Prevention of early “preclinical” stages of atherosclerosis
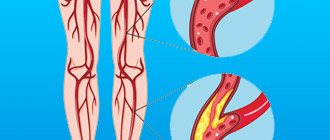
Atherosclerosis is a chronic disease characterized by specific damage to elastic and muscular-elastic arteries. In their walls, connective tissue grows in combination with lipid (fatty) infiltration of the inner membrane. This leads to organ and general circulatory disorders.
Atherosclerosis is a major disease of the cardiovascular system, causing angina pectoris (angina pectoris), myocardial infarction, stroke and death. According to WHO, in recent years, mortality from coronary heart disease, the main cause of which is atherosclerosis, has increased significantly. Atherosclerosis is called a disease of civilization. Indeed, an inactive lifestyle, unhealthy diet, addiction to bad habits, obesity, poor heredity, age - all these factors lead to the fact that a person begins to show signs of atherosclerosis.
It is a mistake to think that this disease is reserved for older people. Alas, atherosclerosis is increasingly affecting young people and even children. It is difficult to treat severe atherosclerosis. But, unfortunately, its symptoms often appear only when atherosclerotic plaques have already affected the coronary vessels of the heart and brain, arteries of the kidneys, pancreas and sensory organs.
The most at risk for atherosclerosis are men, who get sick more often than women, and in the latter, atherosclerosis develops on average 10 years later than in men. These differences are a consequence of different lifestyles, diet, occupation, genetic characteristics, neuro-hormonal factors, etc.
Preventive measures for atherosclerosis from 20 to 25 years of age become especially relevant for any person. The approach must be systematic. It should be borne in mind that in the early stages this disease is asymptomatic. Due to the high frequency of asymptomatic variants of the course of atherosclerosis, in all patients with risk factors for the development of this disease, it is necessary to assume the presence of atherosclerosis and carry out its prevention and diagnosis.
There are primary and secondary prevention of atherosclerosis. Primary prevention is aimed at preventing the development of the disease and is carried out among people who are practically healthy and have no signs of disease, and secondary prevention concerns people with existing diseases that contribute to increased formation of plaques.
These cases depend entirely on the patients themselves, their compliance with the doctor’s recommendations and are under the control of medical institutions.
Primary prevention includes measures aimed at organizing the correct work and rest regime, balanced nutrition, elimination of the main risk factors (excess body weight, smoking), identification and treatment of diseases that contribute to the development of atherosclerosis (hypertension, diabetes mellitus). Secondary prevention of individuals at risk for atherosclerosis or already suffering from it is important.
Detection of lipid levels in the blood and their detailed analysis are the basis for laboratory diagnosis of the early “preclinical” stages of atherosclerotic lesions. Laboratory studies of the main indicators of lipid metabolism (especially in combination with indicators of carbohydrate metabolism and liver function) make it possible to determine the degree of risk of developing atherosclerosis, coronary heart disease and to outline ways of prevention and therapy. Screening for hyperlipoproteinemia is necessary.
In every patient over 20 years of age, it is necessary to determine the concentration of total cholesterol. If the concentration of total cholesterol is more than 5 mmol/l, the lipid profile (total cholesterol, triglycerides, high-density lipoprotein cholesterol (HDL), low-density lipoprotein (LDL), very low-density lipoprotein (VLDL) cholesterol should be determined, as well as the calculation of the atherogenic coefficient.
In the clinical diagnostic laboratory of the Consultative and Diagnostic Center, lipid profile determination is carried out every day except Sunday. The result is issued within one working day.
It is recommended to donate blood in the morning (between 8 and 11 o’clock), strictly on an empty stomach (at least 8 and no more than 14 hours of fasting, you can drink water). Food overload should be avoided the day before.
Interpretation of the analysis result with subsequent recommendations is carried out by the attending physician of the Consultative and Diagnostic Center.
ATHEROSCLEROSIS. TIME TO CHANGE YOUR LIFE
25.Oct.2019
Damage to the cardiovascular system by atherosclerosis is one of the main causes of acute myocardial infarction, stroke, peripheral circulatory disorders and, as a consequence, disability and mortality.
However, it should be remembered that atherosclerosis is not only a disease of blood vessels, it is a systemic disease that affects the entire body. The disease proceeds as follows: on the inner surface of the arteries (which is normally very smooth and even), peculiar growths appear - plaques, protruding into the cavity of the blood vessel (like rust in pipes). Over time, these formations increase, and when the lumen of the vessel narrows to 70%-80%, difficulty in blood flow occurs, which means attacks of angina pectoris, myocardial infarction, strokes, etc. may occur.
The development of atherosclerosis (especially characteristic of old age) is greatly influenced by living conditions, work, nervous overload, the presence of hypertension, as well as alcohol consumption, smoking and a number of other conditions. Practice shows that men are more predisposed to this disease (92% of all cases); often, in the stronger sex, the appearance of the disease directly depends on the characteristics of work and life.
DIET VS...
Often with atherosclerosis, there is an increased level of cholesterol in the blood, so it is impossible not to take into account an irrational diet of animal foods rich in fats. To reduce the “cholesterol” indicator, it is recommended to consume foods: grains: wholemeal bread, porridge cooked in water (buckwheat, barley and especially shaggy), pasta (group A); dairy: skim milk, cottage cheese, cheeses (20% fat) - Suluguni, Adyghe, Brynza, Ossetian; soups: vegetable, meat and poultry broths are undesirable; fish: all types, including oily sea fish (it is better to remove the skin), but it is advisable to consume it at least 2 times a week or one fish dish daily; meat: lean beef, veal, “young” lamb 85-90g. (in finished form); Poultry: Turkey, chicken (white meat), fat and skin should be removed from poultry before cooking; fruits (apple, pear, orange, peach), berries (raspberries, strawberries, blueberries), vegetables (cauliflower, broccoli, green beans) and legumes (peas, beans, lentils. Don't forget: boiling, stewing, casseroles and grilling are done only with vegetable oil or without oil in dishes with a special coating that does not require the addition of fat.
SPORTS FROM THE “BAD”
Along with the above diet, physical activity should also be increased. Dynamic aerobic exercises are recommended, such as cycling, measured walking, swimming, team sports (football, volleyball, etc.). Such physical exercise of moderate intensity for 30-40 minutes at least 3 times a week not only improves the condition of the cardiovascular system, reduces the level of “bad” cholesterol, but also increases the production of “good” cholesterol in the body, including in patients who have undergone myocardial infarction.
It is also important to remember that static loads (lifting weights, carrying loads, etc.), which provoke an increase in “bad” cholesterol in the blood, a rise in blood pressure, etc. And further!
Monitor your blood pressure and cholesterol levels daily, monitor your body weight, stop smoking, learn to deal with “bad” emotions, avoid overexertion and conflict situations, spend more time on auto-training and relaxation methods.
O. Solomennikova, general practitioner, Nyagan City Clinic
Prevention of atherosclerosis
A healthy lifestyle is the main way to prevent atherosclerosis. Only a nutritious and balanced diet, sufficient physical activity, and giving up bad habits will have a positive effect on the condition of blood vessels. In addition, a mandatory method of prevention (or at least identifying the disease at an early stage) is to pay attention to your health: preventive examinations by doctors and taking a cholesterol test. If you have hypertension, you must constantly monitor your blood pressure and take the necessary medications; if you have diabetes, maintain normal blood sugar levels.
Watch your health and remember that a healthy lifestyle is necessary for everyone!
Newspaper “News of Medicine and Pharmacy” 17(224) 2007
What is primary prevention of atherosclerosis?
Primary prevention is the timely identification of risk factors for atherosclerosis and ischemic heart disease, their correction or elimination in individuals without any clinical manifestations of the disease. It is aimed at preventing or slowing down the atherosclerotic process.
What is secondary prevention of atherosclerosis?
Secondary prevention is the correction or elimination of risk factors in individuals with clinical manifestations of atherosclerosis, forms of ischemic heart disease and their complications, accelerated recovery, improved quality of life, increased life expectancy within the biological age, reduced severity of the disease and improved prognosis for life and work ability, both by lifestyle changes (quitting smoking, increasing physical activity, following an appropriate diet), and by prescribing (if appropriate indications) adequate lipid-lowering, antihypertensive, antidiabetic, antiaggregation, antioxidant and antithrombotic therapy.
What are the possible positive results of correction of lipid metabolism and anti-atherosclerotic therapy in the primary and secondary prevention of coronary artery disease and its complications?
It is now firmly established that it is possible to significantly influence the reduction of morbidity and mortality caused by atherosclerosis only through prevention. This has been proven in randomized studies with appropriate assessments:
— reduction in mortality from coronary heart disease by 15%;
— reduction in overall mortality by 11%;
— reduction in total cholesterol levels by 18%;
- reduction in LDL cholesterol - the first target for preventing coronary artery disease by 13%.
The severity of preventive measures depends on the correction or elimination of key risk factors such as smoking, arterial hypertension and elevated levels of cholesterol in the blood serum.
What causes an increase in LDL cholesterol levels?
Excessive consumption of saturated fat and excessive caloric intake of food provokes an increase in LDL cholesterol levels.
What is the role of physical inactivity in the development of atherosclerosis?
Physical inactivity contributes to a decrease in the level of HDL cholesterol and an increase in body weight due to the fat layer in the abdominal area with simultaneous emaciation of the lower and upper extremities, as well as the face, which is associated with hyperlipidemia, especially hypertriglyceridemia, both directly and through impaired glucose tolerance, up to before the development of type II diabetes mellitus.
What is the role of obesity in the development of atherosclerosis?
Android obesity (excessive deposition of abdominal fat with thin thighs and buttocks) is associated with increased resistance to endogenous insulin, the occurrence of hyperinsulinemia and a high content of small, dense LDL.
How does smoking contribute to the development of atherosclerosis?
Cigarette smoke contains 300 chemical compounds (of which 60 are so-called beneficial). The most harmful to health are those that contain salts of heavy metals - strontium, cobalt, cadmium, lead, etc. Smoking also helps reduce LDL cholesterol by about 20%.
The role of alcohol in the development of atherosclerosis
Alcohol abuse is one of the causes of elevated triglyceride levels, and in some cases it provokes type I or IV hyperlipidemia with hyperchylomicronemia and severe hypertriglyceridemia, which causes acute pancreatitis.
It is widely believed that the anti-sclerotic effect of alcohol is associated with an increase in HDL cholesterol levels. This statement is true only when alcohol is consumed in minimal quantities by practically healthy individuals (up to 40 years of age). This should be a high-quality drink, environmentally friendly bottling, preferably from a harvest of high-quality red grapes growing in certain areas of the Caucasus, France, etc., with a low strength, or high-quality dry wine (unfortified wines). After 40 years, the majority of males and females living in unfavorable environmental and unstable natural and meteorological conditions already have several previous diseases.
Natural resistance to atherosclerosis has been described, occurring in young people who use alcohol or drugs, in particular, in those whose parents abused alcohol or were addicted to drugs.
Apo A is the main protein of HDL - a marker of antiatherogenic function, which has the property of oxidizing cholesterol in the liver. Therefore, whatever the total pool of total cholesterol, but in conditions of a healthy liver, pancreas and intestines, as well as in the presence of a sufficient concentration of HDL, the formation of oxidized cholesterol occurs, since HDL are the main suppliers of substrates for oxidized (“self-burning”) cholesterol (or cholesterol as an energy and plastic cellular, in particular membrane, product).
What is the main goal of nutritional therapy?
The goal of dietary therapy is to avoid provoking atherosclerotic attacks or attacks, reduce the consumption of saturated fats, cholesterol (egg yolk, fatty pork, etc.) and reduce daily dietary calories with a relative increase in the content of polyunsaturated fatty acids in the diet. The amount of proteins should not change, and caloric intake should be maintained through the consumption of complex carbohydrates and proteins of plant origin, and not refined sugars (sweets, cakes, etc.). In this case, it is necessary not only to reduce the overall dietary calorie intake, but also to avoid physical inactivity, for example, after a hearty, hearty lunch, you should not immediately go to bed, but on the contrary, you should move around. You should regularly increase your physical activity in any convenient and pleasant way for a person.
What is the 1st degree diet?
This diet does not involve a radical revision of nutrition. This requires limiting the consumption of egg yolk, lard, butter, processed cheese, sour cream, cream, and fatty meats. When cooking, use exclusively vegetable oil. Meat consumption is limited, but consumption of lean beef and veal is allowed. Any type of fish is recommended. The amount of milk and dairy products is limited, but low-fat cheese and cottage cheese are recommended. The main dietary product of plant origin is potatoes, rice, buckwheat, fruits, vegetables, and cereals.
What is the 2nd degree diet?
This type of diet provides for strict restrictions on the consumption of saturated fats and cholesterol, smoked sausages, and balyk. Only a vegetarian diet and fruit fasting days are allowed.
At what level of total cholesterol and LDL cholesterol is the need for lipid-lowering therapy determined?
Certain indicators of total cholesterol and LDL cholesterol correspond to three levels of endogenous cholesterol, verified as low, borderline and high (Table 1).
What are the criteria that determine the need for lipid-lowering therapy in patients without and with coronary artery disease, taking into account risk factors?
The advisability of drug therapy in patients without and with coronary artery disease is determined by the number of risk factors with the determination of LDL cholesterol, based on both the initial level of this indicator (before treatment) and the target level of LDL cholesterol, i.e. that which should be achieved after a course of therapy. In table Table 2 presents groups of patients with coronary artery disease with a different number of risk factors and the corresponding level of LDL cholesterol before and after achieving the optimal target level.
What is traditional and radical therapy for hyperlipidemia?
Traditional therapy for hyperlipidemia includes non-drug and medicinal methods of influence. Radical therapy includes the correction of refractory and genetically determined hyperlipidemia, carried out by extracorporeal blood purification of LDL cholesterol, as well as surgical treatment and gene therapy of atherosclerosis.
What two groups of statins are distinguished depending on their effects on cholesterol and triglycerides?
Currently, a distinction is made between naturally and artificially synthesized statins. The former include lovastatin, simvastatin and pravastatin; the second - fluvastatin, atorvastatin and cerivastatin.
Their effect on cholesterol and triglycerides is presented in table. 3.
What are the anti-sclerotic, anti-inflammatory and anti-ischemic activities of statins or their pleiotropic properties?
The pleiotropic properties of statins are manifested in the inactivation of macrophages, those cells whose predecessors are circulating monocytes. Macrophages capture oxidized LDL with their subsequent destruction, as a result of which cholesterol esters accumulate in macrophages. Then macrophages degenerate into so-called foam cells, the accumulation of which under the endothelium gives rise to lipid stripes - the first morphological stage in the development of an atherosclerotic plaque. Some foam cells are constantly subject to programmed voluntary destruction (apoptosis) with the release of cholesterol crystals into the extracellular space. Statins reduce the production of metalloproteinases and proinflammatory cytokines, which destroy the cap and destabilize the atherosclerotic plaque. Due to this, statins reduce the risk of plaque rupture and intravascular thrombus formation. Statins reduce the proliferation of smooth muscle cells in the walls of blood vessels and thereby prevent the formation of a connective tissue capsule of a future plaque. Statins have systemic effects: improve and restore endothelium-dependent dilatation; have a positive effect on the rheological and coagulation properties of blood, significantly slow down the progression of atherosclerosis and even cause its reverse development in the coronary arteries.
What are the anticoagulant properties of statins?
The anticoagulant properties of statins are associated with a decrease in plasma fibrinogen levels, inhibition of ADP-dependent platelet adhesion, and inhibition of thromboxane production. Statins reduce the concentration of the first tissue plasminogen activator inhibitor and thereby reduce the likelihood of coronary spasm.
What is the fundamentally new development of standards for the management of patients with acute coronary syndrome?
Prescribing statins in the early stages of ACS reduces the progression of angina and the incidence of death.
What is the treatment strategy for simvastatin?
For primary prevention, the dose of simvastatin is 10 mg, for secondary prevention - 20 mg per day (evening dose), followed by an increase to 40 mg. The maximum daily dose is 80–160 mg.
Should patients be informed about the side effects of statins?
It is worth it, but without causing fear in him when taking drugs and indicating that discontinuation of the drug leads to the complete and complete disappearance of adverse reactions of statins.
What is the mechanism of action of fibrates, doses and conditions of their administration depending on the types of hyperlipidemia?
Fibrate drugs (gemfibrozil and bezafibrate) are the drugs of choice in patients with type IV hyperlipidemia with high levels of triglycerides in the blood. They are also indicated for rare hyperlipidemias of types I and V. Gemfibrazil is prescribed at a dose of 1200 mg 2 times per dose, 30 minutes before meals; fenofibrate - at a dose of 200 mg; ciprofibrate - 100 mg 1 time per day during the evening meal. The mechanism of action of fibrates in relation to cholesterol and triglycerides, types of apoproteins and hyperlipidemia is presented in Table. 4.
What is the mechanism of action of bile acid sequestrants (BAS), their dose and effect on blood lipids and types of hyperlipidemia?
Traditional therapy for hyperlipidemia includes the use of FFAs - cholestyramine and colestipol, which are anion-exchange resins (polymers) that are insoluble in water and not absorbed in the intestine. They bind cholesterol and FFA, which are synthesized from cholesterol in the liver.
The initial dose of cholestyramine is 4 g, colestipol is 5 g per day.
What is the mechanism of action of nicotinic acid, its dose and effect on blood lipids and types of hyperlipidemia?
The most pronounced effect of nicotinic acid is on reducing triglycerides, in particular in patients with diabetes, and increasing HDL cholesterol by 15–30%.
Dose 1.5–3 g per day; maximum dose 6 g per day.
It should be noted that nicotinic acid potentiates the hypotensive effect of antihypertensive drugs, which can cause hypotension in patients with hypertension, up to the development of syncope, especially in the elderly.
What are the new approaches in the treatment of atherosclerosis and the use of drugs with anti-sclerotic and anti-ischemic properties?
Such drugs are angiotensin-converting enzyme inhibitors - ramipril and perindopril, which have shown an anti-sclerotic effect in patients with coronary artery disease, which allows expanding their indications in the treatment of atherosclerosis.
As for the use of drugs such as probucol, essential phospholipids, tocopherol, fish oil and heparin, their effects on atherosclerosis have not been proven and require study in large multicenter randomized and placebo-controlled studies.
Is it correct to say that if the moment to begin treatment of atherosclerosis is missed, then treatment of generalized atherosclerosis will not have a positive effect?
This judgment is incorrect at the current level of knowledge and practical medical experience.
In countries where this disease has been treated over the past two decades, significant success has been achieved both in reducing mortality from CVD and in reducing overall mortality.
In primary and secondary prevention, it is necessary to achieve a reduction in cholesterol by 25% in patients with atherosclerosis of the brain and lower extremities, as well as those who have suffered a myocardial infarction.
The goal of lipid-correcting and anti-atherosclerotic therapy is to prevent outbreaks of the atheromatous process, stabilize the disease and, finally, achieve regression of atherosclerosis with long-term treatment.
Does simvastatin improve the prognosis and affect the survival of patients?
Simvastatin reduces overall mortality and from coronary artery disease, as shown by the Scandinavian SSSS study. It has been shown that secondary prevention of coronary heart disease not only helps to reduce lipids, but also improves life prognosis, and also affects people's life expectancy. At the same time, overall mortality is reduced by 30%, and the risk of death from coronary heart disease by 42%.
Is it possible to monitor individual prognosis of risk factors?
The risk of disease and mortality from coronary artery disease depends on 200 risk factors for atherosclerosis. In order to take into account such a number of individual risk factors for the disease, computer programs, tables, and diagrams are currently being compiled that make it possible to assess the risks of each individual person and, based on this, decide whether it is necessary to reduce the level of lipids in the blood or not. To avoid lifelong use of statins, fibrates and other drugs, it is important to get rid of at least half of the risk factors that each individual person has, such as physical inactivity, excess nutrition, abuse of refined carbohydrates or fatty meats, etc.
It is important to take into account the general risk factors for complications associated with coronary artery disease. For example, if a patient with AMI develops gastrointestinal bleeding, does he need a blood transfusion in order to stop this bleeding? But if the patient dies not from bleeding, but from pulmonary edema, then one should think about whether the doctors overestimated the threat to the patient’s life from possible blood loss, without thinking that the bleeding in such a patient could be compensatory in nature in response to the increased volume of circulating blood. blood. And infusion of 200 ml of freshly citrated blood into a patient with severe AMI provoked pulmonary edema. The patient, according to this logic, cannot be ruled out, died due to the fault of diligent doctors who made the wrong decision, did not weigh the pros and cons and did not make a choice between two evils in the direction of the lesser evil.
Based on this, is it worth hitting the sparrows with guns, using statins, without worrying about deciding on the dietary regimen, smoking, and physical inactivity of a patient with incipient atherosclerosis. In the latter case, it is possible to prevent the progression of the disease in simple but systematic ways (directing one’s efforts to combat Pushkin’s principles “The habit is given to us from above” or “Sins leave us when we can no longer indulge in them”), rather than resorting to those which unilaterally reduce blood lipids, without taking into account more severe lifestyle violations and getting rid of bad habits.
The higher the overall risk of complicating factors on the course of the disease, the more difficult it is to correct atherosclerosis in patients with acute coronary syndrome. Previously, it was believed that in case of AMI, statins were indicated only after discharge from the hospital. It has now been proven that in case of AMI they are indicated in the first hours and days of ACS, which can significantly improve the patient’s condition and the prognosis of the disease due to the pleiotropic properties of statins, without taking into account low blood lipids as an important criterion in assessing the type of hyperlipidemia in atherosclerosis.
Do lipid-lowering drugs in the primary prevention of atherosclerosis affect overall mortality?
Lipid-lowering drugs do not affect overall mortality, but when cholesterol fluctuates more than 8.2 mmol/l, the use of lipids is justified in the absence of other risk factors. If cholesterol fluctuations are from 8 to 7 mmol/l and there are no other other risk factors, then prevention tactics should depend on the total risk of episodes of coronary heart disease over the next 10 years. If cholesterol is below 7 mmol/l, then a healthy person does not need to take medications in the absence of other risk factors. In these cases, you need to make drastic lifestyle changes in terms of diet and vigorous physical activity. After a year, in people following, for example, a vegetarian diet and dramatic lifestyle changes, LDL cholesterol decreases by 37%, and repeat angiography improves by 82%, which leads to regression of coronary stenosis. No modern medical intervention will give such an effect and, obviously, cannot.
Overall mortality is reduced by 60% with dietary interventions. The diet should be based on:
- consumption of vegetable oil with a high content of alpha-linolenic acid;
- more bread, root vegetables, green vegetables (not a single day without fruit);
— it is important to have fasting days when eating (apple, kefir, beet, etc.);
- a lipid-lowering diet should continue for at least 6 months. And if during this period it does not help, lipid-lowering therapy is needed.
How is the choice of lipid-lowering therapy adequate for a particular patient made?
The first place in initial therapy should be given to FFAs - cholestyramine or colestipol; in second place are statins; third - nicotinic acid. In cases where cholesterol levels increase in combination with an increase in triglyceride levels, nicotinic acid comes first, statins come second, and then FFAs or combinations of drugs.
Do statins work the same?
Almost the same, but preference should be given to the less expensive one.
Is there a unique niche for fibrates?
These are lipid-lowering drugs, which at the same time increase the level of HDL cholesterol, but do not act reliably and stably on LDL cholesterol. These drugs are indicated for the corresponding types of hyperlipidemia (Table 4).
How long should treatment with lipid-lowering drugs be carried out?
A decrease in the severity of coronary artery stenosis in those treated with simvastatin was detected after 4 years. Reliable results of the effect of statins on overall mortality are observed after 5 years.
Is the cost of treatment with lovastatin and simvastatin comparable?
A monthly course of treatment with lovastatin costs 25.5 USD. Simvastatin costs the same for the same duration of treatment.
Are statins indicated for normal lipid levels?
Indicated in the presence of other risk factors for atherosclerosis and the presence of concomitant diseases such as diabetes mellitus, obesity, hypertension and its complications.
Blood heparins: do they have a lipid-lowering effect?
Low molecular weight heparins reduce blood cholesterol levels for 6 months.
Is there an alternative to statins in the group of lipid-lowering drugs, depending on the clinical course of atherosclerosis and which drug is best to start treatment with in this case?
Each drug has its own niche, but, for example, with homozygous hypercholesterolemia there is no benefit from statins, but probucol has found good use in this form of atherosclerosis.
From an economic point of view, it is necessary to start treatment with FFA, nicotinic acid, and then switch to statins.
It is not advisable to carry out lipocorrective therapy as part of primary prevention measures in men aged 35 years and in women with preserved menstrual function.
How does the development of atherosclerosis differ in men and women and is there a difference in approaches to treatment and the choice of lipid-lowering drugs in different sexes?
Before menopause, atherosclerosis practically does not develop in women, with the exception of those who have several risk factors. After menopause in women, the outcome of atherosclerosis is the same in men and women.
Atherosclerosis in the age aspect and the role of lipid-lowering therapy...
Previously, it was believed that atherosclerosis is an age-related pathology. If this is the case, then statins, for example, need to be taken for the rest of your life. Further research will show how justified this approach is.
Symptoms of atherosclerosis
The first period of atherosclerosis is the preclinical (asymptomatic) period. During this period, the disease does not make itself known in any way, while a high (exceeding the norm) amount of β-lipoproteins or cholesterol is detected in the human blood. Clinical manifestations occur only after the vessel becomes 50% narrower (or more). The symptoms of this disease depend on which artery or aorta is affected.
Atherosclerosis of cerebral vessels.
Symptoms:
deteriorated memory function, low poor performance, sleep problems, dizziness. As it progresses, the patient’s psyche becomes impaired. The following complications may also make themselves felt: thrombosis and hemorrhage.
Atherosclerosis of the heart vessels (coronary vessels).
Symptoms:
myocardial infarction, cardiosclerosis, angina pectoris.
Atherosclerosis of the thoracic aorta.
Symptoms:
severe pain behind the sternum, radiating to the upper abdomen or back and arm. Duration: the continuation of such pain occurs from a couple of hours and even up to several days.
Atherosclerosis of the abdominal aorta.
Symptoms:
constipation, flatulence, pain in the abdominal area; in addition, numbness of the legs and swelling of the feet may occur.
Atherosclerosis of the renal arteries.
Symptoms:
unilateral damage - gradual development and intensification of hypertension with constantly high blood pressure numbers; bilateral damage - arterial hypertension. Low back pain may also be present.
Atherosclerosis of the arteries of the lower extremities.
Symptoms:
pain in the calves or a feeling of weakness in them, a feeling of numbness in the legs.
Atherosclerosis of the penile arteries.
Symptoms:
erection problems, impotence.
Prevention of atherosclerosis in persons with risk factors and in patients with coronary heart disease
Preventive and therapeutic measures aimed against atherosclerosis and related diseases are carried out as part of primary and secondary prevention
. If primary prevention is understood as a set of measures that prevent the development and progression of atherosclerosis, then secondary prevention means measures taken to slow down the progression of the disease and reverse the development of the existing atherosclerotic process in the coronary and other arteries in people already suffering from coronary heart disease (CHD).
Risk factors for atherosclerotic diseases
The likelihood of developing cardiovascular diseases and their complications increases as the number and severity of risk factors increases, which include:
• belonging to older age groups;
• postmenopausal period for females;
• smoking;
• presence of arterial hypertension (BP>140/90 mm Hg);
• insufficient physical activity (lack of active physical exercise, at least 3 times a week for 30 minutes);
• excess body weight (20% more than ideal);
• family predisposition to IHD (presence of cardiovascular death, myocardial infarction, stroke in one, both parents and/or siblings before the age of 55 years);
• presence of chronic diseases leading to secondary dyslipidemia:
a) diabetes mellitus type I and II;
b) nephrotic syndrome;
c) chronic renal failure;
d) hypothyroidism.
Primary prevention of atherosclerotic diseases in the population implies a set of government measures aimed at preventing atherosclerosis of the vessels of vital organs and complications using non-drug methods of combating risk factors (arterial hypertension, smoking, hyper- and dyslipidemia, excess body weight, physical inactivity) and medications. The latter include lipid normalizing agents.
Research on primary prevention of atherosclerosis
To date, some experience has been accumulated in organizing and conducting large projects on primary prevention.
The Oslo Study
In 1981, the results of the so-called The Oslo Study
.
The study was devoted to exploring the possibility of primary prevention of coronary artery disease using an anti-atherosclerotic diet and smoking cessation. The research program was carried out starting in 1972 in the city of Oslo (Norway). From 16,202 practically healthy men 40–49 years old, 1,232 people with a high risk of coronary artery disease, but with normal blood pressure levels, were selected. The criteria for inclusion in the study were:
1) hypercholesterolemia in the range of 7.5–9.8 mmol/l;
2) high coronary risk – the upper quartile of the distribution (by blood cholesterol level, smoking and blood pressure level);
3) systolic blood pressure level is below 150 mm Hg.
Eligible men were randomized to an intervention group (lowering blood cholesterol levels through diet and smoking cessation) or a control group.
Particular importance was attached to assessing the actual nutrition of the intervention group, teaching them an anti-atherosclerotic diet and monitoring its compliance. It should be noted that those in the intervention group followed the recommended diet extremely carefully, as evidenced by Table 1. The daily diet of patients in the 4th year of observation can be called ideal: it complied with all recommendations for anti-atherosclerotic nutrition.
The total calorie content of the food is just over 2000, which is slightly hypocaloric for middle-aged men with moderate physical activity. Fat in the total diet was only 27%, the ratio of various fatty acids was simply ideal (PUFA/SFA = 1.01), and cholesterol intake was less than 300 mg (289 g/day).
The diet of the control group was very different from the diet of the intervention group. In many ways it is surprisingly similar to our diet. As is typical for us, fats occupied 44.1% of the total calories, daily cholesterol intake significantly exceeded the physiological norm (527 mg/day), the PUFA/SFA ratio of 0.39 indicated a 2.5-fold predominance of saturated fatty acids.
The smoking cessation intervention consisted of conversations about the dangers of smoking and the need to stop it (the conversations took place in the presence of the subject’s wife).
The observation of people included in the study lasted 5 years. Over 5 years, 1 person from the control group and 9 people from the intervention group abandoned the study. As can be seen in Fig. 1, during 5 years of observation in the intervention group, the level of cholesterolemia decreased significantly, although it still significantly exceeded the upper limit of normal, and the average number of cigarettes smoked decreased significantly (25% of people in the intervention group stopped smoking).
In table Table 2 presents data on mortality and other incidents in the compared groups. In the control group, 57 fatal and non-fatal myocardial infarctions and sudden deaths occurred per 1000 people; in the intervention group, their number was significantly lower - 31 (difference 45.6%; p < 0.028).
The total number of cardiovascular events (fatal and non-fatal) was 62 in the control group and 36 in the intervention group (difference - 42%, p = 0.038).
Overall mortality in the intervention group tended to be lower by 27.8%, but the difference was not significant. In any case, death from non-coronary causes was the same in both groups. Please note that there is no difference between the groups in the number of deaths from cancer, suicide and injury.
Thus, basic intervention against the two most important risk factors - hypercholesterolemia and smoking - has yielded excellent results.
Helsinki Heart Study
The first study to achieve the goals of primary prevention with drugs was the so-called Helsinki Heart Study.
The study was randomized, double-blind, and included patients were followed for 5 years. The age of those included in the study was between 40–55 years. Of the 23,531 people, 4,081 men were selected for the study. They met the protocol requirements and were screened. The study was carried out in 37 clinics in Helsinki.
The main group received gemfibrozil
600 mg 2 times a day, control – placebo.
After 5 years, it turned out that in those receiving gemfibrozil, the number of coronary events, non-fatal and fatal myocardial infarction, sudden coronary death, uncertified death was significantly less than in the control group: 56 (27.3%) versus 84 (41.4%; p<
0.02). For each of these incidents, the difference between the groups was not significant. The authors believe that the number of people included in the study and the length of their observation did not allow the true effectiveness of the treatment to be revealed. In the gemfibrozil group, deaths were primarily due to accidents, violence, and intracranial hemorrhage.
Thus, the Helsinki study showed that one of the representatives of fibrates actually helps to reduce the total number of “coronary” cases
, although it has no effect on overall mortality.
Very alarming were the increased incidence of suicide and traumatic death among those receiving gemfibrozil. This feature of the results obtained gave rise to all sorts of conjectures to explain this phenomenon. There were concerns about the impact of lowering lipid levels on the mental sphere. Moreover, it was initially unclear whether this phenomenon is common to all lipid-lowering drugs or is unique to gemfibrozil. In any case, until now, the authors of various lipid-correcting projects specifically calculate the frequency of suicides, murders and traumatic deaths in the patients of the main and control groups they observe.
LRC–CPPT
Another multicenter, randomized, double-blind LRC study is CPPT (The Research Clinics Coronary Primary Prevention Trial; 1984)
was conducted using
cholestyramine
under the guidance of the National Heart, Lung, and Blood Institute (USA) in 12 clinics. The study involved 3810 apparently healthy men aged 35–59 years with hypercholesterol levels over 265 mg/dl. After 7 years of study in the main group, the level of cholesterol and LDL in the blood, although it decreased significantly, actually remained significantly higher than normal. In addition, an increase in triglyceridemia was noted. It was found that the treatment reduced the risk of new cases of coronary artery disease by 25% over 7.2 years.
Thus, the positive effect of cholestyramine occurred against the background of a moderate decrease in blood levels of cholesterol and LDL and an increase in triglycerides.
The West of Scotland Coronary Prevention Study
The eighties were marked by the emergence of a large number of studies devoted to studying the effectiveness, tolerability and impact on clinical endpoints, the morphology of atherosclerosis in the coronary and peripheral arteries of a new class of lipid-lowering drugs - statins.
A major phenomenon in cardiology in recent years has been the results of The West of Scotland Coronary Prevention Study,
or the so-called
West of Scotland Study
, the results of which were published in 1995.
The study included practically healthy people aged 45–64 years who were diagnosed with moderate hypercholesterolemia.
Invitations were sent to 180 thousand men of the specified age, 81,161 people came to the 1st reception. At the 2nd appointment, 20,914 men were studied whose blood cholesterol levels were above 252 mg/dL (6.5 mmol/L). From this number, men with LDL cholesterol levels above 155 mg/dL (4 mmol/L) were selected. They were recommended an anti-atherosclerotic diet for 4 weeks and were invited to the 3rd appointment (13,654 people). Next, a second study of LDL cholesterol and ECG was performed. Those who had the following inclusion criteria for the study were invited to the 4th appointment: the LDL cholesterol level was in the range of 174–232 mg/dl (4.5–6.0 mmol/l), there were no serious ECG changes, no there were clinical signs of coronary artery disease (angina pectoris, previous myocardial infarction, high-grade arrhythmias).
Selected individuals were examined every 3 months, and dietary recommendations were repeated at each appointment.
The endpoints of the study were death from ischemic heart disease, nonfatal myocardial infarction, death from all cardiovascular causes, death from non-cardiovascular causes, and overall mortality.
Under the influence of pravastatin during the observation period, blood cholesterol levels decreased by 20%, LDL cholesterol by 26%, triglycerides by 12%, and HDL cholesterol levels increased by 5%.
As can be seen from table. 3, after 5 years, a significant reduction in the risk of coronary death and non-fatal myocardial infarction was revealed in patients of the main group (risk reduction by 31%, p <0.0001).
This significant reduction in the risk of coronary events was mainly due to a significantly lower number of non-fatal myocardial infarctions in the study group
.
Actual deaths from IHD occurred 52 in the control group and 38 in the main group (1.7 and 1.2%, respectively), which turned out to be unreliable due to the small number of deaths. There were 204 and 143 definite non-fatal myocardial infarctions, respectively (6.5 and 4.6%; p <0.001), which means a 31% reduction in risk for this criterion.
As can be seen from Fig. 2, already after 6 months the cumulative curves for the two groups begin to diverge, indicating a smaller number of definitely coronary deaths in the main group. Over time, this difference increases and turns out to be significant (p <0.001).
The authors strictly differentiated myocardial infarctions, beyond doubt and “possible,” as well as death from them. The number of deaths increases in the control group to 61 (1.9%), and in the main group to 41 (1.3%). Here the difference between the groups is already quite significant (p <0.041). At the same time, the risk reduction in people of the main group is 33%.
In various fragments of Fig. Figure 3 shows the cumulative curves of the two groups with different variants of the end points, including death from non-cardiovascular causes (the difference between groups is not significant) and death from all causes (the difference is significant).
In addition to reducing the incidence of death and myocardial infarction in Table. Figure 3 shows other, less stringent endpoints.
Thus, in particular, in patients of the main group there were fewer cases of the need for control angiography - 215 (6.8%) cases versus 295 (9.3%, p <0.001) and surgical interventions on the heart vessels - 51 (1.7%). %) case versus 80 (2.5%) cases, the difference is significant (p<0.001).
The authors analyzed the incidence of primary endpoints in the two groups depending on a number of factors. It turned out that pravastatin equally reduces the risk of death from non-fatal heart attacks regardless of age
(before or after 55 years), in
smokers and non-smokers, in persons with severe cholesterolemia
(>269 mg/dl) and
less severe
(<269 mg/dl),
in persons with a marked increase in LDL cholesterol levels
(>189 mg/dl )
and less pronounced
. It should be noted, however, that pravastatin was more effective in those with more severe hyperlipidemia (their risk reduction was greater by 10%). The effectiveness of treatment was the same with varying degrees of hypertriglyceridemia and hypo-a-cholesterolemia.
AFCAPS/TEX CAPS
AFCAPS/TEX CAPS study were presented at the 70th Congress of the American Heart Association
, completed by the University of Texas.
The study is devoted to the primary prevention of IHD among men and women aged 45–73 years with moderately increased cholesterol levels in the blood, without clinical manifestations of IHD. A total of 6605 people were observed and randomized into two equal groups: treatment with lovastatin
(20–40 mg/day) and placebo.
The period of treatment and observation was 5 years. It was shown that under the influence of treatment with lovastatin, the level of total blood cholesterol decreased by 18.4%, LDL cholesterol by 25%, triglycerides by 15%, and there was an increase in the concentration of HDL cholesterol in the blood by 6%
.
During treatment, the frequency of the first coronary incident (sudden death, myocardial infarction, unstable angina) in the intervention group decreased by 36% (p <0.001) ,
and the frequency of second-line end points also decreased: the need for CABG - by 33%, cases of unstable angina – by 34%, cases of fatal and non-fatal myocardial infarction – by 35%, all fatal and non-fatal cardiovascular incidents – by 24% (all differences compared to the placebo group are highly significant).
Clinical effects were more pronounced in women (-54%) than in men (-34%), and were significant in subgroups of the elderly (-29%), smokers (-59%), hypertensives (-43%) and diabetics (- 43%). Taking into account the fact that in patients with IHD, treatment with lovastatin significantly reduces the severity of myocardial ischemia, it can be argued that lovastatin is effective not only for secondary, but also for primary prevention of IHD in middle-aged and elderly people of both sexes, including those with such risk factors as like smoking, hypertension, diabetes.
Thus, primary and secondary prevention of atherosclerotic heart diseases are realistically feasible using both non-drug and drug-based approaches. Among the latter are representatives of fibrates (gemfibrozil), resins (cholesterolamine), statins (lovastatin and pravastatin). It should also be noted that the effectiveness of statins in achieving primary prevention goals was superior to that of gemfibrozil and cholestyramine. At the same time, quite favorable results were obtained with the combined use of an anti-atherosclerotic diet and smoking cessation.
Principles of secondary prevention of atherosclerosis
Patients suffering from coronary artery disease, especially those who have had acute myocardial infarction, unstable angina, or stroke, are considered to be at high risk of developing serious cardiovascular complications
. The likelihood of death and repeated myocardial infarctions, unstable angina and other complications (i.e., coronary risk itself) increases depending on the number and severity of the risk factors discussed above.
Secondary prevention for these people is individual and complex. It is based on the correction of existing lipid disorders to the target level, as well as the elimination of risk factors. Secondary prevention, in addition to these fundamental measures in patients who have suffered a myocardial infarction or other serious cardiovascular incident, involves prescribing the following medications for preventive purposes:
• antiplatelet agents, usually acetylsalicylic acid as a cheap and quite effective agent;
• b-blockers;
• angiotensin-converting enzyme inhibitors.
It is generally accepted that the anti-atherosclerotic effect and reduction in the risk of serious cardiovascular events, including death, are closely associated with the achievement of the so-called target blood lipid levels
– LDL cholesterol, total cholesterol, HDL cholesterol and triglycerides. Lipid factors in the previous sentence are placed in order corresponding to the rank of their importance.
Target lipid levels vary depending on overall risk:
• persons without coronary heart disease (CHD) who have 1 risk factor (low-risk persons)
it is necessary to reduce the level of LDL cholesterol < 160 mg/dl;
• persons without CAD, but with two or more risk factors (persons of average risk)
LDL level needs to be reduced to <130 mg/dL;
• patients with CAD, or any other atherosclerotic diseases (high-risk individuals)
it is necessary to reduce the level of LDL cholesterol to 100 mg/dl.
Studies on secondary prevention of atherosclerosis
SCRIP
Research – Stanford Risk Intervention Project (SCRIP)
– refers to non-drug methods of prevention.
In 1984–1987 out of 4771 candidates, the authors selected for the initial examination 538 men and women in whom coronary angiography revealed the main selection criterion - a narrowing of the lumen of one of the main coronary arteries by less than 70%. Of this number, 300 people were randomized into a group of patients receiving usual care in the community (155 people) or an intervention group (145 people). In the latter, measures were taken to eliminate or reduce risk factors, adherence to an anti-atherosclerotic diet, lowering the level of atherogenic blood lipids, quitting smoking, and increasing physical activity.
In patients of the main group, there was a significant decrease in the level of LDL cholesterol (-22%), apo B - (-22%), an increase in the level of HDL cholesterol - (+12%), a decrease in triglyceride levels (-20%), a decrease in body weight (- 4%), increased exercise tolerance (+20%), decreased fat intake (-24%) and dietary cholesterol.
These favorable changes in reducing risk factors led to the fact that by the end of the observation period, a significant difference in the severity of the minimum diameter of the affected segment was revealed. In the usual treatment group, there was a further narrowing of 0.051 mm, and in the intervention group - by 0.021 mm (i.e., half as much; p < 0.0003).
According to repeated coronary angiography, progression of atherosclerosis of the coronary arteries occurred in 41.4% of patients in the control group and in 29.3% in the main group (p <0.002). Regression of atherosclerosis was observed in 12.5% and 14% of cases, respectively, across groups.
The clinical course of the disease and its end points were more favorable for patients in the intervention group. Thus, non-fatal myocardial infarction occurred in 10 people in the control group, and in 4 people in the main group; CABG surgery was performed on 14 patients in the control group, 6 in the main group; total hospitalizations (death, acute myocardial infarction, CABG, balloon dilatation of arteries) were 44 in the control group, 25 in the main group (p <0.05).
The Lyon Diet Heart Study
The Lyon Diet Heart Study, better known in the literature as the “Mediterranean Diet”
, performed in a number of medical centers in Lyon (France), included 605 patients who had suffered a myocardial infarction, randomized equally into the main and control groups.
Patients in the main group were allowed to drink wine in moderation during meals. A diet common in the Mediterranean region was recommended, the composition of which boils down to the following: more bread, not a day without fruit, more red fruits, more greens, more fish, less meat (beef, lamb, pork should be replaced with poultry), and butter and cream should be replaced by poultry), and butter and cream should be replaced by margarine, which was provided to the sick free of charge. The duration of observation is 5 years.
Among 303 patients with CHD in the control group, 16 died from cardiovascular diseases over 4 years (of which 10 had sudden death), and in the main group - only 3 (sudden death - 0). This means that the mortality rate in the main group from CAD was 0.24% per year, in the control group - 1.32% (reduction in mortality - by 81.4%; p <0.02). There were 17 cases of non-fatal myocardial infarction during the observation period in the control group, 5 in the main group; death from other causes occurred in 4 and 5 people (p<1.0). The total number of deaths was 20 and 8, respectively, in the control and main groups (p <0.02). Reduction in overall mortality in the main group – 60%.
Thus, this work showed that secondary prevention using margarine enriched with linolenic acid is quite effective. Under its influence, mortality from cardiac causes, including sudden death, as well as the frequency of non-fatal myocardial infarction significantly decreases.
POSCH
POSCH study
is one of the most original in its method of influencing the atherosclerotic process. The work was carried out at a number of universities and medical institutions in the United States. A total of 838 patients were included in the study. The observation is cooperative, multicenter, randomized. Its purpose is to study the effect of partial shutdown of the small intestine on the state of lipid metabolism, long-term clinical (mainly cardiovascular) incidents, and the specific goal is to monitor the condition of the coronary arteries of patients using multiple repeated angiographic studies.
In patients of the main group, 2 m of the distal section or, if it was long, the entire distal third of the ileum was disconnected using shunting. Bowel patency was restored by connecting the proximal end of the ileum to the colon end-to-side and closing the distal end of the disconnected bowel.
By the end of the tenth year, the number of people with progression of coronary atherosclerosis according to the results of repeated angiography in the control group was 85%, and in the main group - 54%. Thus, the difference in the progression of coronary artery atherosclerosis between groups was 30.9%. This is a very good result (p<0.0002). Clinical results were also clearly better in patients of the main group. Thus, 10-year survival rate in the study group was significantly higher than in the control group (p <0.001).
Stenosing atherosclerosis of peripheral arteries occurred in 33.6% in the control group, and in 19.0% in the main group (p<0.001).
Over the years of observation, CABG surgery was performed in 137 patients in the control group and only in 52 patients in the main group (p <0.001).
Coronary artery ballooning was required in 33 patients in the control group and 15 in the main group; (p=0.005). Three patients from the control group underwent heart transplantation. The total number of cardiac surgical services provided to patients in the control group was 2.6 times higher than in patients who underwent small intestinal bypass surgery.
REGRESS
In recent years, with the advent of the group of statins, the possibilities of secondary prevention of atherosclerotic diseases and its implementation have been greatly simplified, and its effectiveness has increased markedly.
First of all, I would like to dwell on the REGRESS
, which included 885 men suffering from CAD with blood cholesterol levels ranging from 155–310 mg/dL (average 232 mg/dL).
Patients were randomized to receive placebo or pravastatin
(40 mg/day). In individuals of the main group, the level of cholesterol and LDL cholesterol reached the lower target value (190 mg/dl and 125 mg/dl, respectively).
According to serial quantitative coronary angiography, in those treated with pravastatin, the average diameter of the arterial segment decreased by 0.06 mm (from 28 mm to 2.74 mm), and in the control group - by 0.1 mm (p < 0.01). The minimum obstruction diameter decreased by 0.03 mm and 0.09 mm, respectively (p<0.001). This suggests that after two years of treatment with pravastatin, it was possible to prevent narrowing of the artery by 0.06 mm
. Progression of coronary artery atherosclerosis was observed significantly less frequently in patients treated with pravastatin (44% versus 55%; p <0.003).
During the observation period, 59 cardiovascular events occurred in the main and 93 in the control groups. There were significant differences in the number of emergency cases of balloon angioplasty of the coronary arteries performed (fewer in the group receiving pravastatin). Over 2 years, no clinical incidents were observed in 89% of patients taking pravastatin and in 81% of patients receiving placebo (p < 0.002).
MAAS
To the MAAS
381 patients were included, of whom 278 completed the four-year follow-up.
The main group of patients received simvastatin
20 mg once a night. The control group received a placebo.
Under the influence of simvastatin, blood cholesterol decreased by 32%, LDL cholesterol by 38%, triglycerides and apo B in the blood by 12%
; There were no significant changes in blood lipids in the control group.
According to the results of repeated coronary angiography, progression of the atherosclerotic process in the coronary arteries occurred in 41% of patients in the main group, and in 54% of patients in the control group; regression was observed in 17% and 9% of patients, respectively. The size of the lumen of the coronary arteries in the control group decreased by 0.08 mm, and in patients receiving simvastatin by only 0.02 mm (p <0.001).
Progression of atherosclerosis of the coronary arteries occurred in 32% of patients in the control group, and in 23% of patients in the main group. Reversal of atherosclerosis occurred in 19% of patients in the main group and 12% in the control group.
The number of various clinical incidents was greater in the control group (51 people) than in the main group (40 people). In the control group, 11 patients died (from cardiovascular complications - 5), and in the main group - 4 (all from cardiovascular complications). 11 and 7 patients in the control and main groups suffered myocardial infarction, respectively. The number of CABG and angioplasty of the coronary arteries was higher in the control group (51 versus 40 people). Thus, simvastatin is effective in stabilizing the atherosclerotic process in the coronary arteries of patients with coronary artery disease
.
Scandinavian Simvastatin Survival Trial (4S)
One of the most famous clinical studies examining the effect of lipid-correcting therapy on mortality during long-term follow-up is the Scandinavian Simvastatin Survival Trial or 4S, or the Scandinavian Study
.
The purpose of the study was to reduce overall and cardiovascular mortality in patients who had suffered a myocardial infarction and/or suffered from angina pectoris with a high level of hypercholesterolemia (5.5–8.0 mmol/l or 215–310 mg/dl).
In the study group, the levels of total cholesterol, LDL cholesterol and triglycerides decreased by 25%, 35% and 10%, respectively, compared with baseline values, and the level of HDL cholesterol increased by 8%. In the control group, these indicators increased by 1%, 1%, 1%, and 7%, respectively.
During the observation period, a total of 256 patients (12%) died in the control group and 182 (8%) in the main group. The relative risk of death during treatment with simvastatin was 0.70 (p=0.0003). The estimated 6-year survival rate (70 months), calculated using the Kaplan-Meier method, was 87.7% and 91.3% in the control and study groups, respectively. In the control group, there were 189 cases of death from CHD (74% of the total number of deaths), in the main group - 111 cases (61%).
The relative risk of death from CAD when taking simvastatin was 0.58, i.e. the reduction in the risk of coronary death was 42%.
LIPID
Study (The Long-Term Intervention with Pravastatin in Ischemic Disease)
is a multicentre study carried out at 87 centers in Australia and New Zealand. It was double-blind, randomized, placebo-controlled in nature. Its purpose was to study the effectiveness of 40 mg/day pravastatin in reducing mortality in patients under 75 years of age who had myocardial infarction or unstable angina and had hypercholesterolemia between 4.0 and 7.0 mmol/L (155 and 270 mg/dL). ). For inclusion in the study, 11,106 patients of both sexes were screened. 9014 people were randomized. Among the patients, there were 3692 people who underwent CABG, coronary artery ballooning, or both procedures. The average level of total cholesterol was 218 mg/dl, LDL cholesterol – 150 mg/dl, triglycerides – 158 mg/dl, HDL cholesterol – 37 mg/dl. The main and control groups were instructed and were on an anti-atherosclerotic diet. The study was scheduled to end in 1998, but in 1996 the Investigative Committee decided to terminate the study prematurely due to the clear benefit on the primary endpoints in subjects receiving pravastatin.
Conclusion
Thus, this very brief review shows that reducing the levels of atherogenic blood lipids to target values leads to the cessation of the progression of coronary atherosclerosis, its partial reverse development and, in connection with this, a fairly pronounced reduction in the risk of death from cardiovascular diseases. On this basis, the average life expectancy of the population increases and the quality of life of patients improves.
A comparative analysis of the above results gives reason to believe that the most effective and at the same time easily feasible prevention program is the use of statins - simvastatin, pravastatin and lovastatin.
References
1. ThC. Anrews, K. Raby, J. Barry, C.L. Naimi, E. Allred, P. Gans, A. Selwyn. “Effect of cholesterol reduction on myocardinal ischemia in patients with coronary disease.” Circulation. 1997; 95:324–8.
2. JR. Downs, PA. Beere, E. Whitney, M. Clearfield, M. Weis, J. Rachek, E.A. Stein et al. “Design and rationale of the Air Force Texas Corona Virus Atherosclerosis Prevention Study (AFCAPS/TexCAPS).” Am.J.Cardiol. 1997; 80:287–93.
3.MH. Frick, O. Elo, K. Haopa, P. Heinsalmi, P. Helo, J.K. Huttunen et al. “Helsinki Heart Study: Primary prevention trial with gemfibrazil in middle-aged men with dyslipidemia. Safety of treatment, changes in risk factors, and incidences of coronary heart disease.” New Engl.J.Med. 1987; 317(20):1237–45.
4. I. Hjermann, K.V. Byre, I. Holme, P. Leren. “Effect of diet and smoking intervention on the incidents of coronary heart disease. Report from the Oslo Study Group of a randomized trial in healthy men.” Lancet. 1981; December 12: 1303–10.
5. Lipid Research Clinics Program. “The Lipid Research Clinics Coronary Primary Prevention Trial Results. Reduction in incidence of coronary heart disease.” JAMA. 1984; 251(3):351–64.
6. Lipid Research Clinics Program. “The Lipid Research Clinics Coronary Primary Prevention Trial Results. II. The Relationship of reduction in incidence of coronary heart disease to cholesterol lowering'. JAMA. 1984; 251:365–74.
7. J. Shepherd, S.M. Cobbe, I. Ford, C. G. Islands, AR. Lorimer, et al for the West of Scotland Coronary Prevention Study Group. “Prevention of coronary heard disease with pravastatin in men with hypercholeaterolemia.” New. Engl.J.Med. 1995; 333(20):1301–7.
Simvastatin –
Zokor (trade name)
(Merck Sharp & Dohme Idea)
| Applications to the article |
| Fig.1. Dynamics of cholesterol content in the blood and frequency of smoking in patients in the intervention group (main) and control in The Oslo Study.a - cholesterol content in the blood of patients during the observation period; b — dynamics of the frequency of cigarettes smoked in the main and control groups during the observation period. |
| Secondary prevention of atherosclerosis is individual and complex. |
| Fig.2. Cumulative curves showing the percentage of coronary death and defined non-fatal myocardial infarction in the West of Scotland Study. |
| Rice. 3. Kaplan-Meier curves indicating the frequency of various clinical incidents in patients in the control and study groups in the West Scottish study. |
| Secondary prevention of atherosclerosis using margarine enriched with linolenic acid is quite effective |
Not everyone understands that atherosclerosis is a chronic disease of the arteries. Impaired lipid metabolism and cholesterol deposition in the vascular wall lead to changes. First, spots and stripes form on the wall of blood vessels, and this has no clinical manifestation. Later, a plaque forms and the lumen of the vessel gradually narrows, disrupting tissue nutrition from this artery. Progression of the process can lead to complete closure of the artery or to thrombosis (for example: plaque rupture).
There are several reasons predisposing to the development of atherosclerosis:
- hereditary dyslipidemia, significant changes are observed at a young age, cholesterol levels and its fractions are high,
- smoking,
- unhealthy diet
- physical inactivity,
- stress,
- high blood pressure,
- overweight,
- diabetes.
Atherosclerosis affects the aorta, large arteries, and their branches: coronary arteries, carotid arteries (common, internal), brachiocephalic, subclavian. Atherosclerotic changes affect the vertebral, renal, arteries of the lower and upper extremities, the celiac trunk, and mesenteric arteries. Most often the coronary and brachiocephalic arteries and arteries of the lower extremities are affected.
In cases where an atherosclerotic plaque partially closes the lumen of a vessel and narrows it, we speak of stenosis. Such situations lead to a heart attack. If a plaque ruptures, blood may become blocked in a smaller vessel. Embolism will lead to the development of stroke, myocardial infarction, and limb ischemia.
Preclinical stages of atherosclerosis do not cause subjective sensations. Significant narrowing of the coronary vessels will lead to an attack of angina pectoris and a heart attack. The person will experience squeezing, pressing pain behind the sternum.
When the vessels supplying the brain with blood are damaged, dizziness, unsteadiness of gait, memory loss, disturbances in speech, vision, motor functions of the limbs, and decreased sensitivity occur.
Atherosclerosis of the arteries of the lower extremities can cause lameness and pain in the legs, forcing you to stop when walking, decreased sensitivity, trophic ulcerations, and dry gangrene will also occur.
Preventing the development of atherosclerosis can reduce the risk of its development or progression.
To prevent the development of irreversible changes in blood vessels, it is important to be interested in your health, undergo annual medical examinations, monitor your weight and nutrition, be physically active, and eliminate bad habits.
The level of cholesterol and its fractions, blood glucose should not exceed normal levels. Maintain blood pressure up to 130/80 mm Hg. Art. , body mass index should be equal to 18.5 and no more than 25. Calculate BMI using the formula Weight (kg) / Height (m2). The patient can choose the necessary antihypertensive therapy with the doctor. Moderate physical activity. Physical activity must be adequate, taking into account existing cardiovascular, endocrine, pathology of the osteoarticular system, etc.
Achievable for most people, walking at a varying pace for 35 to 40 minutes can be an excellent cardio workout.
Treatment of atherosclerosis is carried out conservatively or surgically. The first visit to a general practitioner will allow you to assess the patient’s condition and determine the examination tactics and prescribe treatment.
Author - therapist Dymovskaya Elena Vitalievna
Types of atherosclerosis
There are different types of atherosclerosis. The classification of the disease is based on the site of origin of the process and, accordingly, on which organ receives insufficient blood circulation. The following types of atherosclerosis are distinguished:
- heart vessels (coronary atherosclerosis);
- cerebral vessels (cerebral atherosclerosis);
- aorta (in the abdominal/thoracic cavity);
- renal arteries;
- arteries of the lower extremities;
- arteries of the upper extremities;
- atherosclerosis of the penile arteries.
What you need to know about atherosclerosis, cholesterol and healthy lifestyle rules
What is atherosclerosis and why is it dangerous?
Almost everyone now knows that cardiovascular disease is the most common cause of disability and death in a person's most productive age. The basis of cardiovascular diseases is damage to the walls of blood vessels by ATHEROSCLEROSIS. People with blood vessels of the heart affected by atherosclerosis suffer from severe chest pain - angina pectoris, which often ends in myocardial infarction - death of the heart muscle. Atherosclerosis can affect the blood vessels that carry blood to the brain, and then brain disorders develop, including cerebral stroke—death of brain tissue.
It happens that atherosclerosis affects the vessels that carry blood to the muscles of the legs, then a person cannot walk due to unbearable pain, and in the final stage gangrene develops.
In everyday life, there are two incorrect opinions about atherosclerosis. One of them is that in younger people, atherosclerosis is not coming soon. Another thing is that in older people, I still have atherosclerosis and it is useless to resist it.
What are the risk factors for cardiovascular diseases and the most common of them - coronary heart disease
Large scientific epidemiological programs examining hundreds of thousands of people and monitoring them for decades have proven the existence of factors that greatly increase the likelihood of developing diseases associated with atherosclerosis at any age. They are called RISK FACTORS.
The most dangerous of them are: high blood cholesterol, high blood pressure and smoking, followed by diabetes/high blood glucose and overweight - obesity. The effect of one factor enhances the effect of the other, so their combination is especially dangerous. If you reduce the level of each risk factor, for example, lower the level of cholesterol in the blood, lower blood pressure, quit smoking, lose excess weight, then the overall likelihood of developing cardiovascular diseases will actually decrease, and the development of atherosclerosis will slow down. This is most proven to lower blood cholesterol levels.
What is cholesterol
Cholesterol is a fat-like substance that is vital for humans. It is part of the membranes of all cells of the body, there is a lot of cholesterol in the nervous tissue; bile acids necessary for digestion and steroid hormones are formed from cholesterol.
More than enough cholesterol is produced in the body (in the liver) for all these needs. But people also consume it with food, and often in excess. The main source of cholesterol is fatty animal products. If there are a lot of them in the diet, and there are few cholesterol-free vegetable oils, grains, vegetables and fruits, then the cholesterol level in the blood increases, and it turns from a necessary friend for the body into a mortal enemy.
What are lipoproteins
Not all blood cholesterol is equally dangerous: sometimes they talk about “good” and “bad” cholesterol. But cholesterol as a substance is all the same, it is simply found in the blood in different spherical particles - complexes with other fat and protein molecules - they are called LIPOPROTEINS. Some of them, low-density lipoproteins, carry cholesterol in the blood to peripheral tissues from the liver, where it is synthesized. If too many of these particles are formed or their breakdown is impaired, a lot of cholesterol accumulates in the blood, it is deposited in the walls of blood vessels, and connective (scar) tissue grows around its deposits. This is how an atherosclerotic plaque is formed, narrowing the lumen of the vessel and impeding blood flow. And then the cholesterol in low-density lipoproteins can be called “bad”.
There are different types of atherosclerotic plaques. The most malignant ones, with a large cholesterol core and a thin cap of connective tissue, are called unstable. Such a plaque ruptures easily and opens like an abscess into the lumen of the vessel. In response to this, the body tries to close the resulting damage with a blood clot. Often the thrombus cannot stop growing and closes, like a plug, the entire lumen of the vessel. The blood flow stops, and the organ tissue dies without oxygen and nutrients. If this happens in the heart, a myocardial infarction develops; if it happens in the brain, a cerebral stroke occurs. As can be seen from the above, the onset of such dangerous diseases is caused by an increased level of cholesterol, which is found in low-density lipoproteins. That is why it is called “bad”. In a detailed laboratory analysis of blood lipids (fats and fat-like substances), this indicator is abbreviated as LDL cholesterol.
But there are others in the blood - “good” lipid-protein complexes. They are called high-density lipoproteins (HDL). HDL captures and removes cholesterol from where it accumulates in the walls of blood vessels. By “cleansing” blood vessels of excess cholesterol, HDL prevents the formation of atherosclerotic plaques.
The higher the level of LDL cholesterol (cholesterol in the “bad” complexes) in the blood and the lower the level of HDL cholesterol (cholesterol in the “good” complexes), the faster atherosclerosis will develop.
Cardiologists around the world are of the opinion that every person over 20 years of age should know their cholesterol level. Moreover, it is necessary to do a blood test for “good” and “bad” cholesterol, i.e. detailed lipid analysis. Our Center operates a lipid clinic, so in the clinical diagnostic laboratory you can do a detailed analysis of your lipid profile, and also contact a lipidologist, a specialist who will competently advise you based on the results of laboratory tests. Depending on the cholesterol level and its distribution in “bad” and “good” complexes, as well as according to other examinations, the doctor decides on the need for dietary or drug correction and gives appropriate recommendations. It should be borne in mind that the price of drugs is not only the price of lowering cholesterol, but the price of prolonging a person’s active life.
So, if cholesterol is elevated, it is dangerous as a factor contributing to the development of atherosclerosis and severe cardiovascular diseases.
How to reduce bad cholesterol levels
Blood cholesterol levels can be reduced. To do this, try to change your lifestyle:
- improve your diet;
- stop smoking;
- move more.
Diet to lower cholesterol
- The basis of all cholesterol-lowering diets is to reduce the consumption of saturated (solid) fats, especially fats of animal origin (fatty meat, organ meats, butter, full-fat dairy products, baked goods, etc.) and replacing them with vegetable oils (sunflower, olive, corn ).
- Dairy products with reduced fat content, low-fat cheeses (no more than 30% fat), lean meat, baked goods with vegetable fats, fried fish, and potatoes fried only with vegetable fats are allowed in moderate (limited) quantities.
- Eggs can only be consumed boiled or fried in vegetable oil (omelet).
- More often use foods with reduced fat and cholesterol in your diet: wholemeal bread, whole grain bread, any cereals, pasta, low-fat dairy products, all kinds of vegetable dishes and fruits.
- Among meat products, you should prefer chicken, turkey, and veal. Remove fat and skin from poultry before cooking.
- Eat more fish, especially sea fish, you can introduce 2 fish days a week or eat one fish dish every day.
- Prefer desserts without fat, without cream, without sugar, preferably fruit ones.
- Pay special attention to regular consumption of foods that reduce cholesterol levels in the body and increase its elimination. They contain soluble fiber (pectin, psyllium, gluten) and form a jelly-like mass when cooked. These are oatmeal (rolled oats), apples, plums, and various berries.
- Eat legumes (beans, peas) regularly.
- When cooking, avoid frying in butter and animal fat; cook, stew, and bake more often. Use cookware with a special coating that does not require adding fat when cooking.
Recommendations for choosing food products:
| Types of products | Recommended | Consume in moderation | Exclude from food |
| Cereals | Whole grain bread, wholemeal bread, porridge, pasta | Fine flour bread | Butter bread |
| Soups | Vegetables | Fish | With meat broth |
| Dairy | Low-fat dairy products and cheeses | Half-fat dairy products and fats | Whole milk, cream, fatty dairy products and cheeses |
| Eggs | Egg white | Eggs | Scrambled eggs with animal fats |
| Seafood | Scallop, oysters | Mussels, crabs, lobsters | Squid, shrimp |
| Fish | All types, especially sea | Fried in vegetable oils, lightly salted | Fried in animal fats, hard margarines or unknown fats |
| Meat and poultry | Chicken, skinless turkey, veal, rabbit | Lean varieties of beef, lamb, ham; liver | Fatty meat, duck, goose, fatty sausages, pates |
| Fats | Vegetable liquid oils: sunflower, olive, soybean | Soft vegetable fat spreads containing no trans fats | Butter, meat fat, lard, hard margarines |
| Vegetables and fruits | Any fresh, frozen, steamed, boiled, legumes | Potatoes fried in vegetable oils | Potatoes and other vegetables fried in animal or unknown fats |
| Nuts | Almonds, walnuts | Peanuts, pistachios, hazelnuts | Coconut, salted |
| Dessert | NOT sweetened juices, fruit drinks, popsicles | Confectionery, baked goods, creams, ice cream with vegetable fats | Baked goods, sweets, creams, ice cream, cakes made with animal fats |
| Seasonings | Pepper, mustard, spices | Unsalted sauces | Mayonnaise, sour cream salted |
| Beverages | Tea, coffee, water, soft drinks | Alcoholic drinks - small/moderate amounts | Coffee or chocolate drinks with cream |
By carefully following a diet, you can reduce blood cholesterol by 10-12%.
This diet not only lowers the level of “bad” cholesterol, but also increases the level of “good” cholesterol.
If following a diet for 6-8 weeks does not lead to the desired reduction in the level of total blood cholesterol (less than 5 mmol/l) and LDL cholesterol (less than 3 mmol/l), and the risk of developing diseases caused by atherosclerosis remains high, then the doctor will raise the question on the prescription of cholesterol-lowering medications.
There are many such drugs now. The main thing is not to self-medicate after hearing enough advertisements about miraculous and safe food supplements. Among dietary supplements, only those that contain known food components that affect cholesterol, for example, soluble fiber preparations, can be effective. However, their effectiveness is no higher than a well-established diet; they only help its effect.
Of the medications used to lower blood cholesterol levels, doctors most often prescribe statins. These drugs in normal doses reduce cholesterol by 20-40%. Scientific studies have shown that statins not only reduce blood cholesterol, but also alleviate the course of diseases caused by atherosclerosis, reduce mortality from cardiovascular diseases and overall mortality. Using special studies of heart vessels, it was shown that treatment with statins slows the growth of atherosclerotic plaques and even causes them to shrink.
To give up smoking
It has been proven that both active smoking by a smoker and passive smoking by others increase the risk of developing many serious diseases, primarily cancer and cardiovascular diseases. Tobacco smoke contains a whole range of substances that are toxic to many organs and tissues (nicotine, carbon monoxide, hydrogen cyanide, carcinogens). Nicotine, for example, disrupts the tone of the vascular wall and contributes to its damage, spasms, and aggravates the formation of blood clots in blood vessels. Carbon monoxide, combining with hemoglobin, blocks the transfer of oxygen to organs and tissues. Components of tobacco smoke contribute to the development of arterial hypertension, a disruption in the system of cholesterol transfer into the walls of the vessel, exacerbating the deposition of cholesterol in them. A high total risk of developing CVD is created.
Sufficient physical activity
Sufficient physical activity is an integral part of a healthy lifestyle. The most accessible and fairly effective type of physical activity is brisk walking in the fresh air. You should exercise 5 times a week, for 30-45 minutes (up to 2 hours). The heart rate should reach 65-70% of that achieved at maximum load for a given age. The maximum heart rate for a particular person can be calculated using the formula: 220-age in years. For example, for a practically healthy person of 50 years old, the maximum heart rate is 220-50 = 170 beats per minute, and the heart rate that is recommended to be achieved during training is 110-120 beats per minute.
Many people do not have enough time for training, then it is necessary to use any opportunities for movement during the working day and after. For example, for people in “sedentary” professions, it is recommended to stand up to make a phone call or throw trash into a trash can, take the stairs instead of using the elevator, hold a short meeting while standing, etc.
The results of large studies have shown that the combination of regular physical activity with a reduction in periods of prolonged sedentary work through short breaks makes a complementary, significant contribution to the prevention of heart and vascular diseases.
In the presence of heart and vascular diseases, the physical activity regimen is selected by the doctor individually, strictly in accordance with the results of an electrocardiographic test with physical activity.
The text was prepared based on materials from Professor N.V. Perova, Department of Biochemical Markers of Chronic Non-Infectious Diseases, State Scientific Research Center for Preventive Medicine
To reduce blood cholesterol levels you need to:
— Reduce daily fat intake to 30% of total calories.
— There are fruits and vegetables. Start every meal with a vegetable salad. Eat foods low in fat. Replace butter with vegetable oil. Try to stew meat and vegetables rather than fry them.
Good to use
Fresh fruits and vegetables, greens, salad, low-fat cottage cheese, low-fat fish, cereals, bran
Should be consumed in moderation
Cereals, potatoes, legumes (peas, soybeans, beans, lentils), fruits and berries pureed with sugar, milk, fermented milk products (kefir, curdled milk, yogurt), low-fat hard cheeses, lean meat, chicken breast, turkey breast, eggs, bread, pasta, unsweetened juices
Should be avoided
Everything fried, lard, butter, margarine, mayonnaise, nuts, seeds, fatty meat, meat salads with mayonnaise, fatty sausages and meat products (bacon, brisket, ham, boiled pork, etc.), fatty fish, caviar, canned fish in oil , sour cream, cream, ice cream, fatty cheeses (more than 30% fat), sugar, candy, chocolate, jam, jam, marmalade, cakes, pastries, pies, sweet juices, cocoa, alcoholic drinks
- Move more. Let physical activity become regular. The more we move, the less cholesterol is deposited in our blood vessels.
- Quit smoking. Components of tobacco smoke increase blood cholesterol levels.
There are other fats that contribute to the development of atherosclerosis. These are triglycerides (TG). The desired blood TG level is less than 150 mg/dL (1.7 mmol/L). Controlling elevated TG levels is another important factor in helping prevent atherosclerosis.