Indications for testing
MSI in a blood test is a highly informative indicator, thanks to which it is possible to assess the current state of the body, confirm the diagnosis, conduct differential diagnostics and study the dynamics of prescribed therapy. Typically, this test is prescribed at the MedArt clinic for:
- Preventive and clinical observation, including for pregnant women.
- Baseline examination during patient hospitalization.
- Suspicion of anemia (of any type).
- Diseases of the hematopoietic system.
- Infectious and inflammatory processes.
- Evaluation of the effectiveness of the started treatment.
It is important to understand that the MCH is not an independent indicator. To evaluate it, a detailed blood test is prescribed, reflecting the most complete picture of the bloodstream at the moment.
Causes of increase and methods of treatment
An increase in the MCHC indicator indicates that red blood cells carry more hemoglobin than usual, and since this substance is also a pigment that gives the cells their rich hue, the color indicator also changes.
This happens in many cases.
Megaloblastic anemia
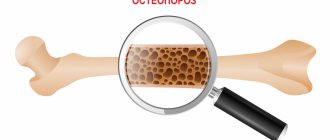
In other words, a disorder of hematopoiesis due to vitamin B12 deficiency. Less commonly involved is folic acid. If one or the other is insufficient, the maturation of shaped structures in the bone marrow is impossible, and mchc in the blood test will be increased. Vitamins are responsible for the normal development of red blood cells.
Insufficiently formed cells are significantly larger than normal ones. They carry a lot of hemoglobin, but due to their structural features they are not able to bind oxygen and carbon oxidation products.
When hematopoiesis completely switches to abnormal tracks, a paradoxical situation is observed. The cells carry huge amounts of pigment, but don't work as well as they should. An increase in hematocrit and MCHC is most often due to megaloblastic anemia.
Treatment: in the early stages it is much easier to cope with the problem. When the disease reaches an advanced phase, this is also possible, but the duration of therapy will be much longer.
The main way to correct the disorder is to restore the supply of vitamins. They are administered artificially, in large doses. The concentration is gradually reduced.
The problem may also be in the absorption of B12 or folic acid. For example, due to inflammatory pathologies of the small intestine or other disorders. In this case, you need to fight the primary disease. At the same time introducing vitamin-based medications. The specialized specialist is a hematologist.
Read more about megaloblastic anemia in this article.
Smoking
Tobacco consumption, especially in large quantities, “hits” the hematopoietic system. The problem is not nicotine, although it is certainly harmful.
The outer shell of a cigarette, the dye, contains many substances that, when burned, form dangerous poisons. For example, oxides of cadmium, arsenic, volatile carbon compounds (methane). This is only a small part.
All of them depress the hematopoietic system. Although formally the red blood cells remain normal in size, the hematocrit decreases. That is, the number of cells becomes smaller.
For this reason, gas exchange occurs much more slowly than usual. In order to somehow compensate for the current state of affairs, the body seeks to strengthen the functional capabilities of those cells that exist. The amount of hemoglobin per red blood cell increases.
This is not a one-time or rapid process. The longer a person smokes, the more noticeable the problem.
Treatment: the main thing to do is to quit the bad habit. Then, as needed, doctors prescribe a course of therapy and supportive techniques. But the main task is to quit smoking.
Alcohol consumption
Especially for a long time and in excessive quantities. Alcohol works in much the same way as cigarettes. Inhibits bone marrow function. Cells cannot mature and are released half-ready.
The effect is identical. Since these structures are larger in size than normal ones, more hemoglobin is placed in them. This does not change the situation, since they still cannot transfer gases due to their irregular structure, the thickness of the cell membrane and other factors.
Treatment: hematologists are involved in the treatment of organic disorders themselves. The goal is to eliminate alcohol from life and at the same time support and stimulate normal hematopoiesis.
Addiction specialists can help you quit your addiction. Solving both issues at once is not easy; it will take time. If a person has been drinking for a long time or suffers from alcoholism, full recovery takes from several months to six months or even more.
Some medicines
Medicines can also interfere with hematopoiesis. Three groups of drugs are especially dangerous in this regard:
- The first are hormonal or glucocorticoid-based drugs. They inhibit bone marrow function. Red blood cells do not mature in sufficient quantities. Many undeveloped forms emerge into the mainstream - large in size and with excess hemoglobin. A similar effect can develop immediately after starting treatment or later. It all depends on the characteristics of the individual patient’s body.
- The second are sedatives and tranquilizers. They provoke approximately the same result.
- Still others are psychotropics. Antidepressants and neuroleptics.
Treatment: no special therapy is needed. It is enough to give up the drugs and everything will return to normal on its own.
This is not always possible: for example, in schizophrenia and organic psychoses, antipsychotics are constantly needed. Or a patient with autoimmune inflammatory disorders needs courses of glucocorticoids.
Then the issue is resolved by simply replacing the medication. They choose something else.
Genetic pathologies
In the context of the situation under consideration, they are relatively rare. We are talking about disorders that are inherited. With “defective” material from parents.
A spontaneous mutation is possible. Genes have nothing to do with it, this is a sporadic episode. The degree of impairment depends on what material is altered.
Treatment. As such, there is no specific therapy. At the very least, it won’t be able to radically influence the situation. The violation is encoded in the foundation of the body; we have not yet learned how to edit the genome. Doctors resort to symptomatic treatment. The investigation is being corrected.
Excessive amount of fat in the body
In other words, hyperlipidemia. There are many forms of this condition. All of them are equally dangerous from the point of view of hematopoietic disorders.
Treatment. You need to reduce the amount of fat. For this purpose special preparations are used. Statins, for example, Atoris or similar. To quickly remove excess cholesterol or other lipids.
If they are ineffective, heavier drugs are used - fibrates. Nicotinic acid also performs well.
In general, specific medications are selected based on the form of hyperlipidemia.
There are special clinical recommendations with a detailed classification of disorders and advice on what to do in each specific case.
Read more about the types of lipidemia and treatment methods in this article.
Autoimmune anemia
They are extremely rare. Usually secondary to the underlying disease. The inflammatory process leads to the destruction of formed blood cells. The body turns on compensatory mechanisms and oversaturates red blood cells with hemoglobin.
Treatment. Drugs are used to weaken the immune response. For example, glucocorticoids. Prednisolone, Dexamethasone and others.
They differ in their degree of activity and therapeutic potential. From the weakest (Beclazon) to the most powerful (Betamethasone).
If they do not bring the desired effect, they resort to immunosuppressants. Those drugs that directly inhibit the synthesis of cells of the body's defense system.
Attention:
That those that other medications cannot be used for a long time. Is it dangerous.
Electrolyte imbalances in the body
Change in the proportional ratio of potassium, calcium, sodium magnesium and water. Sometimes it is episodic. For example, after heavy physical activity, etc.
However, such situations do not fundamentally affect the state of hematopoiesis. When the process becomes persistent, problems begin.
Treatment: potassium preparations, other salts. Also a change in drinking regime. Under the supervision of a specialist.
If the mchc indicator is increased, this is always a consequence of a pathological process. Which one exactly needs to be clarified.
How to prepare for the test
To obtain the most reliable data, it is recommended to carry out a number of preparatory activities. They will help not to “blur” the overall picture and accurately diagnose any deviation from the norm. Before taking blood, you must refrain from eating at least 4 hours before the procedure. It is also recommended to exclude heavy physical activity, emotional disorders and stress the day before. When taking any medications, you should talk in advance with your doctor, who can evaluate their composition and understand whether taking them can affect the analysis. If medications affect the results, you will need to limit their use a few days before the test. You also need to stop drinking alcoholic beverages and drugs. To achieve reliability, it is better not to smoke before analysis.
The best option is to visit the laboratory in the morning, on an empty stomach. In the morning you are allowed to drink only a glass of clean water. Strong tea, coffee and any other snack are not allowed. If it is necessary to donate blood several times to monitor therapy or more detailed diagnostics, then it is best to do this at the same time and in a similar condition. It is also worth contacting an identical clinic or laboratory. By adhering to these rules, the influence of third-party factors on the results obtained will be reduced to almost zero.
Necessary therapy for a low MNCH index
If a reduced level of concentration of iron-containing protein in such elements is detected, medical professionals prescribe therapeutic treatment using medications that can increase the level of MNCH.
Having determined the reasons for the decrease in MNCH levels, doctors develop an individual therapeutic treatment plan. The basis of this treatment are:
- A vitamin complex with an element of group “B” included in its composition;
- Mineral components and additives;
- Preparations rich in components such as folic acid and iron.
With the described deficiency of pigment in the cells, patients under 3 years of age are recommended to take drugs in the form of Ferum, Lek, Actifferin, while older children are advised to take drugs in the form of Totem, Ferroplex, Tardiferon. The purpose of these particular drugs is due to the content of natural elements in their composition, which during the treatment process in no way can harm the child’s still fragile body.
The treatment process for the adult generation is based on the same medications, but in a much higher dosage. The duration of the prescribed course of treatment varies from 1 to 3 months, and the frequency of administration and individual dosage is calculated by the attending doctor, taking into account all the characteristics of the body of a particular patient, as well as based on the reasons that led to this condition.
The above-described therapy is complemented by the inclusion in the patient’s daily menu of foods rich in elements in the form of iron and folic acid.
How the research is carried out
To obtain data on MSI in a blood test, blood is drawn from a vein. In rare cases, it is possible to use finger capillaries (nowadays they are practically not used, as they are less accurate and informative). This procedure is performed by a nurse or laboratory worker who has the appropriate education and license to carry out this activity. Its duration is no more than 5 minutes and is accompanied by slight pain and discomfort at the puncture site. However, the discomfort quickly disappears, and a small bruise may remain at the puncture site. Persons who are afraid of the sight of blood are strongly advised to turn away and not look at the hand until the end of the procedure. But to prevent loss of consciousness and quickly restore consciousness, a cotton pad and ammonia are always present in the office. Blood sampling is carried out in several successive stages:
- Applying a rubber or fabric tourniquet with clamps to the forearm of the patient, who must work his fists a little (clench and unclench his hand several times to better fill the vessels).
- The technician or nurse selects the most appropriate vein and cleans the skin with an alcohol swab.
- Inserting a needle into a vein, through which blood flows into a syringe or special tube. Often, no more than 5 ml is collected.
- Remove the needle and apply cotton wool soaked in alcohol to the puncture site.
To prevent bruising or bruising, the patient is asked to press his forearm to his shoulder for a few minutes. At this point, the procedure ends and the medical worker signs the tube, after which the resulting material is placed in the analyzer. Its use makes it possible to automatically count all types of blood cells, including red blood cells. The obtained data is sent to the attending physician, after which the MCH blood test begins to be deciphered.
MCH norm indicators
The average amount of hemoglobin in one red blood cell varies depending on age and gender. Its average value in a healthy adult is from 27 to 31 picograms (pg). The highest rates are observed in infants under 14 days of age. They can vary from 30 to 37 pg and, as they grow older, gradually decrease and are compared with the norm for adults. Norms for women
| Woman's age, years | Norm MCH per red blood cell (in pg) |
| 16-18 | 26-34 |
| 19-45 | 27-35 |
| 46-60 | 27-34 |
| After 60 | 27-35 |
The norms for men are approximately the same as for women. Minimal deviations are observed. 46-6027-34 After 6027-35
| Man's age, years | Norm MCH per red blood cell (in pg) |
| 16-18 | 27-32,5 |
| 19-45 | 27-34 |
| 46-60 | 27-35 |
| After 60 | 27-34,5 |
Norms for children. It should be noted that these indicators are unstable; they can change within a matter of hours or days.
| Child's age, years | Norm MCH per red blood cell (in pg) |
| 1-4 months | 27-32 |
| 1-3 years | 23-31 |
| 7-15 years | 26-32 |
Deciphering the MCH blood test
Increase in MCH
If the MCH exceeds the upper permissible limit, then this indicates the presence of a pathological process in the body. Diagnosis of the underlying disease that provoked this change is carried out after determining the cause. In most cases, a similar jump is observed with hyperchromia. This term refers to a condition characterized by an increase in hemoglobin in red blood cells. As a rule, it develops when a person has some type of anemia. The MCH level in the blood increases under the following conditions:
- Severe leukocytosis.
- Exceeding the norm for the amount of fat.
- Increase in the number of heparins.
- Destruction of red blood cells caused by a number of diseases (malaria, poisoning with certain poisons or chemicals, hemolytic anemia, systemic lupus erythematosus, kidney damage, toxoplasmosis, systemic scleroderma, viral hepatitis B and C).
The reasons for such deviations may be a deficiency of vitamin B12, B9 and the use of certain medications (therefore, it is extremely important to carefully study the side effects indicated in the attached instructions, and also stop using the drug before taking the test). To prevent receiving false information, it is recommended to first consult with a doctor and clarify which medications the patient is currently taking. For example, in women, MSI may be affected by a long and uninterrupted course of contraceptive medications.
Other etiological factors that can cause an increase in MSI are:
- Liver damage (especially hepatitis and cirrhosis)
- Excessive drinking of alcoholic beverages and terminal stages of alcoholism.
- Leukemia.
- Neoplasms (both malignant and benign), localized in the bloodstream and other internal organs.
In addition, high hemoglobin levels are observed in individuals suffering from hyperthyroidism. This is a disease of the endocrine system, characterized by damage to the thyroid gland. Its main symptoms are organ enlargement, exophthalmos, increased physical activity, emotional lability, excessive appetite, weight loss, abnormal activity and accelerated metabolism. Often this pathology is diagnosed in residents of an endemic zone, in which, due to natural conditions, there is a low concentration of iodine.
Decreased MCH
If the interpretation of the MCH blood test showed a decrease in this indicator, then this result indicates the presence of another form of anemia - anemia of the hypochromic type. The most common type of this pathology is iron deficiency anemia, characterized by insufficient absorption of iron.
With a decrease in the relationship between Fe and hemoglobin, a noticeable change in the normal parameters of a clinical blood test occurs. In most cases, this indicates the following diseases:
- A source of inflammation localized in any part of the body.
- Disorder of metabolic processes affecting iron metabolism.
- Hypovitaminosis caused by malnutrition, internal pathologies and other etiologies.
- An intoxication period that arose against the background of long-term lead poisoning.
A decrease in MCH has a strong impact on the normal course of biochemical processes, as a result of which a person’s condition significantly worsens. As a rule, this causes rapid fatigue, weakness, pale skin, dry skin, brittle hair and nails. Often there is a feeling of dumbness in the upper and lower extremities, ulcers in the corners of the mouth and irregular heart rhythm.
Having identified any irregularities in the MCH indicators, you must immediately contact a qualified doctor. Only he, based on the laboratory data obtained, will be able to make an accurate diagnosis and select the most effective treatment method.
HGB (Hb, hemoglobin) – hemoglobin concentration
Most accurate method
Mindray systems use the cyanide-free methemoglobin method using imidazole as the ligand. The method is fast (10 seconds) and sensitive, much less affected by high levels of leukocytes in the blood than hemiglobin cyanide. The reagent (NaOH and lauramine oxide) dissolves all cellular particles and lipids and destroys bilirubin - thus eliminating interference due to hemoglobin turbidity. Therefore, this method provides more reportable results than any other.
False indicators
| The indicator may be overestimated as a result of: |
|
Clinical and diagnostic value
| An increase in hemoglobin concentration is observed when: | A decrease in hemoglobin concentration occurs when: |
|
|