Causes of megaloblastic anemia
Megaloblastic anemia develops due to a lack of folic acid (vitamin B9) and vitamin B12 (cyanocobalamin) in the body.
The following factors can lead to a decrease in vitamin B9 levels:
- Errors in nutrition, when a person sharply limits himself in food.
- Impaired absorption of vitamin B9 in the intestine. This occurs in various pathologies of the digestive tract, for example, enteritis, colitis, celiac disease.
- Previous resection of the stomach or intestines.
- There are certain periods in a person’s life when the need for folic acid increases sharply, for example, the period of gestation and breastfeeding.
- Some types of hemolytic anemia.
- Exfoliative dermatitis.
- Parasitic infestations, in particular diphyllobothriasis.
- Carrying out extrarenal blood purification.
- Liver pathologies: hepatitis and cirrhosis.
- Chronic inflammation of the pancreas.
- Alcoholism.
- Taking certain medications: oral hormonal contraceptives, anticonvulsants, etc.
Vitamin B12 deficiency in the body can develop for the following reasons:
- Refusal of food of animal origin and adherence to vegetarianism.
- Oncological damage to the gastric wall or the presence of polyps in the stomach.
- Resection of the stomach and small intestine.
- Pancreatic adenoma is ulcerogenic.
- Carrying a child and breastfeeding him.
- Celiac disease.
- Crohn's disease.
- Liver pathologies: hepatitis and cirrhosis.
- Transcobalamin II deficiency.
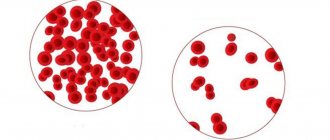
Vitamin B12 and vitamin B9 are directly involved in the formation of human DNA and RNA, and the cells of the red bone marrow and mucous membranes of the digestive system will be the first to suffer. They are the ones that divide faster than others in the body. In this pathology, erythrocyte precursor cells are not able to make a full transition to a more mature form. However, they do not die; their cytoplasm continues to grow and develop. As a result, large defective red blood cells, which experts call megaloblasts, begin to circulate in the blood.
Vitamin B12 enters the body with food. Its main source is animal products. In the stomach, it interacts with a special substance called gastromucoprotein. Vitamin B12 forms a complex compound with it and in such a bundle penetrates the small intestine, where it is absorbed into the blood. Every day a healthy person should receive from 3 to 7 mcg of vitamin B12. In the liver, normally, it contains from 3 to 5 mg - this is a cyanocobalamin depot. The body should receive more folic acid per day - about 100 mcg. Every day (with a standard diet) a person consumes from 300 to 750 mcg of folic acid. The body's depot contains about 5-10 mg of this substance.
Vitamin B12 contains 2 coenzymes. If there is a deficiency of the first coenzyme, then DNA is not able to form normally, which leads to a failure in the production of erythroid cells and the appearance of megaloblasts in the blood. The process of synthesis of leukocytes and platelets also suffers, but not to the same extent as red blood cells.
In addition, the lack of the first coenzyme prevents the body from producing an amino acid (methionine), which is part of the myelin sheaths that cover nerve trunks and cells. Therefore, the functioning of the nervous system as a whole is disrupted.
A deficiency of the second coenzyme, which is part of vitamin B12, leads to the body’s metabolism of fatty acids being disrupted. Toxins begin to accumulate in it, which damage the cells of the spinal cord. This pathology is called funicular myelosis.
MEGALOBLASTIC ANEMIA
Anemia
Megaloblastic anemia is a group of anemia caused by impaired DNA synthesis in erythrokaryocytes due to deficiency of vitamin B12 and/or folic acid and characterized by a megaloblastic type of hematopoiesis.
B12 deficiency anemia
Basic Information on Vitamin B12 Metabolism
Vitamin B12 enters the human body with food. It is found in meat, liver, kidneys, egg yolk, cheese, milk, and black caviar. In food, vitamin B12 is bound to protein. During culinary processing of food, as well as in the stomach under the influence of hydrochloric acid and proteolytic enzymes, vitamin B12 is released from food. Further in the stomach, vitamin B12 (extrinsic Castle factor) combines with proteins “R” (Rapid-binders). Then the complex “vitamin B12 + protein “R”” enters the duodenum, where, under the influence of proteolytic enzymes of pancreatic juice, protein “R” is split off and the released vitamin B12 combines with gastromucoprotein (internal Castle factor), which came here from the stomach. Gastromucoprotein is produced by parietal cells in the fundus and body of the stomach. The alkaline environment of the contents of the duodenum enhances the connection between vitamin B12 and gastromucoprotein. Gastromucoprotein protects vitamin B12 from the effects of proteolytic enzymes.
Next, the “vitamin B12 + gastromucoprotein” complex moves through the small intestine and enters the ileum, where, in the presence of Ca2+ ions, it interacts with specific receptors, after which it is broken down, and vitamin B12 enters the mitochondria of the cells of the mucous membrane. From here, vitamin B12 enters the blood, where it combines with transport proteins - transcobalamins. Transcobalamins are produced by hepatocytes, enterocytes, monocytes, fibroblasts, and hematopoietic precursor cells in the bone marrow. Transcobalamins deliver vitamin B12 to the liver and bone marrow. In these organs, vitamin B12 is released from the vitamin B12 + transcobalamin complex by lysosomal hydrolysis. Part of the vitamin B12 + Transcobalamin complex is eliminated in bile.
In the bone marrow, vitamin B12 is used for hematopoiesis, in the liver it is deposited and subsequently enters the blood if necessary. Part of vitamin B12 from the liver in the bile again enters the duodenum and is subsequently absorbed according to the mechanism described above.
With proper nutrition, a person's daily diet contains up to 30 mcg of vitamin B12. The daily requirement for vitamin B12 is 2-7 mcg. About 6-9 mcg of vitamin B12 is absorbed in the intestines per day. The body of a healthy person contains about 2-5 mg of vitamin B]2. The main organ that contains the largest amount of cobalamin is the liver. The reserves of vitamin B12 in the liver last for 3-5 years after its absorption ceases.
Vitamin B12 performs its biological role in the form of two coenzymes - methylcobalamin and deoxyadenosylcobalamin. The conversion of free vitamin B12 into B12 coenzymes occurs in several stages with the participation of specific enzymes in the presence of FAD (oxidized flavin adenine dinucleotide), reduced nicotinamide adenine dinucleotide, ATP and glutathione. With the help of these coenzymes, vitamin B12 carries out two important reactions.
The first reaction occurs with the participation of the coenzyme methylcobalamin 1 and ensures the maturation, development and reproduction of cells of the hematopoietic system, primarily the red hematopoietic germ and the epithelium of the gastrointestinal tract.
The second reaction, the breakdown and synthesis of fatty acids, occurs with the participation of the coenzyme deoxyadenosylcobalamin and ensures the conversion of the metabolic product of fatty acids, methylmalonic acid, into succinic acid. The normal course of this reaction ensures optimal metabolism of myelin in the nervous system and requires the presence of an active form of folic acid.
Etiology
The main reasons for the development of B12-deficiency anemia:
I. Violation of the secretion of “internal factor” by the stomach - gastromucoprotein.
- Atrophic autoimmune gastritis with the production of antibodies) to parietal cells and gastromucoprotein.
- Total gastrectomy (less commonly, subtotal gastrectomy).
- Congenital disorder of gastromucoprotein secretion.
- Stomach cancer.
- Gastric polyposis.
- Toxic effect of high doses of alcohol on the gastric mucosa.
II. Malabsorption of vitamin B12 in the small intestine:
- Resection of a section of the ileum (more than 60 cm).
- Malabsorption syndrome of various origins (enzymatic enteropathies, celiac disease, tropical sprue, enteritis, Crohn's disease, intestinal amyloidosis).
- Small intestinal cancer, small intestinal lymphoma.
- Chronic pancreatitis with impaired trypsin secretion.
- Congenital absence of receptors for the Vitamin B12 + gastromucoprotein complex in the ileum.
- Impaired absorption of vitamin B12 caused by drugs (colchicine, neomycin, biguanides, cimetidine, PAS, etc.).
III.Competitive consumption of vitamin B12:
- Infestation by worms (wide tapeworm, whipworm).
- Multiple diverticula of the small intestine with diverticulitis.
- Operations on the small intestine with the formation of “blind loops”.
IV. Increased consumption of vitamin B12:
- Multiple pregnancy.
- Chronic hemolytic anemia.
- Multiple myeloma and other neoplasms.
- Myeloproliferative diseases.
- Thyrotoxicosis.
- Violation of vitamin B12 intake from food. Veganism.
- Decreased vitamin B12 reserves. Severe cirrhosis of the liver.
- Violation of vitamin B12 transport. The absence of transcobalamin or the appearance of antibodies to it.
Impaired secretion of gastromucoprotein by parietal cells of the gastric mucosa
The most common cause of decreased secretion of gastromucoprotein by the gastric mucosa is atrophic gastritis. This disease of an autoimmune nature (autoimmune gastritis A) is accompanied by achylia, the absence of pepsin in the gastric juice and the production of antibodies to parietal cells that produce gastromucoprotein.
A common cause of B12 deficiency anemia is total gastrectomy or subtotal gastrectomy, which naturally results in loss of gastromucoprotein secretion. Due to the large supply of vitamin B12 in the liver, B12-deficiency anemia after gastrectomy develops only after 4-5 years.
Impaired gastromucoprotein secretion can develop when the gastric mucosa is damaged due to prolonged consumption of alcohol, especially pure alcohol.
A hereditarily determined congenital disorder of gastromucoprotein secretion is also possible.
An important and common cause of B12 deficiency anemia is stomach cancer, accompanied by atrophy of the gastric mucosa and cessation of gastromucoprotein production. Widespread gastric polyposis may also be accompanied by impaired gastromucoprotein production and the development of B12-deficiency anemia.
Impaired absorption of vitamin B12 in the small intestine
Most often, impaired absorption of vitamin B12 in the small intestine is caused by severe malabsorption syndrome associated with fermentopathy, celiac disease, tropical sprue, chronic enteritis, and Crohn's disease. Resection of the small intestine, amyloidosis, lymphoma, and cancer of the small intestine also lead to impaired absorption of vitamin B12. In some cases, the absorption of vitamin B12 is associated with a disruption in the production of trypsin by the pancreas in chronic pancreatitis, which disrupts the cleavage of protein “R” in the duodenum and, thus, the formation of the “vitamin Bc + gastromucoprotein” complex.
Sometimes impaired absorption of vitamin B12 is caused by the use of certain medications - colchicine, neomycin, cimetidine, PAS, biguanides, but this is a rare cause of little practical significance.
Competitive consumption of vitamin VP
Competitive consumption of vitamin B12 is observed during invasion by the broad tapeworm, which, living in the small intestine, absorbs vitamin B]2 that comes here; with “blind loop” syndrome (due to the imposition of anastomoses, “blind” sections of the intestine remain, in which the contents stagnate and microflora multiply, absorbing vitamin B12); with multiple diverticula of the small intestine (in this case, the situation is the same as with the “blind loop” syndrome).
Violation of vitamin B12 intake from food
Violation of the intake of vitamin B12 from food is rarely observed in people who are strict, convinced vegetarians and do not consume food of animal origin (meat, fish, liver, kidneys, etc.), as well as dairy products and eggs.
Decreased vitamin B12 reserves
A decrease in vitamin B12 reserves can be observed with cirrhosis of the liver, rarely with chronic hepatitis.
Violation of vitamin B transport
Violation of vitamin B12 transport is observed with transcobalamin deficiency. This is a very rare disease.
Pathogenesis
With a deficiency of vitamin B12, the following disorders develop.
A deficiency of the coenzyme vitamin B12 methylcobalamin leads to disruption of the synthesis of thymidine, which is included in DNA, as a result of which DNA synthesis and mitosis processes in the body's cells are disrupted. Fast-growing tissues are most significantly affected - bone marrow cells, epithelium of the gastrointestinal tract. Bone marrow cells lose their ability to mature normally. Violations of the red hematopoietic germ are especially pronounced. A large number of megaloblasts appear - megaloblastic erythropoiesis is characterized by a delay in the maturation of erythrokaryocyte nuclei in comparison with the degree of hemoglobinization of the cytoplasm, a reduction in the life span of red hematopoietic cells, and an increased breakdown of megaloblasts in the bone marrow.
Thus, erythropoiesis in B12-deficiency anemia becomes ineffective, which is confirmed by the discrepancy between the increased number of erythrokaryocytes in the bone marrow and a sharp decrease in the content of reticulocytes in the peripheral blood, an increase in serum iron and a decrease in the inclusion of radioactive iron in erythrokaryocytes.
At the same time, there is a violation and ineffectiveness of granulocytopoiesis and thrombocytopoiesis. Giant forms of platelets and granulocytes appear; in addition, phagocytosis of neutrophils by bone marrow macrophages increases. There is a possibility of the appearance of autoantibodies to neutrophils, which also contributes to the development of neutropenia in patients with B12-deficiency anemia.
Thus, deficiency of vitamin B12 and, accordingly, the coenzyme methylcobalamin leads to ineffective hematopoiesis with the development of megaloblastic anemia, leukopenia and thrombocytopenia. In addition, methylcobalamin deficiency leads to impaired maturation of epithelial cells of the gastrointestinal tract and causes the development of atrophy of the mucous membrane of the stomach and small intestine.
A deficiency of the coenzyme vitamin B12 deoxyadenosylcobalamin leads to disruption of fatty acid metabolism and the accumulation of large amounts of methylmalonic and propionic acids, which are toxic to the nervous system. In the absence of vitamin B12, methylmalonic acid is not converted to succinic acid. As a result of these disorders, damage to the posterior and lateral columns of the spinal cord develops, and myelin synthesis in nerve fibers decreases.
Clinical picture
The development of the disease is typical mainly for the age of 60-70 years. At the age of 30-40 years, the disease occurs with a frequency of 1 case per 5000 people, at the age of 60-70 years - 1 case per 200 people.
The clinical picture of B12 deficiency anemia is characterized by damage to three systems: digestive, hematopoietic and nervous.
Damage to the digestive system
In the vast majority of patients, symptoms of damage to the digestive system (primarily subjective) may be the earliest signs of the disease. Patients complain of a decrease, sometimes even lack of appetite, a feeling of heaviness and fullness in the epigastric region after eating, belching of eaten food and air, pain and burning in the tongue, in the gums, lips, and sometimes in the rectum. These complaints from patients are caused by the development of glossitis, atrophic gastritis and atrophic changes in the intestinal mucosa. Some hematologists explain the lack of appetite by brain hypoxia and inhibition of the appetite center in the hypothalamic zone.
When examining the oral cavity, attention is drawn to inflammatory-atrophic changes in the mucous membrane of the oral cavity and tongue. B12-deficiency anemia is characterized by a smooth, “varnished” tongue with atrophied papillae, cracked, with areas of bright red inflammation (the entire tongue may be inflamed and red), sometimes with ulcerations. It should be emphasized that glossitis is observed only with a significant and long-term deficiency of vitamin B12, in approximately 25% of patients. Glossitis is characteristic not only of B12-deficiency anemia, it can also be observed with iron deficiency anemia. The mucous membrane of the oral cavity is pale, and aphthous stomatitis may occur.
Palpation of the abdomen reveals mild pain in the epigastric region (not a permanent sign), and enlargement of the liver and spleen is often observed. If the development of B12-deficiency anemia is caused by impaired absorption of vitamin B12 in the small intestine, then in the clinical picture, along with the anemia syndrome, there are usually clearly defined symptoms of malabsorption syndrome.
Damage to the hematopoietic system
Disturbance of the hematopoietic system is the leading one in the clinical picture of the disease and is characterized by anemia of varying severity. Patients present complaints characteristic of anemic syndrome. The skin is usually pale, very often with a lemon-yellow tint (due to hyperbilirubinemia caused by hemolysis).
Due to anemia, especially if it is significantly pronounced, memory and mental performance decrease. Sometimes with B12-deficiency anemia, body temperature rises (not higher than 38°C).
Damage to the nervous system
Changes in the nervous system with B12-deficiency anemia are a characteristic sign of this disease and, as a rule, are observed in severe and long-term cases. Damage to the nervous system in B12-deficiency anemia is called funicular myelosis and is characterized by involvement of the posterior and lateral columns of the spinal cord. Demyelination occurs, followed by degeneration of nerve fibers in the spinal cord and spinal nerves. Patients complain of weakness in the legs, especially when climbing stairs, when walking quickly, a crawling sensation in the legs, numbness in the legs. Patients feel that they do not feel support under their feet when walking. It seems that the foot is not stepping on solid ground, but on something loose, soft, like cotton wool. This forces patients to repeatedly “test the ground with their feet.” These complaints are caused by a violation of proprioceptive sensitivity. Neurological symptoms are largely determined by the predominant damage to the posterior or lateral columns of the spinal cord. When damage to the posterior columns predominates, deep, spatial, vibration sensitivity is impaired; sensory ataxia and difficulty walking appear; tendon reflexes decrease; atrophy of the muscles of the lower extremities is observed. With severe damage to the posterior columns of the spinal cord, dysfunction of the pelvic organs (urinary incontinence, fecal incontinence) may occur.
When damage to the lateral columns of the spinal cord predominates, the neurological symptoms are different: lower spastic paraparesis develops with a sharp increase in tendon reflexes and muscle tone of the lower extremities; dysfunction of the pelvic organs is characterized by retention of urination and defecation.
Laboratory data
Examination of peripheral blood and bone marrow are crucial in diagnosing the disease.
General blood analysis. The development of hyperchromic macrocytic anemia (color index more than 1.1) is typical, but in rare cases anemia can be normochromic. The erythrocytes are large (macrocytes), anisocytosis (different sizes of erythrocytes, along with macrocytes there are erythrocytes of normal size), poikilocytosis (changes in the shape of erythrocytes) are also characteristic. Many megalocytes (macrocytes) contain nuclear remains (Jolly bodies, Cabot rings), and basophilic punctuation may be present.
Normoblasts are often found in the peripheral blood; the number of reticulocytes in most patients is reduced or normal. The number of leukocytes is reduced, neutropenia, eosinopenia, and relative lymphocytosis are determined.
B12-deficiency anemia is extremely characterized by the appearance of large segmented neutrophils with a polysegmented nucleus.
The platelet count is reduced, but, as a rule, there are no hemorrhagic manifestations, because thrombocytopenia does not reach a critical value.
Myelogram. Analysis of sternal puncture is crucial for making the diagnosis of B12 deficiency anemia.
Characteristic signs of B12-deficiency anemia that allow verification of the diagnosis are:
- irritation of the red hematopoietic germ, its hyperplasia; cells of the red row predominate over the cells of the white row, the leuco/erythro ratio becomes equal to 1:2, 1:3 (at a norm of 3:1, 4:1);
- the appearance of megaloblastic type of hematopoiesis;
• changes in myeloid cells - they increase in size, large metamyelocytes (young), band, segmented neutrophils are found; the appearance of hypersegmented neutrophils is characteristic;
• impaired maturation of megakaryocytes, expressed in impaired release of platelets (non-permanent sign). In severe cases of the disease, a decrease in the number of megakaryocytes and changes in their nuclei, reminiscent of changes in megaloblasts, may be observed. Biochemical blood test - there are no specific changes. However, with B12-deficiency anemia, hemolytic syndrome is quite often observed, caused by the intramedullary breakdown of erythrokaryocytes, as well as a shortening of the life span of peripheral erythrocytes. This is manifested by unconjugated hyperbilirubinemia. It is possible to increase the level of LDH and LDH2 in the blood - usually in proportion to the severity of anemia. There is often a moderate increase in iron content in the blood serum (mainly with the development of hemolysis syndrome).
Analysis of urine and feces - with the development of hemolysis, urobilin is detected in the urine, and in the feces - the amount of stercobilin is increased.
Schelling's test - allows you to evaluate the absorption of vitamin B12 in the intestine in the presence of gastromucoprotein or without it and make a conclusion about the pathogenetic variant of B12-deficiency anemia (it is caused by gastromucoprotein deficiency or impaired absorption of vitamin B12). The patient is given radiolabeled vitamin B12 to take orally. element and after 1-6 hours, a “loading dose” of unlabeled vitamin B12 is administered intramuscularly to saturate the liver depot. Then the content of radioactive vitamin B12 in 24-hour urine is measured. A decrease in its excretion indicates a malabsorption of vitamin B12 in the intestine.
Instrumental studies
Esophagogastroduodenoscopy - atrophic changes in the mucous membrane of the digestive tract are observed. The most typical development is diffuse atrophic gastritis, duodenitis; atrophic esophagitis can be detected (much less often). A biopsy of the mucous membrane confirms the presence of atrophic gastritis.
A study of gastric secretion reveals a sharp decrease in the amount of gastric juice, the absence of hydrochloric acid (Achilia) and pepsin, sometimes hydrochloric acid is detected, but its level is very low. In B12-deficiency anemia, caused by impaired absorption of vitamin B12 in the small intestine or infestation of the broad tapeworm, the secretion of hydrochloric acid is significantly reduced, however, stimulants of gastric secretion (histamine, pentagastrin) increase the level of hydrochloric acid in the gastric juice.
X-ray of the stomach - violations of the evacuation function of the stomach, flattening and smoothing of the folds of the mucous membrane are detected.
Diagnosis
Diagnostic criteria for B12 deficiency anemia:
I. Basic diagnostic criteria.
- Hyperchromic nature of anemia (relatively rarely the color indicator is normal).
- Characteristic changes in peripheral blood erythrocytes: increase in diameter (macrocytosis), volume, preservation of nuclear remnants (Jolly bodies, Cabot rings), reticulocytopenia.
- Characteristic changes in peripheral blood leukocytes: leukopenia, hypersegmentation of neutrophils.
- Thrombocytopenia. Characteristic changes in the myelogram: the appearance of megaloblasts in the bone marrow, hyperplasia of the red hematopoietic lineage, hypersegmentation of neutrophils (sternal puncture should be performed before treatment with vitamin B12, since even 1-2 injections of vitamin B12 lead to the disappearance of megaloblasts).
- Development of the clinical picture of funicular myelosis (usually with severe and prolonged course of the disease).
- Low levels of vitamin B12 in the blood (Determination of vitamin B12 in the blood is most often carried out using the radioimmunological method.
II. Additional diagnostic criteria.
1. Atrophic gastritis, absence of hydrochloric acid, pepsin and gastromucoprotein in gastric juice (80-90% of patients have classic pernicious anemia caused by gastromucoprotein deficiency).
2. Detection in the blood of antibodies to gastric parietal cells, gastromucoprotein or the “vitamin B12 gastromucoprotein” complex.
3. Positive Schelling test result.
4. Increased urinary excretion of methylmalonic acid.
5. Positive result of trial therapy with vitamin B12. On days 5-7 of treatment, the number of reticulocytes in the peripheral blood increases sharply (reticulocyte crisis).
Once a diagnosis of B12 deficiency anemia has been made, it is necessary to find out the cause of vitamin B12 deficiency. In most patients, we are talking about a violation of the synthesis of “internal Castle factor” (gastromucoprotein) due to the development of diffuse atrophic gastritis (usually of autoimmune origin). The diagnosis of diffuse atrophic gastritis is easily established using fibrogastroscopy and biopsy of the gastric mucosa.
Folate deficiency anemia
Folate deficiency anemia belongs to the group of megaloblastic anemias. The development of the megaloblastic type of hematopoiesis is due to the fact that with folic acid deficiency, the effect of vitamin B12 on DNA synthesis is disrupted.
Understanding Folic Acid Metabolism
Folic acid is a water-soluble, heat-labile vitamin. In food products and in body cells, folic acid is contained in the form of folic acid salts - polyglutamates (folates). Folates are found in meat, liver, plant foods (spinach, asparagus, lettuce, legumes, vegetables, fruits, mushrooms), yeast, and milk.
During culinary processing and long-term cooking, more than 50% of folates are destroyed, therefore, to meet the body's needs for folates, it is necessary to consume fresh vegetables and fruits. Folate absorption occurs in the duodenum and proximal jejunum. First, dietary folate is converted into monoglutamate in the intestine. Next, 5-methyl-tetrahydrofolate is formed, which enters the blood. In the blood, 5-methyltetrahydrofolate binds to various proteins and enters the liver and rapidly proliferating bone marrow cells. The penetration of folates through the membrane and their accumulation in the cell occurs with the participation of vitamin B12. In cells, methyltetrahydrofolate is converted to tetrahydrofolic acid (tetrahydrofolate), which is then transformed into polyglutamine tetrahydrofolate. It is assumed that this mechanism allows folic acid to be retained in the cell. Folic acid is involved in the following biochemical reactions:
- together with vitamin B12, it participates in the synthesis of thymidine monophosphate from uridine phosphate. Thymidine monophosphate is involved in the synthesis of pyrimidine bases and DNA. Therefore, folic acid is essential for DNA synthesis. For these purposes, the active form of folic acid is used - 5-10-methyltetrahydrofolic acid;
- participates in the synthesis of purine bases, which are part of DNA and RNA;
- takes part in the formation of glutamic acid from histidine; the intermediate product of this reaction is formiminine glutamic acid. The coenzyme of folic acid, tetrahydrofolic acid, is involved in the formation of glutamic and formamineglutamic acids. With a deficiency of folic acid, DNA synthesis in hematopoietic cells is disrupted, and megaloblastic anemia develops.
Indicators of normal folic acid metabolism:
- The daily requirement for folic acid is 100-200 mcg.
- The total amount of folic acid supplied from food in a nutritious diet is 500-600 mcg/day.
• The amount of folate absorbed in the intestine is 400-480 mcg/day.
- The total folate content in the body is 5-10 mg.
- The period during which the depot provides the need for folic acid when its intake into the body ceases is 4-5 months.
Etiology
Insufficient intake of folate from food
Nutritional folate deficiency is a common cause of folate deficiency anemia. It develops with insufficient consumption of vegetables and fruits, meat and other foods containing folates, as well as with improper cooking. Folate deficiency anemia can develop in infants when fed goat's milk, various nutritional formulas containing very little or no folate; when excluding vegetables, fruits, and meat from the diet.
Malabsorption of folate in the small intestine
The reasons that impair the absorption of folate in the intestine are similar to those that impair the absorption of vitamin B12: .
• congenital disorders of folate transport through the wall of the small intestine;
• extensive resection of the small intestine, especially the jejunum;
• enzyme-deficient enteropathies (gluten enteropathy - celiac disease, disucrose-deficient enteropathies);
• malabsorption syndrome of various origins (enteritis, exudative hypoproteinemic enteropathy, Whipple's disease, intestinal amyloidosis, Crohn's disease, etc.);
• “cecum” syndrome;
• tumor diseases of the small intestine.
Increased need for folate
An increased need for folate is observed in children of any age, but especially often in children of the first year of life, as well as during periods of intensive growth and puberty. An increased need for folate is typical for pregnancy, chronic inflammatory diseases, chronic hemolytic anemia, exfoliative dermatitis, malignant neoplasms, including hematological malignancies.
Chronic alcohol intoxication
Alcohol impairs the absorption of folate in the small intestine, so chronic alcohol abuse can lead to folate deficiency anemia.
Increased folate loss
It can be observed with severe liver cirrhosis (folate depot in the liver decreases), hemodialysis, and heart failure.
Taking medications
Some medications can cause folate deficiency anemia. The mechanism of action of the drugs is different:
- impaired absorption and use of folic acid is caused by cycloserine (an antibacterial drug for the treatment of tuberculosis and urinary tract infections); anticonvulsants (diphenylhydantoin or diphenine, hexamidine or primidone, phenobarbital); metformin (a biguanide for the treatment of type II diabetes mellitus);
- inhibition of the enzyme dihydrofolate reductase is caused by chloridine, pentamidine, bactrim, biseptol, sulfalazine, aminopterin and methotrexate (cytostatic drugs), triamterene (potassium-sparing diuretic);
- inhibition of pyrimidine synthesis is observed during treatment with the cytostatic 5-fluorouracil;
- inhibition of the enzyme ribonucleotide reductase is caused by the cytostatics cytosine arabinoside and hydroxyurea.
Pathogenesis
The above etiological factors lead to a decrease in the formation of the active form of folic acid - 5,10-methylenetetrahydrofolic acid, necessary for the synthesis of thymidine monophosphate from uridine monophosphate. As a result, DNA synthesis in hematopoietic cells is disrupted and megaloblastic anemia develops.
Clinical picture
The disease most often develops in children, young people and pregnant women.
Patients present complaints characteristic of anemia of any origin - a nonspecific anemic syndrome is noted. However, unlike B12-deficiency anemia, there are no complaints caused by damage to the nervous system; patients are not bothered by the sensation of crawling on the legs, numbness of the legs, or sensory disturbances. There are also no complaints caused by glossitis (pain and burning in the tongue). Upon examination, attention is drawn to the paleness of the skin and subicterus.
When examining the internal organs, one can detect a slight enlargement of the spleen (a variable sign) and myocardial dystrophy syndrome (muffled heart sounds, quiet systolic murmur at the apex, disturbance of the repolarization phase of the left ventricular myocardium on the ECG in the form of a decrease in the amplitude of the T waves).
Unlike B12-deficiency anemia, folate deficiency anemia is characterized by the absence of atrophic glossitis, atrophic gastritis and achylia.
There are no neurological symptoms of funicular myelosis in folate deficiency anemia, since the spinal cord columns are not affected.
Laboratory data
Complete blood count - the same signs are characteristic as for B12-deficiency anemia.
Biochemical blood test - an increase in the amount of unconjugated bilirubin (due to hemolysis of red blood cells) and a decrease in the content of folic acid in the blood and red blood cells may be observed.
Myelogram - characterized by hyperplasia of the red hematopoietic lineage, the appearance of a large number of megaloblasts, hypersegmented neutrophils.
Histidine test - the patient takes 15 g of histidine, after which the urinary excretion of formiminoglutamic acid is determined 8 hours after taking histidine. Normally, the main part of histidine is converted with the participation of folic acid into glutamic acid, and from 1 to 18 mg of formiminine glutamic acid is excreted in the urine. In folate deficiency anemia, the secretion of formiminoglutamic acid increases significantly.
Diagnostic criteria for folate deficiency anemia
1. General analysis of peripheral blood: hyperchromic anemia, macrocytosis of erythrocytes, hypersegmentation of neutrophils, leukopenia, thrombocytopenia.
2. Myelogram - detection of megaloblasts, hypersegmented neutrophils.
3. Absence of glossitis, atrophic gastritis.
4. Absence of funicular myelosis.
5. Normal blood levels of vitamin B12.
6. Reduced folic acid content in blood serum and red blood cells.
7. Normal daily urinary excretion of methylmalonic acid.
Symptoms of megaloblastic anemia
Most often, megaloblastic anemia develops due to a lack of vitamin B12 in the body. All symptoms of this disorder are combined into four large groups:
- Symptoms associated with disorders of the digestive system. With megaloblastic anemia, atrophic changes occur in the mucous membranes of the stomach and intestines, and there is also a lack of production of enzymes necessary for normal digestion of food. This leads to patients making the following complaints:
- Lack of desire to eat.
- Aversion to meat dishes.
- Painful sensations in the tongue, distortion of taste. The tongue may become brightly colored and covered with a shiny film (Gunther's atrophic glossitis).
- Complaints of nausea, which may periodically result in vomiting.
- Stool disorders (diarrhea).
- Symptoms of funicular myelosis.
- Headache.
- Sensitivity disorders in the form of “goosebumps”, tingling of the skin, etc.
- Feeling of cold in the extremities, deterioration of their sensitivity.
- Changes in a person's gait.
- Decreased muscle strength, and with severe anemia, the patient develops paralysis.
- Circular hypoxic syndrome. Its manifestations:
- Feeling of constant weakness.
- Increased fatigue.
- The appearance of shortness of breath. At first it occurs against the background of physical activity, and then begins to bother, even when the person is resting.
- Cardiopalmus.
- Painful sensations in the chest (heart pain).
- The skin becomes unnaturally pale or even icteric.
- Symptoms caused by disorders of the nervous system:
- The person becomes more irritable and becomes very nervous.
- Hallucinations may occur.
- Convulsions occur periodically.
- Mental abilities deteriorate.
At the beginning of the development of anemia, a person may not make any complaints, since there will be no pathological symptoms during this period. There may be a slight deterioration in health, fatigue and mild dyspepsia. As a rule, patients do not go to doctors during this period. Although already at this time it is enough to do a blood test to identify developing anemia.
As the disease progresses, symptoms begin to increase in severity. If a person already has any chronic pathologies, their symptoms will worsen. For example, this is true for angina and arrhythmia. Swelling also appears on the legs and arms, as well as on the face.
In old age, anemia most often has a hidden course. Patients do not indicate to the doctor that they feel unwell, which makes diagnosis difficult.
What diseases can it be associated with?
Megaloblastic anemia develops against the background of malabsorption in the digestive system caused by diseases of the stomach, small intestine and competitive absorption of cyanocobalamin in the intestine.
This is observed in the following conditions:
- violation of the secretion of internal factor in atrophic gastritis caused by hereditary, toxic, immunological factors,
- during gastrectomy,
- with partial resection of the stomach;
- for tumors,
- with blind loop syndrome,
It should be remembered that hyperchromic anemia in elderly people often occurs due to tumor processes (stomach cancer), for which an instrumental examination of the digestive system is performed (fibrogastroscopy, colonoscopy, X-ray examination, etc.). Megaloblasts are found in the bone marrow of leukemia. With metastases of malignant neoplasms to the bone marrow (except for stomach cancer), normochromic anemia usually occurs.
How to detect megaloblastic anemia?
The search for the correct diagnosis begins with collecting anamnesis and listening to the patient’s complaints. An experienced doctor may suspect anemia already at this stage.
Patient examination includes the following steps:
- Examination of the skin: it is pale, sometimes with a yellowish tint (“parchment skin”).
- The tongue is red and shiny, painful and slightly swollen.
- When listening to the heartbeat, systolic murmurs and tachycardia are diagnosed.
- When palpating the peritoneum, an enlarged spleen is palpated.
- There are also signs of funicular myelosis.
The next stage of diagnosis is donating blood for clinical analysis. The results of the study will reveal a decrease in the number of red blood cells and hemoglobin, the color index of the blood exceeds 1.1. Sometimes anemia is accompanied by thrombopenia and leukopenia. Macrocytes and megaloblasts are also visualized in the blood. Blood cells change their normal shape and size. Another sign of megaloblastic anemia is the presence of Kebbot rings and Jolly bodies in the blood. The reticulocyte level is decreased.
There is also a deficiency of folic acid and vitamin B12 in the serum part of the blood. Serum iron levels remain within normal limits or increase, which is caused by the accelerated destruction of red blood cells. This fact also provokes a jump in bilirubin in the blood.
Studying the bone marrow, which is obtained by performing a sternal puncture, allows us to clarify the diagnosis. The study must be carried out in advance, that is, before starting treatment. The fact is that taking vitamin B12 will return the composition of the bone marrow to normal within 1-2 days, and the signs of megaloblastic anemia will be stopped.
The vast majority of patients are diagnosed with damage to the mucous membranes of the digestive system with their atrophic changes. The production of hydrochloric acid in the stomach decreases.
Thus, the diagnosis of megaloblastic anemia consists of 3 main stages:
- Blood sampling for general analysis.
- Performing a bone marrow puncture.
- Collecting anamnesis and studying the condition of the digestive system organs, including the liver, spleen, etc.
It is imperative to exclude the fact that the patient has a parasitic infestation.
How to treat?
Treatment should be based on the causes that led to the development of anemia. It may be necessary to take antiparasitic drugs, eliminate polyps or other neoplasms of the digestive system, treat intestinal diseases, place the patient in a drug treatment clinic if he suffers from alcohol addiction, etc.
It is imperative to adjust the patient’s diet. It is necessary to include meat, liver, fermented milk products, fresh vegetables and fruits in its menu.
To eliminate vitamin B12 deficiency, intramuscular or intravenous administration of cyanocobalamin is possible. From 200 to 1000 mcg of the drug can be prescribed per day, depending on the severity of anemia.
After the blood counts return to normal, the dosage of the drug can be reduced, or the frequency of injections can be reduced. That is, the drug is administered once every 2 days, and then 2 times every 7 days.
Improvement occurs within a week from the start of treatment, which is characterized by the development of reticulocyte crisis. The level of young red blood cells in the blood increases by 2-3%. The effectiveness of the therapy is indicated by normalization of blood counts.
Sometimes vitamin B12 is prescribed for the rest of your life, for example, for Addison-Biermer anemia. With funicular myelosis, it is necessary to administer 800 to 100 mg of cyanocobalamin to the patient daily. It will be possible to reduce the dosage of the drug only after the patient has been completely relieved of neurological symptoms.
Sometimes megaloblastic anemia is very severe, and the patient himself may fall into a coma. In this case, he requires a transfusion of red blood cells.
When autoimmune diseases are the main reason for the development of anemia, the patient requires the administration of glucocorticosteroids. The dosage of the drug should be minimal and the course of treatment short.
For folate deficiency anemia, folic acid is prescribed. The daily dose is from 1 to 5 mg of the drug, depending on the severity of the disease. After all the symptoms of anemia have been relieved, a course of folic acid will be required to prevent recurrence of the disease. But the dose of the drug should be reduced.
Prevention and prognosis
To prevent the development of anemia, the following recommendations must be followed:
- Eat right by eating foods rich in vitamins B9 and B12.
- Lead a healthy lifestyle, give up alcoholism.
- Avoid situations that could lead to parasite infection.
- Treat all diseases of the digestive system in a timely manner.
As for the prognosis, with timely treatment it is favorable and it is possible to completely get rid of anemia.
Treatment of other diseases starting with the letter - m
| Treatment of malaria |
| Treatment of manic-depressive syndrome |
| Treatment of Marseilles fever |
| Treatment of mastitis |
| Treatment of mastopathy |
| Treatment of meningococcal infection |
| Migraine treatment |
| Treatment of multiple myeloma |
| Treatment of skeletal myeloma |
| Treatment of mycosis of the lungs |
| Treatment of mycoplasmosis |
| Treatment of myocarditis |
| Treatment of thrush |
| Treatment of urolithiasis |
The information is for educational purposes only. Do not self-medicate; For all questions regarding the definition of the disease and methods of its treatment, consult your doctor. EUROLAB is not responsible for the consequences caused by the use of information posted on the portal.
Which doctor treats megaloblastic anemia?
When the first signs of anemia appear, you should contact your local physician. If the doctor detects such a violation, he will redirect the patient to a hematologist who will prescribe treatment. Consultation with specialized specialists is possible, including: neurologist, infectious disease specialist, hepatologist, gastroenterologist. To select an adequate diet, you should visit a nutritionist.
Author of the article:
Shutov Maxim Evgenievich |
Hematologist Education: Graduated from Kursk State Medical University in 2013 and received a diploma in General Medicine. After 2 years, he completed his residency in the specialty “Oncology”. In 2021, she completed postgraduate studies at the National Medical and Surgical Center named after N.I. Pirogov. Our authors