticoagulants, corticosteroids, immunosuppressants - azathioprine, as well as antithrombotic therapy). The following drugs are used:
disaggregants - chimes 2-4 milligrams/kilogram per day, trental intravenous drip. heparin in a dosage of 200-700 units per kilogram of body weight per day subcutaneously or intravenously 4 times a day, gradually withdrawn with a decrease in the single dose. activators of fibrinolysis - nicotinic acid. In severe cases, plasmapheresis or glucocorticosteroid therapy is prescribed. In exceptional cases, cytostatics such as Azathioprine or Cyclophosphamide are used. In general, the course of the disease is favorable, and immunosuppressive or cytostatic therapy is rarely used (for example, in the development of autoimmune nephritis).
Children must be registered at a dispensary. Conducted over 2 years. For the first 6 months, the patient visits the doctor monthly, then once every 3 months, then once every 6 months. Prevention is carried out by sanitation of foci of chronic infection. Regularly examine stool for helminth eggs. Such children are contraindicated in sports, various physical procedures and exposure to the sun.
Drug therapy
Rashes necessarily require urgent consultation with a specialist. The pinpoint hemorrhagic rash itself cannot be treated, since it is only an external manifestation of another, more dangerous disease, the consequences of which may be irreversible.
Treatment of granulomatosis involves the use of cytostatic drugs in combination with glucocorticosteroids. The main cytostatic agent is Cyclophosphamide, but in some cases Chlorbutin and Methotrexate may be prescribed. They are combined with Prednisolone. If the patient has achieved stable remission, then the medications are discontinued gradually. With proper therapy, remission can last for 15 years.
Treatment of hemosiderosis involves the use of immunosuppressive drugs, but the results of therapy may not always be positive. To achieve the best effect, they are used in combination with plasmapheresis.
Additionally, symptomatic therapy is carried out with the prescription of iron supplements to replenish its reserves in the blood. For better absorption of the drug, it is not recommended to take ascorbic acid with them. Vitamin and mineral complexes are also required.
Treatment of hemorrhagic vasculitis should be carried out only in a hospital setting. The number of drugs in this case should be limited, since any auxiliary drugs can only intensify the course of the disease.
Treatment of purpura should be comprehensive. The main group of drugs are glucocorticosteroids, which are prescribed regardless of the course of the disease. The main drug is Prednisolone. In some cases, surgical intervention is indicated.
Treatment of hemorrhagic rash caused by meningitis is carried out in a hospital setting with the prescription of antibiotics to which meningococcus is sensitive.
Treatment of purpura
To bring the skin condition back to normal, ordinary ointments or creams are not enough. Treatment of a hemorrhagic spot requires accurate diagnosis to exclude other diseases with similar symptoms.
Self-treatment of purpura with dubious means or with the help of traditional medicine does not give the expected result and can be dangerous for the body.
When you seek medical help at our medical and aesthetic center, you receive qualified assistance from experienced specialists. To diagnose pathology, we use modern laboratory tests.
Treatment of the disease includes a comprehensive selection of drugs, which may include antibiotics, hormonal therapy, antihistamines, anticoagulants, and drugs to support the immune system. The selection of medications is carried out on an individual basis, taking into account the patient’s health condition.
Our specialists will also develop a number of preventive measures to adhere to diet and daily routine in order to prevent recurrence of the disease in the future.
Other treatments
In addition to prescribing medications, therapy can be carried out using other methods:
- pulse therapy;
- Acellbia;
- plasmapheresis.
Pulse therapy involves the administration of large amounts of corticosteroids. The medicine is used in critical cases when it is necessary to urgently eliminate the inflammatory process occurring in the vascular area.
Plasmapheresis is characterized by the fact that using a special device, blood is taken, which is then cleared of aggressive immune cells and returned back to the bloodstream. During the procedure, plasma is removed along with substances that provoke inflammation and some aggressive immune cells. This is one of the most effective methods of therapy, but it is short-term, which means it cannot replace taking medications. Used only in critical cases.
Acellbia involves the administration of antitumor drugs that destroy cells produced by antibodies. As a result, the activity of the immune system decreases. Such drugs have a more gentle effect compared to corticosteroids and cytotoxic agents.
Treatment of hemorrhagic vasculitis
For vasculitis, two groups of drugs are used: in mild forms - non-steroidal drugs used for symptomatic treatment, in severe forms - a group of corticosteroids that reduce the production of factors that synthesize cells that damage blood vessels.
If hormonal drugs are ineffective, cytotoxic agents are used to destroy immune cells (usually used to treat malignant tumors).
It is important to understand that corticosteroids do not treat vasculitis, they only protect organs from the damaging effects of aggressive immune cells. This is not an excavator to eradicate evil, but just an umbrella to protect against hemorrhagic vasculitis.
It is impossible to cure vasculitis, but it is important to prevent damage to blood vessels and organs. When is treatment recommended and when is prevention recommended? Treatment is indicated for active vasculitis. If there is no inflammation (in remission), therapy is useless.
For example, if a patient had a tumor about a month ago and has kidney dysfunction (according to studies), a small pinpoint rash appears on his legs. He was diagnosed with hemorrhagic vasculitis affecting the kidneys and skin. By the time we started treatment, her condition had stabilized on its own. This temporary improvement is called remission.
There is no point in recommending treatment because there is nothing that can protect the organs. The patient is simply recommended for observation.
Treatment is prescribed for active symptoms of hemorrhagic rash. If the symptoms of vasculitis are minor and the internal organs are not affected, you can simply observe the changes. In all other cases, the disease is treated in the active stage.
With vasculitis, there are stages of exacerbation, resolution, partial and even complete remission. In the latter case, no treatment is required, observation is sufficient.
There are three types of treatment:
- inducing remission;
- maintaining remission;
- Temporary withdrawal of medications.
Induction is when a steroid or cytotoxic drug in any combination is given at a relatively high dose. The dose is adjusted to relieve all clinical and laboratory signs of vasculitis. After this, the dose of drugs is gradually reduced to the minimum necessary to maintain the patient in remission.
If drug remission continues for several months, an attempt may be made to discontinue the medications.
It should be understood that drug-free and drug-free remission is a transient state: an exacerbation can occur at any time, after which you should immediately return to the remission induction mode. In this transition, the patient's role in recognizing the symptoms of an exacerbation is important.
Contact a rheumatologist, or rather his attending physician, because vasculitis is a relatively rare disease and not every doctor can choose a suitable treatment regimen. In such a situation, you can independently increase the dose of conventional medications and consult a doctor immediately.
During consultations, doctors give appropriate recommendations, but the patient does not always adequately perceive this information.
When preparing to see a doctor, make a list of questions and get answers to them:
- What are the symptoms of an exacerbation?
- In what situations should I talk to my doctor immediately?
- When can I increase the dose of the prescribed medication myself?
Knowing the answers to these questions will help you feel comfortable and able to work despite your chronic illness. Taking corticosteroids and cytotoxic drugs has side effects. They need to be known, monitored and reported to the attending physician.
Folk remedies
Instead of medications, you can use folk remedies. Garlic oil helps to cope well with any type of rash. You can use a decoction of oak bark for baths. This procedure helps speed up the healing process and also has a beneficial effect on the body.
To treat the affected area and make the skin shiny and smooth, it is recommended to use a decoction of barley grain.
Diet
If there is a hemorrhagic rash, it is imperative to adjust the patient’s diet. The principles of the dietary diet largely depend on the individual characteristics of each specific case, but there are certain general rules. The following must be observed:
- reduce consumption of protein-rich foods;
- eliminate allergens;
- limit salt intake;
- portions should be small;
- you need to eat small and regularly;
- the temperature of the food should be normal;
- diet - balanced;
- the cooking method is used to prepare dishes;
- exclude flavorings and dyes.
The patient needs to give up bad habits and adhere to a healthy lifestyle. Taking vitamins is also important.
Possible complications
Timely treatment contributes to the favorable course of the disease, and with proper therapy there are no scars left. But if you start the process of this disease, as well as in case of improper treatment, dangerous complications can arise:
- pulmonary hemorrhage;
- formation of diathesis;
- intestinal obstruction;
- disorders of the liver, heart and kidneys;
- peritonitis.
Dangerous complications can be caused by corticosteroid drugs, which are analogues of the hormone cortisol. If its level increases, pathological processes begin to occur in the body. It is possible to develop such disorders as:
- insomnia and mood swings;
- exacerbation of ulcers and gastritis;
- increased blood pressure;
- weight gain in certain parts of the body;
- swelling and fluid retention in the body;
- osteoporosis.
The greatest danger comes from damage to the bone marrow, since it is the bone marrow that is involved in the process of formation of blood cells. To monitor this process, you need to undergo tests periodically. It is important to follow preventive measures. A healthy lifestyle, proper nutrition, giving up bad habits, and maintaining a work and rest schedule help eliminate many diseases. It is also extremely important to monitor your health and the well-being of your loved ones, especially if there are small children in the family.