Few people know what systolic and diastolic blood pressure are and how important it is for both of these indicators to remain normal. Blood pressure is measured using the Korotkoff method. Tonometers today work precisely on this principle. After measuring blood pressure, doctors receive two numbers showing the systolic as well as the diastolic index.
The norm of such indicators may vary, depending on many factors, age, gender of the person, as well as the presence of concomitant diseases. A large difference between systolic and diastolic pressure is considered normal, but a small difference between these indicators can mean health problems.
The word systolic comes from the medical term systole, which refers to a short period of heartbeat. This level is considered the upper level and characterizes the force of pressure in the arteries during cardiac contraction. At the same time, the ventricles of the heart are compressed, as a result of which blood is pushed into the arteries and vessels, which is why such pressure occurs.
This indicator directly depends on the activity of the heart muscle and its condition, as well as on the speed with which cardiac contraction occurs and the strength of this process. Doctors believe that upper blood pressure is high when the heart beats rapidly, which is why systolic pressure is also called cardiac pressure. However, this statement is erroneous, because in the process of forming this indicator, large vessels and arteries are involved, serving as a kind of buffer.
Blood is released into the circulatory system during one systole, reaches the arteries and vessels in a short period, and they are able to provide resistance, on which the upper pressure indicator depends. The stronger the resistance provided by the arteries, the higher the tonometer needle will be when measuring the systolic indicator.
The normal systolic blood pressure reading is 120 mm Hg. pillar
Such indicators can be calculated based on a person’s age, as well as some individual characteristics. Sometimes doctors record a patient’s upper pressure level in the area of 130-140 mmHg. pillar and this may also be a variant of the norm. If this figure is even higher, we are talking about hypertension.
Causes of increased systolic pressure:
- diseases of the cardiovascular department of the body;
- thickening of vascular walls;
- menopause;
- decreased hemoglobin in the blood (anemia);
- kidney pathologies;
- excessive activity of the kidneys and thyroid gland in producing hormones;
- disruption of the aortic valve;
- age-related changes in the walls of large arteries.
There should be a large gap between the systolic and diastolic arterial index; if there is a small difference between these indicators, this is a reason to immediately consult a doctor.
Diastolic pressure is called lower, this medical term comes from the word diastole, the decoding of which means cardiac relaxation following systole. The formation of the lower numbers occurs due to the contraction of peripheral arteries that carry blood to the organs and tissues of the whole body. The state of the vascular system plays a significant role in diastolic pressure. If the tone of the vessels is low, their elasticity is insufficient, then the lower values will be far from normal.
At the end of the heartbeat, the aortic valve closes, preventing blood from flowing back. During this period, the heart is filled with new blood, enriched with nutrients and oxygen for the next contraction. At this time, blood moves freely through the arteries. In addition, the lower pressure index is influenced by the total blood volume in the circulatory system and heart rate. A large gap between systolic and diastolic blood pressure indicates normal processes in the cardiovascular system.
The main phases of the cardiac cycle are systole and diastole
In addition, four valves to separate these cavities and prevent blood from being pumped forward or backward when it should exist in the heart of the atrioventricular valve in a clockwise direction, as its name indicates, which separates the right ventricle from the right atrium and which is called the tricuspid valve and the left ventricular valve (separates the left atrium and ventricle), which is called the mitral valve.
The other two valves are located between the ventricles and the blood vessels that leave the heart and are called semilunar valves. The one that separates the right ventricle from the pulmonary artery is called the pulmonary valve, and the one that separates the left ventricle from the aorta is called the aortic valve.
During each heart rhythm or cardiac cycle, there are two main phases that we have already mentioned: systole and diastole. We will now explain in detail what each phase consists of, but by way of introduction it should be clear that during systole the heart contracts and during diastole the heart relaxes and fills with blood.
When the heart is filled with blood, our natural pacemaker, called the auricular node, releases electrical impulses that are transmitted through the muscle walls of the heart and stimulate its contraction. This begins systole, the active and powerful phase of the heart rate, the walls of the ventricles contract so that the pressure inside increases and the aortic and pulmonary valves open, and then blood can pass into the aorta and into the pulmonary arteries because the atrioventricular valves are closed.
Diastolic heart failure and vascular stiffness
Academician Ivashkin V.T.: – I ask Oksana Mikhailovna to make another message. "Diastolic heart failure and vascular stiffness." Please. Professor Drapkina O.M.: – Thank you very much. Dear colleagues, today I talked about myocardial fibrosis, and, in principle, when talking about myocardial fibrosis, one way or another you are talking about diastolic heart failure. We at the clinic and at the department are dealing with this problem, accordingly, now there are also certain opportunities to share the experience that we have accumulated.
We are talking about diastolic heart failure, we are talking about arterial hypertension and we say that, after all, impaired diastole is the fate of patients with a high risk of arterial hypertension. But when the risk of arterial hypertension according to SCORE is high, we know that this is severe target organ damage and more than three risk factors or, for example, metabolic syndrome, when there are other risk factors (Sergei Rudzherovich spoke today, and we together recalled the Jupiter study ", where the marker in healthy people was an increase in high-sensitivity C-reactive protein).
So the question arises. We say all the time: “Patients come to us with myocardial infarction because we treated arterial hypertension incorrectly.” What if we treated arterial hypertension correctly? Then you get myocardial hypertrophy and, accordingly, an increase in rigidity. So what happens that chronic heart failure with preserved ejection fraction is the correct treatment for arterial hypertension and that there is no other way?
Of course this is not true. But nevertheless, with this slide I would like to draw attention to this postulate: delaying myocardial infarction in a patient with arterial hypertension is not our only task. The range of our tasks is much larger, including preventing this stage, when the patient moves from simply being hypertensive to being hypertensive with chronic heart failure, usually with preserved ejection fraction.
Therefore, once again a few words about terminology. We will talk about heart failure with preserved ejection fraction. In principle, this is the correct term, but we, the medical community, allow each other to call this heart failure diastolic heart failure - probably just for shorthand.
The epidemiology is known. There are slightly different data – European and ours. According to the EPOCHA study, more than 70% of patients with heart failure have preserved ejection fraction. Of course, this is the lot of the elderly, since we are all fighting for the fact that our population is getting older, we are all fighting for life expectancy. This will lead to the fact that there will also be more patients with diastolic heart failure, and we will need to manage them somehow for many years.
Here, in my opinion, is interesting data. The annual mortality rate of patients with diastolic heart failure is indeed somewhat lower. But when we looked at mortality after three years, it almost leveled off. But, most importantly, statistics say that among patients with chronic heart failure with an ejection fraction of more than 50%, less than 60% remain alive after three years, which means 40% die.
But here, I would say, is data that shocks me. If the prognosis improves with treatment for heart failure with preserved ejection fraction (and we see here the range since 1987, when we mainly talked about the cardiorenal theory of chronic heart failure), then please note, dear colleagues, nothing happens with the improvement in prognosis patients with preserved ejection fraction - just as 60% of them died three years later, strictly speaking, after diagnosis, everything remains so. This raises the question that we may not yet know exactly how to treat this form of chronic heart failure.
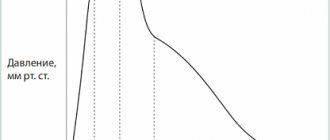
Well, very briefly I would like to remind you of the basic knowledge that we receive from the physiology course in the third year, the so-called equator (students say “equator”; having completed the third year means that you have completed half of your studies at the institute). This is the pressure-volume curve in the left ventricle, and it is the change in this curve that characterizes the main changes that occur in patients with rigid myocardium and first with diastolic dysfunction, and then with diastolic heart failure.
So, the end of diastole marks the phase of isovolumic contraction. We see that here the pressure in the left ventricle is rapidly increasing without changing its volume. The aortic valve opens and the same systole, or ejection phase, occurs. It was precisely in the shadow of this systole that there was always diastole, since we assessed the work of the heart precisely by how it contracts, by its contractile function.
Then the period of systole closes, the aortic valve naturally closes, and exactly the most interesting stage at the moment, at the time of my story today, occurs - this is diastole. The first period, it is precisely characterized by the stage of isovolumic relaxation (we see that it is very similar to the stage of isovolumic contraction), that is, a sharp decrease in pressure in the left ventricle, the mitral valve opens, and finally the filling stage occurs. You must understand that this stage is a fairly energy-intensive process, therefore, in order for diastole to be perfect, a sufficient number of macroergs is needed.
Well, the mitral valve closes, and we see (where the point that shows the mitral valve closes) that the end of diastole occurs at such a positive end-diastolic pressure. So, if the left ventricle is rigid, then this slight rise will be steeper, and the pressure that will be in the left ventricle will be higher.
The graph is two-dimensional, so it is impossible here - at least I could not - show the time, the so-called “tau”, of isovolumic relaxation. This is a very important indicator, and we will return to it below.
Thus, we can summarize those factors that influence diastole. We can summarize them by dividing them into two, in my opinion, absolutely unequal, but quite important groups. The first is, of course, the work of the ventricle, this is the early diastolic filling of the ventricle. And it is precisely factors such as: elastic return of blood to the left ventricle, contractile function of the left ventricle, stiffness of the left ventricle in diastole, properties of the pulmonary veins, area of the mitral valve opening that make an 80 percent contribution to full diastole.
But there is still a small contribution, and nevertheless, we should not forget about it either, especially when, for example, a patient comes to us with rhythm disturbances, and chronic heart failure becomes decompensated. This is the contribution of the atrium. And here the following are very important: the PQ interval, the contractile function of the atrium itself (now there are methods that evaluate this contractile function, they are not invasive - echocardiographic), heart rate (of course, the less often the heart beats, the better the diastole) and the activity of the sympathetic nervous system .
Thus, the portrait of a typical patient with arterial hypertension and diastolic heart failure is an elderly woman (usually a woman, although, of course, it can also be a man) with a long history of arterial hypertension, which is still poorly treated; with a bouquet of other pathologies, which also contributes to the possible processes of fibrosis in the heart of such patients: this is diabetes mellitus, this is coronary heart disease, this is supraventricular rhythm disturbance, kidney dysfunction, which we determine by the glomerular filtration rate, and with vascular fibrosis.
There are key differences, and we can detect them already at the stage of getting to know the patient and at the stage of his examination. Muffled heart sounds are characteristic of systolic heart failure with reduced ejection fraction. With the ejection fraction preserved, the tones can be quite decent, and even the first tone can be preserved.
Most often, we hear a gallop rhythm in both cases, and just if we are talking about systolic heart failure, then it manifests itself with the appearance of a proto-diastolic gallop rhythm - due to S3, an additional tone, a third tone. And finally, diastolic heart failure, where the greater contribution of the atria, exhausted by high end-diastolic pressure in the left ventricle, is S4.
Diastolic heart failure sometimes progresses rapidly to pulmonary edema. And here is also amazing data. Dmitry Alexandrovich, I want to discuss them with you. It turns out (I came across this article) when... Patients with pulmonary edema, completely clinically justified pulmonary edema, are admitted to the intensive care unit, and they all had their left ventricular ejection fraction measured. Then the pulmonary edema was stopped and the left ventricular ejection fraction was measured again. So, there was no pattern. It would seem that if pulmonary edema was stopped, the ejection fraction should increase, or if you were admitted with pulmonary edema, the ejection fraction should be low. There were patients with a high ejection fraction during the culmination of pulmonary edema, and vice versa.
How do you think we, as clinicians, should evaluate this, since we so often rely on this parameter - the ejection fraction?
Professor Zateyshchikov D.A.: – Well, as they say, so much the worse for the ejection fraction. In fact, many have been saying for a long time that the ejection fraction is, so to speak, not a very good parameter. And, obviously, with the advent of new non-invasive techniques - tomography, magnetic resonance imaging - we will have a more accurate method of assessment. And, perhaps, what we today accept as this very diastolic dysfunction will partially move into another category, into the systolic category. Hard to say.
But in any case, in my opinion, this once again shows that this is not the only parameter: systole is not only systole, but also something else.
Professor Drapkina O.M.: – And yet the clinic, the clinical picture is what should mainly determine our attitude towards this patient and his prognosis.
Let's get back to the slides. Thus, there are disputes, they are not over. Is this one syndrome, in which provoked diastole is, as it were, a precursor to reduced ejection fraction, or are there two syndromes? There are both supporters and opponents of various theories. To be honest, I take the position that these are still two different syndromes. Because even the portrait of these hearts, which we see during a pathological autopsy, is so different that the question immediately arises: how can such different hearts be treated with the same approaches? Well, this question is probably still eternal, there is no answer to it.
Nevertheless, we must treat such patients; we must diagnose heart failure with preserved ejection fraction. As always, algorithms come to the rescue.
The algorithm of the European Society of Cardiology also places the clinical picture of chronic heart failure at the forefront. But translating into our daily practice, this is an obese patient who came in with shortness of breath. Then normal or only slightly reduced systolic function. Let us again translate to our realities, this is a woman who came with shortness of breath, we listened to her, examined her, we see that she is obese, we see that there are fine rales in the lungs.
We send her for an echocardiographic study to clarify the diagnosis and are surprised to see that the ejection fraction is normal. This is not a reason to send this patient to a pulmonologist, this is a reason to give such a patient at least a six-minute walk test. And we will see that she may not walk the same 450 meters that would not classify her as a patient with heart failure.
Then there's really a lot of focus on biomarkers of chronic heart failure, particularly natriuretic peptide and its terminal fragment. If it is greater than 220 and we have Doppler signs, that is, we do a regular Doppler study and see when assessing flows that the E to A ratio is less than 0.5, or just the left atrium is large, or the patient has atrial fibrillation, then we can say that we have a patient with diastolic heart failure.
But, in fact, there are more difficulties than any substantiated facts, since none of the echocardiographic criteria is sufficiently accurate today. We say that tissue Doppler is very good, and this ratio E/E' is the best, but also not ideal, characterizes diastole. It is not readily available to conduct (exactly what we were talking about) MRI and various invasive hemodynamic studies. Well, in my opinion, the exact threshold values of various biological markers of heart failure have not been determined.
This raises the question: maybe we should look for possible mechanisms of diastole development in the periphery? Why? Firstly, with diastolic heart failure, certain moments of aortic stiffness also arise, but the aorta is a second heart if it is elastic. If there is an increase in the stiffness of blood vessels in general, then these reflected waves (we’ll talk about them a little later), which gather at the periphery, go to the center, to the heart. They arrive, it turns out, just at the moment of systole, they arrive a little later than they should have arrived, and collide with the newly formed pulse wave.
Again the question: does diastolic heart failure begin in the periphery? We know that blood vessels in arterial hypertension are both the culprits and the victim. Because the high pressure itself acts on the blood vessels, and at the same time the stiffness of the blood vessels, for other reasons, spasm can lead to high blood pressure.
If we talk about the main mechanisms, then, probably, the main mechanism that is responsible for the development of diastolic heart failure is precisely the increase in preload due to the stiffness of peripheral vessels. As I have already said, the speed of propagation of pulse waves increases, the preload on the left ventricle increases and the central pulse pressure increases. Right now, central pulse pressure, or pressure in the aorta, and pressure variability are given the greatest importance in the prognosis of hypertensive patients.
How does this happen? Let's imagine our vessels. Basically, these are tubes. They are elastic. And if they are elastic, as shown in the first figure, to release a blood flow - a large blood flow, since blood spreads at high speed... An elastic vessel, as it were, dampens this wave, that is, it expands a little, and then returns to normal, and we see such a schematic pulse wave, which is shown under the elastic aortic capillary tube.
If the vessel is rigid, then it cannot dampen the wave, it cannot relax a little and then contract again. And this leads to the so-called pulse wave augmentation phenomenon.
Here, dear colleagues, we can consider this phenomenon in this diagram. The gray line shows the pulse wave, which reflects the ejection of blood from the left ventricle into the aorta. The dotted line, which is shifted slightly to the right, depicts a reflected wave that comes from the periphery, from our vessels, which have damping abilities, to the center. And when these two waves are layered on top of each other, the presence of a type “C” wave occurs, or a pulse wave of type “C”, which characterizes all healthy people.
Now the arrows will show what happens in hypertensive patients, what happens with a stiff aorta. So, this graph shifts to the left, this graph shifts upward, and the formation of the so-called “A” or “B” wave occurs, which characterizes an increase in preload on the left ventricular myocardium and a decrease in diastolic blood pressure.
Thus, the analysis of this problem, in my opinion, makes it possible to provide a diagram to help the practicing physician. An increase in vascular stiffness leads to an increase in central systolic pressure in the aorta and a decrease in diastolic pressure, hence the pulse pressure increases. Increased systolic pressure in the aorta leads to increased preload on the left ventricle. Hypertrophy and the preload itself on the left ventricle and impaired relaxation lead to subendocardial ischemia. Low aortic diastolic pressure results in decreased coronary perfusion because the coronary artery fills during diastole. This diastolic pressure, which is not very low, is also important. A study of the aorta confirmed that reducing diastolic pressure below 70 for cardiovascular events is bad. Accompanying myocardial fibrosis leads to diastolic dysfunction.
We decided to conduct a pilot study in order to: evaluate the degree of damage to the endothelium and vessels of different sizes in patients with diastolic heart failure; compare different methods for assessing endothelial function - photoplethysmography and AngioScan; and see what happens during therapy based on different classes of drugs - ACE inhibitors and calcium channel blockers.
We did not forget to pay attention to biological markers. Along with the well-known N-terminal prohormone brain natriuretic peptide, we also looked at the level of galectin-3 in patients with diastolic heart failure. This is a marker, or a biological substrate that is largely responsible for fibrosis - everything: the liver, blood vessels, heart, and so on.
The study design is presented. Patients are high risk with preserved ejection fraction. We analyze endothelial function using all possible methods, randomize patients to a treatment group based on calcium channel blockers and on the basis of ACE inhibitors (amprilan was chosen as the inhibitor). We observe patients for 3-5 weeks in the hospital and then repeat the same studies.
Dear colleagues, I will not dwell on the general characteristics of the patient groups, I will only say that they were comparable in age, body mass index, and various clinical characteristics.
The first day of the study, or the start of the study, was extremely important for us, since we determined all those indicators that can be viewed during contour analysis of the pulse wave: the duration of systole, the age of the vascular wall, the augmentation index, and the stiffness index. In addition, on the same day we did an occlusion test, as if we confirmed it with each other - both by the photoplethysmographic method and according to ultrasound data.
Of course, doing this showed us that it is extremely difficult to look at endothelial function and occlusion test using ultrasound: sit in a certain position for five minutes, clamp the artery for five minutes, pump 300 mm Hg... Therefore, of course, the photoplethysmographic method won us over namely simplicity.
This is what the “C” wave approximately looked like in normal vessels.
Results. The first conclusion we made was that all patients with diastolic heart failure have pulse wave changes. Waves of type “B” and “A” are recorded, which are characterized by a high amplitude and a large range between systole and diastole.
Results of pulse wave contour analysis before the start of therapy. We see that our patients do not differ, either in the stiffness index, or in the reflection index, or in the pressure in the central vessel.
What happened during therapy? It's good to have both. That is, the lower we reduce the pressure, the better for the vessel of our hypertensive patient. Nevertheless, amprilan had a slightly greater impact on the hardness index. And amprilan also had a slightly greater effect on pressure in the aorta.
The results of the test with reactive hyperemia are an occlusion test. We also see that both groups demonstrated good results. However, a slightly greater effect of ACE inhibitors on the vascular wall was also proven in this study.
The average level of NT-proBNP hormones was 153, the average level of galectin-3 was 0.98.
The assessment of endothelial vascular function occurred in this way. We see that after an occlusion test that lasted five minutes... we would like to see an increase in diameter in the brachial artery, and below exactly what happens to the pulse waves is shown.
We found that there was an association between NT-proBNP levels and a lot of parameters, such as the 6-minute walk test, the patient's Clinical Status Rating Scale, which we use in patients with heart failure.
There was no correlation between NT-proBNP levels and left ventricular ejection fraction and parameters of diastolic dysfunction.
As for galectin-3, it turned out that once galectin-3 increased, it did not change. Which, in general, is consistent with literature data. And therefore, we propose the combined use of galectin-3 and natriuretic peptide; this can be assessed to a greater extent as a prognosis for the course of the disease.
This is a combined application. In the first column - the meaning, in the second column - the interpretation. And the risk of an unfavorable outcome, we see, is highest when there are high levels of galectin-3 and natriuretic peptides.
And finally, a clinical example. An elderly patient, over 60 years old. We see that her vessels are stiff. Both the rigidity index, the reactivity index, and the augmentation index are high. Against the background of the use of amprilan, we see a change in the pulse wave, this is visible, so to speak, visually. In addition, this, of course, can be seen from the calculated indices that exist. Please note that the reactivity index decreased from 24 to almost 8.9, and how much the central pressure decreased!
This is naturally reflected in improved endothelial function. That is, an increase... the top picture compared to the bottom picture... we see an increase in the amplitude of pulse waves by 1.3 times.
Thus, dear colleagues, the analysis of this problem makes it possible to draw such preliminary conclusions for now. It is probably true to say that diastolic heart failure begins from the periphery; in any case, vascular stiffness makes a certain contribution to changes in diastole.
The second conclusion is that biological markers of chronic heart failure are again worthy of further study, and the new marker galectin-3 for the prognosis of patients with diastolic heart failure is likely to be very promising.
And finally, our study demonstrated that lower the pressure with something, lower it to normal values, to the values that are given to us by recommendations. But still, the use of ACE inhibitors, and in particular amprilan, in our study suggested a better effect on endothelial function and a better effect on the function of vascular resistance in patients with arterial hypertension and diastolic heart failure. Thank you for your attention.
Use of medications to treat pathology
Medicines in the presence of high diastolic pressure are selected strictly individually and only after a full examination. When the disease becomes protracted or chronic, the patient is prescribed long-term therapy, which may consist of the following drugs.
Beta blockers. Their use is justified in stabilizing high blood pressure in patients suffering from angina or cardiac ischemia
It is necessary to use drugs of this group with great caution to patients who have been diagnosed with bronchial lesions, including asthma. Good examples of beta blockers are the drugs Atenolol and Anaprilin
Calcium antagonists
Refers to traditional drugs for reducing high diastolic pressure. They have been used in treatment since the last century. Calcium antagonists are indicated mainly for patients with myocardial ischemia. The group of these drugs includes Verapamil and its analogues. ACE inhibitors. They can be used not only to reduce high lower pressure, but also general pressure. Patients respond positively to the use of drugs in this group, as they rarely experience side effects. In rare cases, while taking ACE inhibitors, these include Ramipril and Enalapril, patients may experience a dry, prolonged cough. Its appearance makes further therapy impossible and requires a change in medications.
Atenolol Actavis helps reduce high diastolic pressure
Attention!!! Patients with kidney problems need to carefully select the dosage of any medications. If the recommended dose is exceeded, they may develop bradycardia and kidney failure. Traditional medicine can be used in combination with traditional
But despite the use of natural ingredients, you should first coordinate your treatment with your doctor and rule out possible allergies to the ingredients
Traditional medicine can be used in combination with traditional medicine. But despite the use of natural ingredients, you should first coordinate your treatment with your doctor and rule out possible allergies to the ingredients.
Tincture of pine cones helps reduce high lower blood pressure
Used pine cones can be cooked 1-2 more times. But in order for the solution to be sufficiently concentrated, the infusion time is increased by a week with each procedure.
Chokeberry infusion should not be consumed if you have blood problems. Chokeberry infusion should not be consumed if you have blood problems.
This remedy can only be used if you do not have blood problems. If you have a tendency to form blood clots, you should choose other methods of therapy.
- Grind 250 g of blackcurrant into puree;
- pour the mixture with 500 ml of boiling water and simmer over low heat for 5 minutes;
- strain the grounds through cheesecloth;
- add 30 g of honey to the resulting infusion;
- Having closed the vessel, put it in a dark, cool place for 5-7 days;
- drink 100 ml twice a day;
- The course of treatment is determined only by the doctor.
During treatment, the patient is required to follow a nutritious diet with plenty of dairy and fermented milk products; green vegetables are allowed. It is necessary to completely eliminate animal fats, as they increase the deposition of cholesterol on the walls of blood vessels. It is allowed to eat low-fat fish 1-2 times a week.
Due to the danger of developing a fatal symptom, it is worth keeping a high-quality blood pressure monitor at home, this is especially true for older people and those with any diagnosed heart disease. At the initial stage, high diastolic pressure can be easily corrected, which allows not to reduce the patient’s quality of life.
When performing tonometry, high lower pressure is often detected. The most common reason is the presence of hypertension. Diastolic hypertension can be isolated (with normal systolic blood pressure), or there may be an excess of systolic and diastolic pressure at the same time. In any case, consultation with a cardiologist is necessary.
High bottom pressure
The cause of high lower pressure is usually impaired elasticity of blood vessels, their spasms or narrowing of the lumen due to accumulated cholesterol. An increased rate is recorded when:
- Kidney pathologies;
- Malfunctions of the adrenal glands;
- Vascular diseases;
- Impaired blood flow;
- Metabolic disorders;
- Overfatigue (physical or mental).
The cause may also be long-term use of certain medications. The doctor’s primary task is to identify the cause of the changes, and only then prescribe treatment. By the way, lower pressure can increase under the influence of external factors, for example, frequent stress, which causes the release of adrenaline and constriction of blood vessels, bad habits that deplete the heart muscle, poor nutrition, which contributes to the accumulation of cholesterol in the blood vessels and the accumulation of excess weight.
The effect of training on blood pressure
Blood pressure levels are very different before and after exercise. The indicator varies depending on several factors:
- type of impact – static or dynamic (rhythmic),
- person's fitness level,
- age,
- duration or intensity of the load.
While running or dancing, blood pressure and pulse pressure increase, and the heart rate increases. To deliver the required amount of oxygen to working muscles, a signal is sent to the brain via chemoreceptors to increase pressure. As a result, blood flow to skeletal muscles increases.
Optimal loads train the heart and blood vessels. However, overload has a negative effect on the condition of the entire organism. After sports activities, blood flow in the muscles is restored within a few minutes. You just need to make sure that there are no sudden jumps in blood pressure.
Important! Blood pressure is measured 20 minutes before and a quarter of an hour after exercise. It should not rise above 190/90 or fall below 90/60 mm
How to maintain normal blood pressure
Maintaining normal blood pressure is one of the main keys to systematically monitoring your own health. Everyone needs to fully understand this axiom, since jumps in blood pressure and its deviation from normal parameters almost always lead to widespread destructive processes in the body, sometimes ending in failure for a person. For example, an increase in blood pressure becomes a dangerous breeding ground for deformation of cerebral blood circulation and other serious diseases. The increased load on the walls of any vessel significantly increases the likelihood that over time they can become deformed and even rupture and begin to bleed. In such cases, the heart muscle also experiences unacceptable stress. Medical statistics provide a lot of depressing examples when high blood pressure resulted in rapid death for patients.
Low blood pressure (hypotension) is considered less dangerous. However, in this case there are many negative consequences, starting with an unpleasant uncomfortable state of a person, a decrease in his performance and the ability to adequately respond to what is happening around him. If blood pressure drops sharply, this is just as dangerous a phenomenon as its sharp jump, since brain activity becomes unbalanced, consciousness stops working in a normal functional mode, and as extreme options - coma and death.
Traditional medicine, which has many useful recipes, will also help in this matter. It should also be noted that such products are suitable for any age, as they consist of natural, natural ingredients
But still, before taking them, it is important to consult with your doctor. To normalize the condition, use the following recipes:
In a saucepan, mix 0.5 cups of horseradish rhizome, which must be grated in advance, as well as 1 cup each of beet and carrot juice, completely chopped lemon, and honey. The ingredients are thoroughly mixed and infused in a warm room for about 6 hours.
It is important that the container is closed with a lid. When the medicine is ready, it is taken daily for 1 hour.
spoon three times. This remedy will help with high blood pressure. Mix 1 cup of lemon pulp, 2 cups of honey and 2 cups of viburnum berries. The mass is infused for a couple of hours in a closed container and in a warm place, after which it is poured into a glass container in which it will be stored. You need to take the product daily, 0.5 teaspoon up to 4 times. In this case, it should be washed down with cold water. The drug helps increase blood pressure. Take 1 tbsp. a spoonful of honey, dissolve it in 1 glass of mineral water, then add a little lemon juice. This drink is for one use, it is drunk before a meal. The course must be continued for 10-15 days. The healing drink fights hypertension, insomnia, and nervous conditions. Cranberries are ground together with powdered sugar. This mixture is consumed 1-2 teaspoons before meals 3 times a day. The medicine is useful for mild forms of hypertension. Take 100 gr. marsh cudweed, 4 cups honey, 0.5 l. vodka and 4 glasses of beet juice. The ingredients are mixed and poured into a bottle, where it will infuse for 10 days. The mixture is taken daily, 1 teaspoon a few minutes before meals. A natural remedy that is indispensable for hypertension.
Taking all this into account, a person must constantly monitor both his systolic pressure (upper) and diastolic pressure (lower). Systematic monitoring of these two indicators will help you be aware of your constant blood pressure. And in case of deviation from the norm, immediately take appropriate measures, including consulting a doctor. It is worth adding that it is necessary to measure your blood pressure at the same time of day, since it is usually lower in the morning and reaches its peak in the evening. A healthy lifestyle, giving up bad habits such as smoking and alcohol abuse, a proper daily routine, following an optimal diet with a minimum intake of fatty foods, salt, etc. will be an excellent help. The doctor can also suggest other effective means of maintaining normal blood pressure. This should not be difficult for one simple reason: a person does all this not for anyone, but for himself personally! Good health to you!
Reduced upper pressure
Low upper pressure may be associated with lifestyle or illness. In the first case, we are talking about constant overwork and systematic stress, lack of sleep and excessive physical activity. As for pathologies, a decrease in systolic pressure is caused by:
- Thyroid diseases, hormonal imbalances;
- Diabetes;
- Vegetovascular dystonia;
- Arrhythmia;
- Heart failure.
The cause may be prolonged depression. In any case, to normalize the pressure, you need to consult a doctor and identify the factors that contributed to the decrease in pressure. Usually the doctor recommends mainly preventive measures such as strong tea, contrast showers, and healthy sleep. But in some cases, drug treatment is required.
Measurement methods and what is their difference
Methods for measuring blood pressure differed significantly in previous eras, but the point remained the same - to measure the indicator with minimal risk to the patient’s health.
Fortunately, in the modern world, measuring blood pressure is not a problem. The reason for this is the emergence of the Korotkov method. To perform such a procedure, the doctor or even the patient needs a sphygmomanometer and a stethoscope.
It is important to take measurements regularly, at a clearly designated time. In addition, it is worth keeping a blood pressure record or diary.
It is important to measure at least three times, but avoid short periods of time between them. The interval between procedures should last approximately half an hour.
A couple of hours before the expected measurement, you should give up cigarettes and drinks with a high caffeine content, as well as vasoconstrictor drugs (for example, xylometazolyl nasal drops). The measurement should only be taken after sufficient rest.
During the measurement, the person should sit on a chair with a backrest, legs should be straight and relaxed. The atmosphere should be non-coercive. The hand used for measurements must be placed on a soft roller. It is worth keeping in mind that the limb should be at the same level with the intended projection of the heart.
The cuff of the device should be placed on two “fingers” above the cubital fossa. It is worth remembering that there should be at least one and a half centimeters between the skin and the cuff.
The limb should be freed from clothing or covered with a light cloth.
The stethoscope is placed at the projection point of the brachial vessel (elbow area).
When everything is installed correctly, the air should be pumped quickly, while the valve should be closed.
After the doctor stops hearing shock waves, you can begin to slowly deflate the air. The first “push” heard in the “ears” of the stethoscope is an indicator of systole, the second - diastole.
There are different types of blood pressure monitors: mechanical, semi-automatic and automatic. There is much debate about which type of device most accurately measures blood pressure.
Automatic digital devices allow you to measure not only blood pressure, but also detect irregularities in rhythm and pulse.
Such devices detect problems not only with the main types of blood pressure, but also with an equally important, but often overlooked - pulse pressure. A large difference between upper and lower blood pressure can become the basis for serious health problems.
How to increase lower blood pressure at home?
To raise diastolic blood pressure at home, you can use proven folk recipes, one of which is a ginger decoction with the addition of cinnamon. It is prepared as follows:
- Grate 50 g of ginger root or chop in any other way;
- pour 400 ml of boiling water and put on the stove (the heat should be low);
- cook for 5-7 minutes;
- add a pinch of cinnamon and cook for another 2-3 minutes.
You need to drink the decoction warm. The amount received should be divided into 3 doses. It is recommended to take the decoction on an empty stomach, but for people with diseases of the digestive system it is better to take it after meals. The course of treatment is 30 days.
For quick help, you can use cranberries, which need to be rubbed with sugar - for a glass of fresh berries you need to take 2 tablespoons of granulated sugar. Eat the resulting mixture 4 times a day an hour after meals. To stabilize blood pressure and improve well-being, 14 days of treatment is enough, but you can continue taking it for up to 1 month.
Juice treatment has a good healing effect. They need to be prepared immediately before use. The juice of the following fruits and vegetables is suitable for treatment:
- beet;
- pumpkin;
- apples;
- carrot;
- pomegranate.
These fruits can be mixed with each other. This treatment will not only help normalize blood pressure, but also enrich the body with vitamins.
This is especially important for those who lack essential nutrients. You need to drink juice 2-3 times a day, 200 ml.
It is better to do this on an empty stomach. The course of therapy is 21 days.
If there are no contraindications, you can use hawthorn tincture to quickly help the body. Before use, it must be diluted in boiled water. The dosage is calculated individually: on average, a single dose ranges from 5 to 15 drops. You need to take the product 3 times a day for 2 weeks.
other methods
To increase diastolic pressure, you can use massage of the cervical-collar area (especially for people suffering from cervical osteochondrosis). It should be done with stroking and rubbing movements strictly clockwise, avoiding strong pressure, pinching and other aggressive techniques.
Instead of massage, you can use breathing exercises. First, you need to take a deep breath and hold your breath for 10-15 seconds, then exhale sharply through the nasal passages. You need to repeat the steps 15-20 times.
If you have an assistant nearby, you can pour cool water over the back of the head. Here you need to not overdo it, because if the water temperature is very low, there is a risk of chilling the cervical and submandibular lymph nodes. A good alternative to dousing is contrasting limb baths. Place two deep containers with hot and cold water on the floor or table (depending on which part of the body will be lowered into the water). Hold your hands or feet in each container alternately for 1-2 minutes. You should always finish the procedure with a cold bath.
Blood pressure: norm and deviations. Blood pressure: normal for age
Blood pressure, the norm of which varies from person to person and changes with age, also depends on the state of health and even lifestyle. This is an important indicator of how healthy the body is. Let's tell you in more detail.
Photo: pixabay.com
Blood pressure: what is it?
Blood pressure is an indicator of how much pressure in the blood arteries exceeds atmospheric pressure. It is influenced by heart rate and vascular elasticity.
In a healthy body, blood pressure constantly changes. Its fluctuations are influenced by the following points:
- what emotional state the person is in;
- whether he experiences stress and nervous tension;
- does he have any bad habits?
- what kind of physical stress the body experiences;
- what kind of nutrition does the body receive;
- what is the air temperature (temperature changes - pressure changes).
Millimeters of mercury (mmHg) is a unit of measurement for blood pressure.
Photo: pixabay.com
The indicator of the force with which the heart, contracting to its maximum, pushes blood into the arteries is considered to be the upper pressure.
Not affected by:
- ventricular volume;
- maximum speed of blood entering the arteries;
- heart rate;
- stretching of the aortic walls.
The way the heart, in its most relaxed state, supplies blood to the arteries is lower pressure. It is called diastolic. This is the second digit when measuring pressure. This is confirmed by WebMD experts.
It is influenced by the following factors:
- elasticity of the walls of blood vessels;
- degree of arterial patency;
- the frequency at which the heart contracts.
- How elastic are the walls of blood vessels;
- what is the degree of patency of the arteries.
People suffer from both high blood pressure and low blood pressure.
You have high blood pressure if you have the following symptoms:
- you feel dizzy or have a headache, you feel bouts of nausea;
- increased excitability and anxiety;
- nosebleeds suddenly begin;
- vision deteriorates, spots or circles appear before the eyes;
- The face turned red and the eyelids swollen.
Experts share on the pages of WebMD about how to daily control and lead a full life with hypertension.
Photo: pixabay.com
To prevent high blood pressure, doctors recommend:
- Get regular medical check-ups.
- If possible, avoid nervous tension and stress.
- Reduce salt intake and increase the amount of vegetables and fruits in your diet.
- Give up bad habits and lead an active lifestyle.
- Watch your own weight.
Low blood pressure has the following symptoms:
- feeling of weakness, lethargy, general weakness;
- absent-mindedness and memory impairment;
- pain in the back of the head;
- feeling that there is not enough air when you are in a room with many people;
- increased fatigue, sweating and shortness of breath;
- feeling of dizziness when changing body position;
- increased sensitivity to temperature changes.
To prevent low blood pressure, doctors recommend:
- Sleep at least eight hours a day.
- Warm up before getting out of bed.
- Do not neglect the contrast shower.
- Exercise regularly, do morning exercises and lead an active lifestyle.
- Eat right and don’t neglect a hearty breakfast.
Blood pressure: norm by age, table
Doctors use the term "normal blood pressure." This is the ideal level of blood pressure and heart function for an adult between the ages of 20 and 40.
In medicine, it is generally accepted that 120/80 mm Hg. Art. the so-called absolute norm. At 130/85 mmHg. Art. - pressure is slightly increased. Normally high blood pressure is considered to be 139/89, and pathological is 140/90.
Normal human blood pressure is a rather abstract concept. It can only be obtained if a person is in a state of emotional peace and physical relaxation. Our body independently controls the level of blood pressure, changing it by an average of 20 mm Hg. Art. one way or the other.
Depending on gender and age, the concept of normal changes. For example, for people aged 16–20 years, slightly low blood pressure is 100/70 mmHg. Art. - is considered a physiological norm.
More detailed age norms are presented in the table:
Changes in blood pressure are influenced by internal and external factors. Normal values depend on gender and age
Therefore, it is important to know your age norm and control it
The article is for informational purposes only. Do not self-medicate. For professional help, consult your doctor.
Increased systolic pressure
High upper pressure is a sign of:
- Overactive thyroid gland (thyrotoxicosis);
- Severe anemia;
- Bradycardia (decreased heart rate);
- Aortic valve insufficiency;
- Reduced elasticity and increased density of the vascular wall (for example, atherosclerosis of the aorta).
This condition is called isolated systolic hypertension or systolic hypertension. Upper blood pressure often increases during adolescence. This is due to hormonal changes in the body and is not considered a deviation. With the completion of puberty, the indicators return to normal. True, such changes increase the chances of developing hypertension in adulthood.
Treatment of systolic hypertension is generally similar to those taken for normal hypertension. This also applies to prevention. The main thing is to identify the disease in time, regularly monitor your blood pressure and take medications prescribed by your doctor, including those that help lower blood pressure. In addition, you need a diet, adequate physical activity, and protection from stress.
Heart sounds
The heart makes characteristic sounds similar to a knock. Each beat consists of two main tones. The first is the result of contraction of the ventricles, or, more precisely, the slamming of valves, which, when the myocardium is tense, close the atrioventricular openings so that blood cannot return to the atria. A characteristic sound is produced when their free edges close. In addition to the valves, the myocardium, the walls of the pulmonary trunk and aorta, and tendon threads take part in creating the shock.
The second sound is formed during ventricular diastole. This is the result of the semilunar valves, which prevent blood from flowing back, blocking its path. A knock is heard when they connect in the lumen of the vessels with their edges.
In addition to the main tones, there are two more - the third and fourth. The first two can be heard using a phonendoscope, while the other two can only be recorded by a special device.
The activity of the heart is characterized by cyclic sounds produced, they resemble tapping. The components of each blow are two easily distinguishable tones.
One of them arises from contractions in the ventricles, the impulse of which arises from the slamming of the valves that close the atrioventricular openings during myocardial tension, preventing the penetration of blood flow back into the atria.
The sound at this time appears directly when the free edges are closed. The same blow is produced with the participation of the myocardium, the walls of the pulmonary trunk and aorta, and tendon threads.
The next tone occurs during diastole from the movement of the ventricles, being at the same time a consequence of the activity of the semilunar valves, which prevent the blood flow from penetrating back, acting as a barrier. The knocking becomes heard at the moment of connection in the lumen of the edges of the vessels.
We suggest you read how long you can wear compression stockings per day
In addition to the two most noticeable tones in the heart cycle, there are two more, called the third and fourth. If a phonendoscope is enough to hear the first two, then the rest can only be recorded with a special device.
What do pressure indicators and their norms depend on?
The value of blood pressure is influenced by the factors described in the table.
To move blood through the vessels, it is necessary to create a pressure difference, since the blood flow is from high to low levels. This is possible due to the contraction (systole) of the ventricles. During the period of diastole (relaxation), they are filled with blood; the more it enters, the stronger the muscle fibers work, pushing the contents into large vessels.
In diseases of the myocardium, endocrine and nervous pathologies, the synchrony and duration of parts of the cardiac cycle are disrupted.
Read in this article
Conduction system of the heart
The processes of excitation in the heart, impulse conduction and contraction of the heart muscle are unique. For example, in the presence of adequate nutrients and oxygen, an isolated heart can contract for a long period of time without an external nerve impulse. The heart has an autonomous system for generating nerve impulses, the sinoatrial node, which is located in the right atrium at the level of the confluence of the superior vena cava. This so-called pacemaker (pacemaker) generates approximately 60-70 impulses per minute. The impulse causes contraction of the atrium muscles, through which it is transmitted to the atrioventricular node (AV node). From there, the impulse reaches the His bundle, which is a fibrous muscle structure, and is transmitted further to the ventricular myocardium. There, it first passes through the branching node (Tovar's node) along the interventricular septum to the apex of the heart and is distributed along the Purkinje fibers throughout the entire ventricular myocardium. Thus, the heart muscle is excited and, in accordance with the impulse conduction system, contracts rhythmically.
The frequency, speed of impulse conduction and degree of contraction depend on the autonomic nervous system. This brings the activity of the heart into line with the body’s demands (for example, an increase in minute volume of blood flow during physical activity).
Blood pressure parameters
A significant proportion of people with cardiovascular problems suffer from an imbalance in blood pressure.
In medical practice, there is a diastolic option - the lowest, and systolic - the highest point of pressure.
Blood pressure is a constant indicator. Of course, the figure can vary within a certain range. The range of blood pressure indicators is the norm, that is, those indicators at which the organs do not suffer and the person feels well.
The blood pressure indicator means a certain volume of blood distilled over a certain period of time by the heart muscle, as well as the resistance of the walls
and vessel.
The highest pressure levels are in the arteries, the lowest in the venous vessels.
The upper value of blood pressure is the tension in the vessel during myocardial contraction (systole). The lower value is the pressure during the period of relaxation of the cardiac fibers, this indicator is minimal.
The most “popular” and at the same time the healthiest blood pressure is one hundred and ten over seventy. Although the conjunction “on” is used in this case completely incorrectly, it is correct to say “and”, since these two types of pressure do not intersect with each other.
Systole and diastole
The ventricles pump blood into the pulmonary trunk and aorta synchronously and in small volumes. Myocardial contraction in this constantly repeating two-phase cardiac cycle is called systole, relaxation is called diastole. Each of these periods, in turn, is divided into two phases:
systole: - contraction phase; - expulsion phase. diastole: - relaxation phase; — filling phase.
During the first phase of systole, the ventricular myocardium begins to contract (contraction phase). Since the atrioventricular valves are closed and the semilunar valves have not yet opened, the pressure in the ventricles increases rapidly, which is not accompanied by a change in the volume of blood contained in them (isovolumetric or isovolumic contraction). However, as soon as the pressure in the ventricles reaches the pressure in the aorta (about 120 mmHg) or in the pulmonary artery (about 20 mmHg), the semilunar valves open and the ejection phase begins. During this phase, maximum contraction of the ventricles occurs, and about 70 ml of blood (stroke volume) exits into the artery (at rest). Ventricular pressure drops below arterial pressure again and the semilunar valves close.
Systole is followed by diastole, during which the myocardium relaxes and initially the atrioventricular valves remain closed. In this case, the intraventricular blood volume does not change (final diastolic volume, about 70 ml). Then the pressure in the ventricles becomes lower than in the atria, the atrioventricular valves open, and blood begins to flow from the atria into the ventricles (ventricular filling). The signal for this is, first of all, the beginning of contraction of the atria, and especially the descent of the base of the heart. Due to this, in the expulsion phase, the base approaches the apex, expanding the atrium and sucking blood from the veins. As the ventricular myocardium relaxes, the base of the heart moves upward again, and blood enters the ventricles through the opened atrioventricular valves.
Reasons for violation of indicators
Violation of myocardial contractility and weakening of systole cause ischemic and dystrophic processes - angina pectoris, cardiosclerosis, amyloidosis, myocardial dystrophy, myocarditis. Due to narrowing of the valve openings or difficulty in ejecting blood from the ventricles, the amount of residual blood in their cavities increases, and a reduced volume enters the vascular network.
Such changes are characteristic of congenital and acquired heart defects, hypertrophic cardiomyopathy, and narrowing of the great vessels.
Violation of the formation of an impulse or its movement through the conduction system changes the sequence of myocardial excitation, the synchrony of systole and diastole of parts of the heart, and reduces cardiac output. Arrhythmias change the duration of the phases of the cardiac cycle, the efficiency of ventricular contractions and the possibility of their complete relaxation.
Diseases that are accompanied by diastolic and then systolic dysfunction also include:
- pericarditis;
- bacterial endocarditis;
- arterial and pulmonary hypertension;
- hypotension;
- systemic autoimmune pathologies;
- disorders of endocrine regulation - diseases of the thyroid gland, pituitary gland, adrenal glands;
- vegetative-vascular dystonia is an imbalance between parts of the autonomic nervous system.