It has long been known that a person’s internal biological clock regulates sleep and the functioning of all body systems. They synchronize with the light-dark cycle and are regulated by a special protein that accumulates at night and is used up during the day. When the phase of biological rhythms shifts, a person becomes hostage to disruption of circadian rhythms. Experiences a constant need to get a dose of sleep during the day and sleeps poorly at night. This condition leads to difficulties in living at a normal pace of life, decreased concentration, and requires urgent treatment from a somnologist.
What is circadian rhythm
Almost every cell of the human body is involved in biological processes that repeat cyclically throughout the day. Under the influence of special proteins, there is a timely activation of the synthesis of hormones for falling asleep, and an increase in blood pressure for awakening. It has been proven that appetite and brain activity depend on circadian rhythms.
The intensity of biological processes is affected by the duration of daylight and darkness. Information about the change of day and night is processed by a special part of the brain, receiving a signal through the retina. Today it is known that not only external factors are responsible for biorhythms. There is a section of DNA in the body that controls the human biological clock.
The circadian system is individual - everyone has their own time of falling asleep and waking up. When the “genetic clock” fails, the body adapts to new conditions. As a result, disorders arise that cause sleep disturbances, deterioration of well-being and a high risk of developing diseases.
Reasons for increasing QI
They are relatively rarely pathological. More often, a deviation in the circadian index indicates that the body is highly trained.
The violation (relatively speaking) is inherent in professional athletes and representatives of physical labor. In this case, recovery is not required, but the patient must be monitored.
You never know how your heart will behave next. Fatal consequences as a result of decompensation of the condition are quite possible.
Also, the cause of increased CI is an increase in pressure in the pulmonary artery and the accompanying dysfunction of the organ, anatomical defects, the so-called cor pulmonale.
How does jet lag manifest itself?
The main symptom of circadian disorders is a person's inability to fall asleep or wake up at a certain time. Lack of sleep leads to:
- to inattention;
- increased daytime sleepiness;
- lack of clarity of thinking;
- difficulty performing usual activities during the day;
- irritability, aggression;
- chronic fatigue, depression.
Sleep disturbances are accompanied by attacks of nausea and general malaise. Failure of biological rhythms threatens deterioration of heart function and the appearance of metabolic disorders.
Very often, in order to stay awake or, conversely, fall asleep, patients uncontrollably use sleeping pills and alcohol. But this behavior only makes the situation worse. If such signs appear, there is no need to try to cope with the problem on your own; it is correct to contact a specialist at a sleep medicine clinic.
Treatment
Treatment of the underlying pathological process is carried out. The circadian index should not be specifically normalized. Yes, and there is no such possibility. Contractility needs to be increased.
Treatment is mainly conservative, with the use of medications to relieve symptoms and combat the etiological factor. Both problems are solved at once.
What drugs are prescribed:
- Antiarrhythmic. Amiodarone or Quinidine. To restore normal heart rate and intervals between contractions. Used in short courses, it is not used on an ongoing basis due to the significant danger and mass of side effects.
- Antihypertensive. As needed. ACE inhibitors, calcium antagonists, centrally acting agents, diuretics with a mild, potassium-sparing effect. The names are selected by the doctor. With illiterate therapy, rapid development of heart failure and death of the patient in the short term is possible.
- Beta blockers. They help lower blood pressure and stop tachycardia. Increased frequency also occurs, but less frequently. If the normal functioning of the heart is disrupted, such as bradycardia, they are never prescribed.
- Cardiac glycosides. If there are no symptoms of coronary insufficiency, ischemia of cardiac structures.
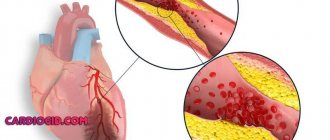
If necessary, statins are also indicated to dissolve cholesterol plaques and eliminate excess low-density lipids. Antiplatelet agents, special agents for normalizing the rheological properties of blood and preventing the formation of blood clots.
The operation is prescribed in extreme cases, strictly according to indications. These are considered to be heart defects. Congenital and acquired. Aortic, mitral, tricuspid valves, the vessels themselves, during the formation of aneurysms and other conditions.
Up to the destruction of chambers, for prosthetics or mechanical expansion of arteries (stenting, ballooning), creating bypass paths of blood flow (bypass surgery).
Radiofrequency ablation is possible for blockades of the conduction system (cauterization of an excessively active area).
The choice of the optimal direction of therapy is decided at the discretion of the doctor. The patient is instructed to limit himself for the rest of his life. But these are reasonable limits that will not cause much discomfort.
Quit smoking, alcohol, no drugs, no anti-inflammatory drugs without a doctor’s prescription, less fatty and fried foods in the diet. Get adequate sleep and at least minimal physical activity.
This is quite enough. Not a high price to pay for health, and possibly life.
Types of violations
There are several types of disorders:
| Variety | Peculiarities |
| Jet lag syndrome | Appears when fast moving across 2 or more time zones. According to the observations of somnologists, a person’s transfer to an earlier time is worse tolerated than a few hours ahead. |
| Distress related to changes in work schedule | A forced change in daily routine leads to disruption of the circadian rhythm. |
| Sleep phase delay syndrome | With this disorder, patients regularly fall asleep and wake up at late hours, and a steady shift in sleep phase is observed. |
| Phase advance sleep | This is the name of the condition when the biological clock is “in a hurry.” A person goes to bed early and gets up early, but he cannot change his wakefulness on his own. |
| Non-circadian sleep-wake cycle mode | Characterized by a daily change in the cycle by 1-2 hours, it is observed in blind people. |
Norms and calculation formula
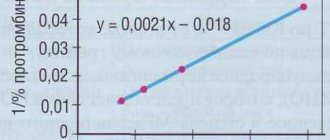
The formula for obtaining the circadian index in adults is calculated simply: you need to take the average heart rate in the period from 6 to 22 hours and divide it by the heart rate level in the period from 22 to 6.00. The resulting number will be the desired one.
The circadian index norm is determined in the form of a decimal coefficient. An adequate value is in the range from 1.2 to 1.4, plus or minus 0.3.
- The growth of the conditional level is considered not such a dangerous indicator. Occurs in athletes and people of physical labor. Less often for pathogenic reasons.
- A decrease in numbers is the result of pathology of the cardiovascular system. The rate of fall directly correlates with the likelihood of death. It is considered an important prognostic point.
It is possible to carry out repeated daily monitoring and, accordingly, calculate the circadian index. The frequency of changes depends on the likely pathological process.
The classic scheme is a study before the start of treatment, during, approximately a week after the start of therapy, and after the course. This will allow you to see the picture in dynamics and evaluate the effectiveness of the measures.
The norm as a percentage is rarely calculated, because the level is difficult to perceive and is not widely used in medical practice. Standard values are from 120 to 140%, perhaps a little higher, but not lower.
Causes of Circadian Rhythm Disorder
A shift in the rhythm of the biological clock in relation to the light-dark cycle is provoked by internal and external factors. The latter include:
- moving across several time zones (air travel from West to East);
- permanent work with irregular work schedule;
- lack of a routine when a person falls asleep and wakes up at different times;
- long bed rest;
- total visual impairment;
- taking medications.
Sleep disorders are often observed in hospitalized patients with frequent periods of wakefulness at night.
Pathological causes of failure of the circadian system:
- brain damage after injury, stroke;
- Alzheimer's disease, Parkinson's disease;
- encephalitis, meningitis;
- mutation of the circadian clock gene CRY 1;
- age-related changes.
Hereditary predisposition plays a major role when a person’s individual “genetic clock” is “fast” or “lagging behind.”
results
Power consumption
Assessment of food intake showed changes in the circadian rhythm in patients with SSP compared to the control group, which confirmed the validity of the selected criteria. The circadian rhythm of total energy consumption showed a phase delay of 1.5 hours (t28 = 2.86, p = 0.008) and this was accompanied in patients with SSP by a 31.4% decrease in amplitude (t28 = −2.76, p = 0.01). Circadian rhythm of carbohydrate (phase: t28 = 2.49, p = 0.019; amplitude: t28 = −2.13, p = 0.042) and fat (phase: t28 = 2.19, p = 0.037; amplitude: t28 = −2.47, p = 0.02) consumption also showed a comparable and significant circadian phase delay as well as a decrease in amplitude in patients with SSP. Despite the similarity of differences in protein consumption rhythm, it failed to achieve significant differences (phase: t28 = 1.13, p = 0.27; amplitude: t28 = −1.44, p = 0.16).
Neuroendocrine analysis
Neuroendocrine measures, such as food intake, also showed significant differences in amplitude and phase between patients with SSP and controls. The delay in melatonin rhythms in patients with SSP is 1.1 hours (t25 = 2.17; p = 0.04), but the differences in amplitude are not significant (t25 = −1.10, p = 0.28).
The phase delay of the TSH rhythm in patients with SNP averaged 0.7 hours, but the differences did not reach statistically significant values (t26 = 1.46, p = 0.16), despite significant increases in amplitude (30.9%; t26 = 2.07, p = 0.049 ). There were no significant phase differences in prolactin rhythms during SNP (t28 = 0.48, p = 0.63), and the decrease in amplitude was also insignificant (t28 = −1.95, p = 0.06). The phase delay of cortisol rhythms at 0.7 hours in patients with SSP did not reach significant differences (t28 = 1.76, p = 0.089), despite a 25.7% decrease in rhythm amplitude (t28 = −3.34, p = 0.002).
Noticeable differences were found between groups in hormones involved in appetite regulation. Circadian fluctuations of ghrelin, a stimulant predominantly produced by the stomach/orexigenic peptide, are accelerated by 5.2 hours in patients with SSP (t26 = −4.15, p < 0.001) and by almost half in amplitude (50.4% amplitude compared with controls; t26 = − 2.45, p = 0.021). In contrast, the circadian rhythm of leptin, an appetite-suppressing fat cell-derived/anorexic hormone that is associated with long-term current energy availability status, showed a 1.0-hour phase delay in patients with SSP (t28 = 2.13, p = 0.042), but no difference in amplitude (t28 = −0.38, p = 0.70), despite elevated levels at all control time points in patients with SSP. Compared to controls, the circadian rhythms of glucose in patients with SNHL are inverted (accelerated by 11.6 hours or delayed by 12.4 hours; t28 = 2.04, p < 0.001), but there is no significant difference in amplitude (t28 = − 1.64, p = 0.11). Insulin circadian rhythms in patients with SSP are delayed in phase by 2.8 hours (t28 = 3.15, p = 0.004), and are almost half smaller in amplitude (42.3% of control amplitude; t28 = −4.57, p < 0.001).
Absolute values for patients with SSP and controls (mean ± SD), as well as differences in amplitude and phase in patients with SSP compared to controls in energy intake, 7 hormones and glucose.
| Index | SNP | Control | Differences in amplitude in SNP (%) | Phase differences during SNP (hours)a |
| Calories in general | 2959 ± 154 | 2765 ± 206 | — 31,4** | — 1,5** |
| Carbohydrates (g) | 370,9 ± 26,9 | 378,8 ± 29,7 | — 33,9* | — 1,9* |
| Fat (g) | 118,0 ± 11,3 | 110,9 ± 14,0 | — 34,4* | — 1,5* |
| Proteins (g) | 113,5 ± 8,3 | 128,5 ± 13,0 | — 16,8 | — 0,5 |
| Melatonin (pg/ml) | 24,3 ± 3,4 | 21,7 ± 3,8 | — 15,3 | — 1,1* |
| TSH (µU/l) | 2,3 ± 0,1 | 1,5 ± 0,1 | 30,9* | — 0,7 |
| Prolactin (ng/ml) | 17,9 ± 0,7 | 16,3 ± 0,9 | — 28,6 | — 0,3 |
| Cortisol (mg/dl) | 8,6 ± 1,1 | 9,8 ± 1,3 | — 25,7** | — 0,7 |
| Ghrelin (pg/ml) | 248 ± 6,4 | 268 ± 5,5 | — 49,6* | 5,2** |
| Leptin (ng/ml) | 40,1 ± 0,9 | 33,2 ± 0,9 | — 3,9 | — 1,0* |
| Glucose (mg/dl) | 109,3 ± 1,4 | 109,7 ± 2,4 | — 56,5 | 11.6/- 12.4s |
| Insulin (ng/ml) | 1,8 ± 0,1 | 1,7 ± 0,2 | — 57,7** | — 2,8** |
The mean and error of the mean were calculated over the entire 25-hour sample collection period. Using a linear mixed effects model and testing fixed effects across groups, there were no significant differences in hormones or glucose, and no significant differences in total energy intake after a two-tailed t test (Allison et al, 2005). NES – night binge eating syndrome; TSH is thyroid stimulating hormone.
a – negative values indicate a phase delay
* — p < 0.05 using a two-tailed t-test.
** — p ≤ 0.01 using a two-sided t-test.
How are circadian disorders treated?
Our center’s somnologists have extensive experience in correcting circadian rhythms, including managing non-standard cases of the disease. The list of therapeutic measures in most cases is individual.
Basic therapy includes:
- Phototherapy with sunlight. This is not always associated with exposure to the sun; fluorescent lamps are also used to correct the circadian system. When you need to stay awake, experts recommend being in bright light. Before falling asleep, carefully darken the room, curtain the windows with thick curtains, and put on glasses with dark lenses before going to bed.
- Regularly performing a set of simple physical exercises helps set your internal biological clock.
- The synchronization of biorhythms with the daily period is affected by food intake. Therefore, it is important to establish a proper diet. Most of the diet is recommended to be consumed in the morning and afternoon. In the evening, the serving size is reduced.
- If, after changes in behavior, symptoms of circadian rhythm disorder persist, the somnologist prescribes drug therapy. The effective dosage, frequency and duration of use of the drug is determined by the doctor, taking into account concomitant diseases.
During the elimination of circadian disorders, patients at the South Clinic are under the close supervision of a competent specialist who promptly assesses changes and, if necessary, adjusts prescriptions.
Diagnostics
It is carried out on an outpatient basis. Hospitalization is required only in critical cases. Specialist - cardiologist.
Approximate list of events:
- Oral questioning of the patient regarding complaints. Objectification of symptoms allows you to build a clear clinical picture and put forward approximate hypotheses regarding the possible disruption of the heart.
- Anamnesis collection. Previous illnesses, habits and lifestyle, family history, other points.
- Measuring blood pressure using routine methods. Using a regular tonometer. Used for immediate assessment of vital signs.
- The basis of diagnosis is daily Holter monitoring. Only it can provide accurate information on the circadian rhythm. The measurement is carried out every half hour or hour and is entered into the memory of an automatic programmable device. Then the device independently calculates the indicator and remembers it.
- Then doctors have more opportunities for diagnosis, the vector becomes clear. Because the numbers usually depend on the probable pathological process.
- The following shows electrocardiography. It is necessary to detect rhythm disturbances. For example, extrasystoles and other similar deviations.
- Echocardiography. Ultrasound research technique. It is used for early detection of anatomical defects or determining the stage of the disorder.
- MRI if necessary.
- Load tests. If there is no reason to suspect anatomical defects, heart failure or other dangerous conditions. It is carried out under the supervision of doctors in order to provide first aid if necessary.
Other specialists may be involved. They are not able to eliminate the cause of the disorders, but identifying abnormalities in the nervous system and respiratory activity is their prerogative.
Causes of cardiac arrhythmia
The causes of arrhythmia (the occurrence of heart rhythm disturbances) are so diverse that listing absolutely everything is a very difficult task. However, in many cases, the safety of the arrhythmia for the patient’s life and further treatment tactics depend on the cause of the arrhythmia.
Many different classifications of the causes of arrhythmia have been proposed, but none of them is currently generally accepted. We consider the following classification to be the most acceptable for the patient. It is based on the presence or absence of primary heart disease in the patient. If there is heart disease, the arrhythmia is called organic, and if there is no heart disease, it is called inorganic. Inorganic arrhythmias are also commonly called functional.
Do cardiac arrhythmias manifest themselves in the same way?
All rhythm and conduction disorders clinically manifest themselves differently in different patients. Some patients do not feel any symptoms and learn about the pathology only after a scheduled ECG. This proportion of patients is insignificant, since in most cases patients note obvious symptoms.
Thus, rhythm disturbances accompanied by rapid heartbeat (from 100 to 200 beats per minute), especially paroxysmal forms, are characterized by a sharp sudden onset and interruptions in the heart, lack of air, pain in the sternum.
Some conduction disorders, such as fascicular blocks, do not show any signs and are recognized only on an ECG. Sinoatrial and atrioventricular blockades of the first degree occur with a slight decrease in heart rate (50-55 per minute), which is why clinically they can manifest only slight weakness and increased fatigue.
Blockades of the 2nd and 3rd degrees are manifested by severe bradycardia (less than 30-40 per minute) and are characterized by short-term attacks of loss of consciousness.
In addition, any of the listed conditions may be accompanied by a general severe condition with cold sweat, intense pain in the left half of the chest, decreased blood pressure, general weakness and loss of consciousness. These symptoms are caused by impaired cardiac hemodynamics and require close attention from a doctor.
How to make a diagnosis?
Classification
All rhythm and conduction disorders are classified as follows:
- Heart rhythm disturbances.
- Conduction disorders in the heart.
In the first case, as a rule, there is an acceleration of the heart rate and/or irregular contraction of the heart muscle. In the second, the presence of blockades of varying degrees with or without slowing of the rhythm is noted.
In general, the first group includes disorders of the formation and conduction of impulses:
- In the sinus node, manifested by sinus tachycardia, sinus bradycardia and sinus arrhythmia - tachyarrhythmia or bradyarrhythmia.
- According to the tissue of the atria, manifested by atrial extrasystole and paroxysmal atrial tachycardia.
- At the atrioventricular junction (AV node), manifested by atrioventricular extrasystole and paroxysmal tachycardia.
- Along the fibers of the ventricles of the heart, manifested by ventricular extrasystole and paroxysmal ventricular tachycardia.
- In the sinus node and along the tissue of the atria or ventricles, manifested by flutter and fibrillation (fibrillation) of the atria and ventricles.
The second group of conduction disorders includes blockades in the path of impulses, manifested by sinoatrial block, intraatrial block, atrioventricular block of 1, 2 and 3 degrees and bundle branch block.