Treatment under the compulsory medical insurance policy is possible!
Submit your application
Follow the news, subscribe to our social networks
Details
A pacemaker (pacemaker) is a small device, weighing approximately 30-50 grams, capable of creating electrical impulses that regulate heart rate. It is installed when it is necessary to maintain rhythm in patients with bradycardia or atrioventricular block, when the heart works intermittently.
A pacemaker, as a rule, consists of two parts: a metal case containing a battery designed for 7-10 years of operation and a microprocessor unit that provides heart rate setting and other parameters; the second part is the electrodes, through which electrical impulses propagate from the pacemaker into the chambers of the heart. Pacemakers are the best treatment for bradyarrhythmias. The first pacemaker was implanted in 1958.
There are three types of pacemaker (this depends on the location of the electrodes):
- Single-chamber: installed in only one chamber of the heart - the right ventricle or atrium,
- Two-chamber: installed in the atrium and ventricle of the heart,
- Three-chamber: contains a device for the treatment of heart failure, installed on the right atrium and both ventricles.
ECS is also divided into temporary (an external stimulator is installed for a period of several hours to 2 weeks) and permanent (an implanted stimulator is installed).
How is the treatment carried out?
- The pacemaker is installed under local anesthesia and under X-ray control in a specially equipped operating room.
- Electrodes connected to a stimulator, which is sewn into the muscle bed in the subclavian region, are inserted into the heart through the subclavian vein.
- The most difficult part of the procedure is positioning and securing the lead tip into the atrium or ventricle to ensure good contact.
- A bed for a pacemaker is created in the subclavian region on the left or right under the skin through a small skin incision.
Don't lose your rhythm: how the heart's electrical system works
Before you understand what a pacemaker is and how it works, you need to remember the anatomy and physiology of an organ such as the heart. The heart has its own internal electrical system that controls the speed and rhythm of its work. With each heartbeat, an electrical signal travels from the upper chambers of the heart (atria) to the two lower chambers of the heart (ventricles). The ventricles then contract and pump blood to the rest of the body. The combined contraction of the atria and ventricles is the heartbeat.
Each electrical signal usually begins in a group of cells called the sinus node. With age or the presence of cardiovascular disease, the sinus node loses its ability to set the correct pace for the heart rhythm.
Problems with the speed or rhythm of the heartbeat are called arrhythmias. During an arrhythmia, the heart may beat too fast (tachycardia), too slow (bradycardia), or with an irregular rhythm. The electrical signal may be completely interrupted as it travels through the heart. Today, such heart rhythm disturbances occupy one of the leading places in the structure of cardiovascular diseases and are the annual cause of death for 200 thousand people in Russia.
Such faulty electrical signaling in the heart can be dealt with by a pacemaker. Using electrical impulses, it prevents arrhythmias and causes the heart to beat at the correct rhythm. To understand how a pacemaker copes with such a difficult task, let’s first consider what this miniature but complex electronic device is.
Possible complications
The risks of the procedure are generally around 1%, including bleeding, pneumothorax (air entering the pleural space), cardiac perforation, risk of suppuration and device malfunction.
Possible complications include displacement and disruption of electrode insulation, pacemaker syndrome (dizziness and shortness of breath when the pacemaker is not working properly) and infectious complications.
In fact, such complications are very rare and are not comparable to the benefits of a pacemaker installed according to indications.
Installation of a pacemaker for arrhythmia
Questions and answers
Possibly gongrene I injured my hand, the skin was torn off while drinking on gravel and my hand became rusty in two hours, what should I do?
Answer:
See a surgeon for an appointment.
Hypoplasia of the left vertebral artery
Hello. I have been sick for a long time. Nausea. vomiting. Impaired coordination. unsteadiness. Severe headaches. What examination should I do before someone turns to you for help?
Answer:
Do MSCT of the arteries of the neck and brain with contrast.
Thromboangiitis obliterans
Hello. My mother is 58 years old, disabled group 1. She had both legs amputated below the knees due to thromboangiitis obliterans. We underwent an ultrasound examination of the NK vessels. What additional research needs to be done...
Answer:
What about the stumps now?
Leg amputated
Hello! My brother had his leg amputated in December 2021 due to atherosclerosis, after which he developed gangrene. In January we underwent re-amputation. It is now March, but the wound is not healing. They did a CT scan of the vessels...
Answer:
What to do?
Restore blood flow. Send a link to MSCT of vessels. Gangrene
Hello, my dad had gangrene on his right leg on the big toe, his toe was amputated, the treatment prescribed by the doctor did not help, there was pain, a large crust and there was pus, they applied ointments...
Answer:
It is urgent to perform an ultrasound of the arteries of the extremities and MS CT with contraception; after receiving the examination results, we will be able to offer you the optimal treatment method.
How to treat trophic ulcers and necrosis of the fingers.
Hello. After examination at the Donetsk Institute of Emergency and Reconstructive Surgery named after. In K. Gusak (DPR), my husband was diagnosed with ischemic heart disease: atherosclerotic cardiosclerosis. CH2a. GB 2st. risk 3. Left ventricular thrombus. ...
Answer:
Good afternoon.
The left leg suffers from ischemia, i.e. lack of blood flow. To prevent it from bothering you, you need to restore blood flow. Need surgery. Perform CT angiography of the abdominal aorta and arteries of the lower extremities (to the feet)…. Red spots.
Hello, I broke my leg in September, but after 4 months, red spots in the form of bruises appeared on my leg, and they just don’t go away. WHAT COULD BE?
Answer:
Good afternoon.
Without examination it is not possible to make a diagnosis. See a traumatologist. Wet gangrene
Hello! My dad (70 years old) has wet gangrene of the leg, we live together in the same apartment with a small child (2 years old), is this situation dangerous for the baby? Thank you!
Answer:
Good afternoon.
Gangrene is dangerous if it is accompanied by an infection. Show the patient to the surgeon. Atherosclerosis of the lower extremities.
Hello, my dad is sick, he is 81 years old. atherosclerosis, calcification of blood vessels of the lower extremities. In Perm, doctors did everything they could (including angioplasty, which did not bring results). For now…
Answer:
Most likely it is possible, but you need to see the patient in person.
You cannot establish a forecast by correspondence. Occlusion of the upper limb.
My mother is 68 years old. Since August 2021, for the first time, very severe pain appeared in the elbow on the right. Gradually, the pain intensified and spread lower throughout the arm; conservative treatment had no effect. Consulted by a neurosurgeon from the Federal Center of Neurology of...
Answer:
Perform CT angiography of the arteries of the upper extremities. Send a link to the study by mail
Heart friend weighing 20 grams: device and principle of operation of a pacemaker
A pacemaker essentially consists of three parts: an electrical pulse generator, a battery, and a series of wires with electrodes on their tips. The battery powers the generator, and both are surrounded by a thin metal casing that is connected to the heart by wires.
All parts of the ECS have evolved significantly over time. For example, the electrical pulse generator currently consists of a programmable microprocessor. While the first pacemakers continuously generated an electrical impulse at a rate of 70 beats per minute, pacemakers are now able to monitor the electrical impulses of the atria and ventricles, as well as a number of other parameters such as breathing rate and body movement. Therefore, they can intervene in the regulation of heart rhythm only when necessary, for example, when a person plays sports or is nervous, that is, behave just like a healthy heart.
Modern lithium-ion batteries have not only extended the service life of the pacemaker to approximately 15 years, but have also made it possible to significantly reduce its dimensions. Now the generator and battery are placed in a titanium box measuring 5x4.5x1 cm, weighing only 20 grams. Wires extend from this box, which through a vein or artery reach the desired area of the heart to stimulate contractions. There can be from one to three such wires; the type of pacemaker depends on their number: one-, two-, or three-chamber.
A single-chamber pacemaker has one such wire that connects it to one chamber of the heart: this can be the right atrium or the right ventricle. A two-chamber pacemaker is connected to two cavities of the heart, and a three-chamber pacemaker, accordingly, has three wires. Such a pacemaker can stimulate both the right atrium and both ventricular cavities. The pacemaker is selected and programmed individually for each patient, taking into account the rhythm of his heart.
A pacemaker is implanted into a person's body (usually under the subcutaneous fat of the chest) and connected to the heart muscle using electrodes. A pacemaker acts on the heart muscle in the absence of a natural heart rhythm, that is, it produces an electrical impulse. As a result of this impulse, the heart muscle contracts. Nowadays, pacemaker implantation is considered a simple operation that is performed under local anesthesia. But once upon a time, this was a serious, life-threatening surgical intervention.
Positive effects of a pacemaker
Implantation of a pacemaker abroad is primarily aimed at normalizing and stabilizing the heart rhythm. This effect is achieved by electrical stimulation of the heart muscle.
In addition, modern models of pacemakers have the function of storing information about the functioning of the heart. Subsequently, a cardiologist can read this data and analyze cardiac activity. Based on such a study, the patient will be offered adequate drug treatment for arrhythmia. In this case, consultation with a specialist is included in the total price of treatment.
Stages of the operation
The operation to install the device lasts up to 2–3 hours. The duration of installation of a single-chamber device is 30 minutes, a two-chamber device is 1.5 hours, and a three-chamber device is up to 2.5 hours.
The intervention occurs in stages:
- The surgical field is prepared for anesthesia. The drugs are administered subcutaneously and intramuscularly.
- Electrodes are inserted into various parts of the heart. The surgeon makes an incision in the collarbone area and then places the electrode in the desired chamber. To accurately perform manipulations, the surgeon needs to take x-rays of the surgical field.
- The electrodes are connected to the body of the pacemaker, which is implanted under the pectoral muscle.
- The device is programmed according to the individual needs of the patient. The doctor sets the baseline heart rate at rest and during exercise. After this, the edges of the wound are sutured.
Modern devices are miniature, so they are invisible on the human body.
Who can check and adjust a pacemaker?
A cardiologist, arrhythmologist or cardiovascular surgeon can check and adjust the pacemaker. The main thing is that the doctor has the appropriate qualifications and knows how to do it correctly. You will definitely need a programmer that is suitable for your pacemaker: each manufacturer produces its own models that are incompatible with others.
The arrhythmologist at City Clinical Hospital No. 31 has extensive experience working with pacemakers of various models. All you need to do is name your device model when making an appointment.
Rehabilitation of patients with a pacemaker
The patient’s recovery after implantation occurs in two periods:
- Hospital stage. Immediately after the surgical procedure, the patient is transferred to the recovery room, where he must adhere to bed rest for several days. During this time, doctors monitor basic cardiac functions. The cost of treatment depends on the length of hospital stay.
- Home rehabilitation. The price of a specialist consultation during this period is included in the complex of cardiac medical care. At home, the patient should refrain from physical activity and water procedures for some time.
A patient with an installed pacemaker is prohibited from
- Stay in the area exposed to powerful electromagnetic fields, perform MRI.
- Be exposed to electric current.
- Use some physical therapy treatments.
- Strike the area where the pacemaker is implanted.
Preparing for surgery
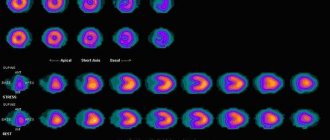
Before installing the pacemaker, the patient undergoes a full examination.
It includes:
- general and biochemical blood tests;
- determination of blood group and Rh factor;
- coagulogram;
- analysis for infections;
- general urine analysis;
- ECG;
- chest x-ray;
- EchoCG;
- Ultrasound of internal organs.
Examinations such as Doppler sonography of the arteries and veins of the lower extremities, coronography, etc. can also be carried out. If necessary, the patient is sent for consultations with specialized specialists: endocrinologist, neurologist, etc. We have all the capabilities to perform diagnostics within one day.
Immediately before surgery, the patient should:
- Eliminate alcohol intake (for a week).
- Stop taking certain medications.
- Do a cleansing enema (on the eve of the operation).
- Refuse food and water (6-10 hours before).
- Take a shower (in the morning of the day of surgery) and, if necessary, shave the hair in the chest area.
The patient is also consulted by a surgeon and an anesthesiologist before the intervention.
Why is it necessary to check the operation of a pacemaker?
An pacemaker implanted in a patient is not only a medical device, but also a foreign body implanted into the patient’s body, and the patient’s quality of life, and sometimes life itself, depends on the correctness of its operation. Therefore, it is important to regularly check and adjust the artificial pacemaker. Monitoring a patient with a pacemaker is not just a check of the device, but an objective assessment of the operation of the entire stimulating system, consisting of three important components: • the patient’s heart, • the electrodes, • the pacemaker itself.
Benefits of installing a pacemaker
The undoubted advantage of implanting a pacemaker in patients with chronic heart failure is saving the patient’s life. Patients with this pathology during drug therapy have a high risk of death. Also, compared to conservative treatment, installation of a pacemaker causes rapid recovery of cardiac activity. All these advantages are observed at a low cost of the operation itself. The price of the device and its fixation is several times cheaper than complex surgical intervention.
The cost of pacemaker implantation in Germany is determined by the model of the generator, the qualifications of the surgeon and the level of the cardiology clinic. The Deutsche Medizinische Union team will select a medical center for the patient, where he will have a high-tech and uninterrupted pacemaker installed. We will also advise you to contact the best German cardiologists to select the optimal model of pulse generator. During the rehabilitation period, DMU specialists will organize a visit to a cardiac surgeon to analyze the functioning of the heart and correct the function of the device.
Pacemakers Boston Scientific
Boston Scientific is an American manufacturer of pacemakers, cardioverter-defibrillators and other medical products. Its main office is located in Boston (USA), production is in Manhattan and Ireland. The company produces different models of pacemakers, the most popular in Russia are Contak Renewal TR2 and Altrua 50. Main features of the brand's products: • Mainly single- and double-chamber models are presented. But there are also three-chamber ones (for example, Contak Renewal TR2). • Boston Scientific pacemakers are small in size and weight (21-27 g). There are miniature devices that can be safely installed in people with narrow chests. • All models have a built-in sensor that monitors battery charge. Checks are carried out every 11 hours. • Some models are equipped with sensors that respond to the patient's condition. • The accelerometer automatically increases your heart rate during exercise. • The minute ventilation sensor adjusts the operation of the device to your emotional state.
How to live after the intervention?
The low-invasiveness of the procedure allows the patient to be discharged from the hospital within 3-5 days. The time spent in the hospital is necessary to set up optimal operation of the pacemaker, prevent postoperative complications, and select adequate therapy for the patient’s heart disease (dose reduction or complete withdrawal of the drug).
During the first 4-6 weeks, the patient may feel a slight tingling sensation at the site where the device was implanted. These are microdischarges that excite tissue. Often, tingling and discomfort disappear on their own; sometimes reprogramming the device is required. The rehabilitation period lasts 7-14 days. A prophylactic dose of antiarrhythmic drugs is prescribed for 7-10 days. Patients at this stage should avoid heavy emotional stress and physical labor.
After two weeks, the person returns to his previous life activities and can start working, and young women can become pregnant and give birth to a child.
There are several prohibitions in professional activities:
- working with heavy vibrating tools;
- with high-frequency heating devices;
- with electrocarbon welding devices, induction furnaces;
- with electrical appliances with a strong magnetic field or high voltage lines;
- with an electric welding machine;
- on radio and television towers.
After discharge from the hospital, you must strictly follow several rules:
- take medications prescribed by a cardiologist;
- adhere to a schedule of visits to check the operation of the pacemaker;
- Always carry with you a patient card with an implanted pacemaker.
After three, six months, and then every year, the patient must undergo a follow-up examination with a doctor and check the condition of the pacemaker using a special device that programs the operation of the device. Checking the ECS consists of:
- analysis of electrode position;
- assessing the optimality of the program;
- checking the battery charge, predicting the date of replacement of the power source;
- eliminating complications that have arisen, educating the patient.
As the pacemaker's power supply gets closer to being replaced, the frequency of visits to the doctor will increase.
There are several considerations for patients with ICD:
- driving with extreme caution;
- It is not recommended to wear a mobile phone over an implanted mechanism;
- do not linger between security gates in shops and airports;
- MRI examinations and medical procedures using certain instruments (electrocautery, diathermy, external defibrillator, ultrasound lithotripsy, radiofrequency ablation, radiation therapy) are prohibited.
Patient Prognosis
Installation of an artificial pacemaker can prolong a patient’s life for decades and significantly improve its quality.
Disability for a patient with ECS can only be established if his complete dependence on the device is proven. For this purpose, it is necessary to conduct a forensic medical and social examination (MSE), during which the patient’s health condition and the degree of circulatory failure will be assessed. Also, to prove dependence on the pacemaker, you need to temporarily turn off the device recording the electrocardiogram. If there is asystole lasting more than 5 seconds (or for 2 seconds followed by a rhythm of less than 30 beats/min), the person is considered completely dependent on the device. If the heart rate is > 40 beats/min. assignment of a disability group will be denied.
Pacemaker and long journeys
There are no travel restrictions for people with ECS. After three months, patients can easily fly on an airplane with a pacemaker. For safe travel, you must adhere to a number of rules:
- Plan a trip 3 months after pacemaker implantation.
- Be trained in the rules of behavior in the event of a device breakdown.
- Indicate to the tour operator the presence of an artificial pacemaker and arrange insurance.
- Take your ECS patient card with you (at the airport it allows you to pass a manual search instead of a magnetic frame).
- Do not stay inside the metal detector for more than 15 seconds.
- Find several nearby medical facilities that can provide assistance in an emergency.
People with an artificial pacemaker can drive without interference. The only precaution is that if you need to travel for a long time behind the wheel, it is recommended to wrap the seat belt straps with a towel to reduce the load on the site where the pacemaker is implanted.
Sex, bathhouse and other entertainment after implantation: when and to whom is it possible?
Patients with installed pacemaker have no restrictions on diet and alcohol consumption. But you should follow nutritional recommendations for cardiac pathology and drink alcohol in moderation. Two weeks after implantation of the pacemaker, if the patient feels well, the patient can return to sexual activity.
Patients with ECS can play sports with the exception of:
- contact sports (football, martial arts);
- scuba diving, scuba diving;
- sport shooting (recoil from the buttstock can damage the contacts or the body of the device).
Doctors' recommendations differ regarding relaxation in the sauna. Some categorically prohibit visiting the steam room, others are of the opinion that a short stay in the bathhouse is possible after three months from the time of the operation. In any case, it is necessary to build on the condition of the individual patient.
Postoperative wound and monitoring it
After inserting the sensors into the formed bed, a heart pacemaker is installed in the projection of the pectoralis major muscle. The operation ends with the application of several stitches to the skin.
Living with a pacemaker imposes certain restrictions on the patient, which, although not serious, are important for the correct and long-term operation of the device.
The most critical period is the first 7 days after surgery. This concerns primarily the condition of the postoperative wound.
For the first 5-7 days, the patient is in the hospital to monitor the operation of the electrical stimulator. Every day the wound is dressed and cleaned.
The stitches are removed on the 6th - 7th day. After removal of the sutures, the patient must limit the load on the upper limb from the placement of the implanted device for another 7 days.
Such events are carried out with the aim of creating a mature scar that can withstand the usual work.
Is it possible to check it yourself at home?
In order to fully check the operation of the pacemaker, the following equipment is required:
- ECG device;
- programmer;
- impulse duration meter (for domestic ECS);
- stimulus frequency analyzer;
- special magnet;
- external pacemaker.
Such a diagnostic complex is often absent not only in the clinic, but also in medical institutions that do not specialize in working with pacemakers. For home use, a device such as a heart rate monitoring bracelet, which is used when playing sports, may be recommended.
Fitness bracelet
Fitness bracelets help to estimate the frequency of contractions throughout the day , although they have a measurement defect - an error if worn incorrectly. If they show a daily decrease in heart rate, then this is a reason to visit a doctor.
Indications and age-related contraindications: who needs the device and why?
Absolute include :
- sustained bradycardia with characteristic clinical signs;
- documented decrease in heart rate < 40 beats/min. during physical work;
- episodes of absence of rhythm (asystole) on the ECG lasting more than three seconds;
- combination of sustained AV block of II-III degree with delays in impulse conduction along two or three His bundles in patients with post-infarction cardiosclerosis;
- any types of bradyarrhythmias that may threaten the health or life of the patient (if the heart rate is less than 60 beats/min.);
- paroxysms of ventricular arrhythmias (tachycardia, fibrillation, asystole).
Relative readings:
- AV blockade of II-III degrees without changing the patient’s condition;
- loss of consciousness in patients with blockades without connection with ventricular tachycardia with an unknown cause of arrhythmia;
- severe circulatory failure with asynchronous ventricular function (with atrial fibrillation, myocardial infarction).
There are no age-related contraindications to installing a pacemaker. The only limitation is that the operation is not justified.
Rehabilitation after installation
After the operation, the patient usually remains in the hospital for one or two days. Immediately after the procedure, the patient should, if possible, not stand up for several hours. Typically, upon discharge, the patient will receive detailed information about how to care for the implanted pacemaker site. For proper wound healing during the first weeks, patients should not carry heavy objects or make sudden movements with their hands on the implantation side.
If the sutures are not absorbable, they must be removed by medical personnel within the time frame established by the attending physician. Before the patient is discharged from the hospital, the pacemaker is monitored and programmed based on the patient's needs. The first follow-up visit is determined, and the patient, along with a discharge from the hospital, receives a so-called implanted pacemaker passport, which indicates the type and name of the medical device and electrodes, as well as the parameters programmed in the device (you must always carry it with you).
As a rule, after surgery the patient quickly returns to a healthy lifestyle. In rare cases, symptoms such as fever, severe redness, swelling of the wound, abscess of the implantation site, fainting or dizziness, or persistent hiccups or unusual chest muscle spasms may occur. Then you should immediately contact the center where the patient had the operation to check if everything is fine.