Who, if not pharmacists and pharmacists, should know that ethanol is a typical representative of monohydric alcohols, capable of entering into various chemical reactions. It interacts with alkali metals, magnesium, aluminum, carboxylic, inorganic acids and many other substances, including medicinal ones. According to some data, up to 25% of visits to the emergency room are associated with various adverse reactions between alcohol and drugs [1]. And it is quite natural that such widespread unfavorable events have become fertile ground for various speculations. On the eve of a series of holidays, it’s time to find answers to the most controversial questions about interactions between drugs and alcohol, as well as dispel the myths associated with it.
Nonsteroidal anti-inflammatory drugs
This group of drugs is also known as antipyretics and painkillers. They are taken for fever and various manifestations of pain.
It is important to remember that ibuprofen, aspirin, analgin and their analogues have a pronounced hepatotoxic effect and negatively affect the condition of the gastric mucosa, increasing the risk of the formation of peptic ulcers of the stomach and intestines.
Ibuprofen in combination with alcohol significantly impairs blood clotting, which leads to an increase in bleeding time by approximately 3-4 times. The risk of bleeding from the gastrointestinal tract increases significantly, which can lead to irreversible blood loss.
All drugs in this group, in combination with alcohol, have a toxic effect on the gastrointestinal tract, especially if non-steroidal anti-inflammatory drugs are taken for a course of 10-14 days or more.
It is worth taking enough time to read the composition of combination drugs that modern pharmacology offers as a treatment for influenza and other viral infections. Most often they also contain paracetamol or ibuprofen.
You can take drugs of this class in the morning after drinking alcohol - it is known that analgin relieves hangover and helps you recover the next day. However, it is important to ensure that about 10 hours have passed since the last dose of alcoholic beverages, then the danger to the liver will be minimal. If there are initially risk factors for the development or exacerbation of diseases of the gastrointestinal tract, then it is better to get rid of discomfort due to alcohol consumption with the help of adsorbents - activated carbon or smecta.
BE CAREFUL: WHEN A DOUBLE HIT TO THE LIVER IS POSSIBLE
“Everyone knows that the processing and neutralization of alcohol occurs in the liver,” continues Yuri Kiselev. “Therefore, increased caution should be exercised when taking medications that are hepatotoxic, that is, capable of causing liver damage. This applies, for example, to chemotherapy drugs, anti-tuberculosis and antifungal drugs.
There are also a number of popular medications that are generally quite safe for the liver, but when drinking alcohol, especially unhealthy amounts, can harm the liver. These include statins and many non-steroidal anti-inflammatory drugs: diclofenac, celecoxib, naproxen.
In the era of Covid and vaccination against coronavirus, the demand for paracetamol has especially increased. They are advised to lower their temperature both during illness and if it rises after vaccination. How does it combine with alcohol?
“This is a separate interesting phenomenon,” the expert notes. — In general, paracetamol is a very safe antipyretic and analgesic if used in doses of up to 3-4 g per day and without severe liver disease. But against the background of frequent or heavy intake of alcohol, an enzyme is activated in the liver that converts paracetamol into a toxic metabolic product. As a result, under such circumstances (alcohol abuse), the medicine can cause severe liver dysfunction, even death.
If you abuse alcohol, regular paracetamol can cause severe liver dysfunction, including death.
Photo: Shutterstock
Rheumatology drugs
Rheumatoid arthritis, gout, various chronic inflammations of the joints - these pathologies are manifested by severe constant pain and require the prescription of serious anti-inflammatory drugs or other aggressive drugs. The use of cytostatics is especially dangerous - they have a pronounced damaging effect on the liver. Combining them with alcohol is unacceptable for those who are concerned about their own health.
Get a free consultation
+7 (495) 266-59-76
or make an appointment
Antibiotics
There is a well-known rule - drinking alcohol with antibiotics is absolutely contraindicated. However, few people know where this statement came from and what is associated with the fear of taking antibacterial drugs.
If you look deeper into the biochemical processes of the transformation of alcohol in the body, it is necessary to note the two-stage nature of its metabolism. Initially, with the help of the enzyme alcohol dehydrogenase, ethanol is broken down into acetaldehyde. It is this active substance that is considered toxic to all organs and systems; it has a direct destructive effect on cells. The further path of neutralization is conversion into acetic acid under the influence of the enzyme aldehyde dehydrogenase.
The second stage of alcohol elimination is disrupted or delayed, and acetaldehyde begins to actively circulate in the body. Its accumulation causes a severe hangover, which manifests itself in the form of headache, nausea, vomiting, and severe general malaise.
Antibacterial agents act directly on enzymatic systems, disrupting the work of aldehyde dehydrogenase and blocking the second stage of ethyl alcohol neutralization. The result of the simultaneous use of alcohol and antibiotics is a pronounced hangover syndrome, which brings excruciating headaches, dyspeptic symptoms in the form of nausea, vomiting and stool disturbances, changes in cardiac activity, changes in blood pressure, arrhythmias, and can even lead to breathing problems or seizures.
Significant amounts of alcohol may trigger health-threatening symptoms immediately after drinking, rather than the next day. This negatively affects both the physical and mental state of a person.
Several groups of antibiotics are guaranteed to provide such a reaction almost immediately - metronidazole and other imidazole derivatives are most often prescribed for the treatment of protozoal infections caused by protozoan microorganisms. A similar effect is exerted by first-generation cephalosporins, a number of nitrofurans, macrolides, as well as sulfonamides, for example, the well-known biseptol, which many patients do not at all classify as antibacterial drugs. Antifungal agents - ketoconazole, itraconazole - work similarly.
Antibacterial drugs that are used in the treatment of tuberculosis are especially dangerous - isoniazid, rifampicin and other drugs. They are quite toxic on their own, and in combination with alcohol lead to the development of irreversible changes in the liver parenchyma and other serious consequences.
Newer antibiotics of the latest generations cause such problems to a lesser extent, but unexpected reactions cannot be ruled out, which may be the result of individual sensitivity to the drugs.
It is important to understand that the level of drugs in the blood remains even after stopping the course of treatment. Antibacterial active substances remain active in the blood for some time, and it is important to refrain from drinking alcohol for several days or even weeks after the end of therapy.
Many patients wrongly believe that only tablet forms of antibiotics cause the dangerous effects of alcohol. In fact, solutions for intravenous or intramuscular injections, antibacterial suppositories enter the bloodstream much faster, and even local forms in the form of eye drops or ointments for external use can affect the metabolism of ethanol.
Thesis No. 7: Alcohol should not be combined with certain antidiabetic drugs.
Status: True
In case of diabetes mellitus, drinking alcoholic beverages is generally extremely undesirable - this threatens a sharp drop in blood sugar levels and the development of hypoglycemia, which is associated with a violation of the release of carbohydrates stored in liver cells against the background of alcohol intoxication. The risks of hypoglycemia in diabetic patients who drink alcohol are further increased due to possible drug interactions between ethanol and some sulfonylureas, in particular glipizide [3].
Combining alcoholic beverages with the first-line drug for the treatment of type 2 diabetes mellitus, metformin, can lead to increased levels of lactic acid in the blood and the development of lactic acidosis. The likelihood of its occurrence increases with a low-calorie diet, poor nutrition and liver failure. Therefore, metformin is incompatible with alcohol in both alcoholic beverages and alcohol-containing medications [3].
Insulin also interacts with ethanol. Alcohol can enhance or weaken the hypoglycemic effect of the drug, which can lead to the development of hypo- or hyperglycemia and, accordingly, worsening disease control [7].
Nasal drops
Swelling of the mucous membrane of the nasal passages is one of the most unpleasant symptoms of colds, which, together with a runny nose, leads to difficulty in normal breathing.
A symptomatic remedy to alleviate this condition is vasoconstrictor drops. Preparations of naphazoline and its analogues affect the walls of blood vessels, causing contraction of the muscle layer, thereby achieving the necessary effect of relieving swelling and improving breathing through the nose. Few patients think about the fact that such drugs are derivatives of adrenaline; they act in the body like this adrenal hormone. Ethyl alcohol also affects the secretion of stress hormones as an adrenergic agonist, so the combination of these substances in the body can be fatal. The main symptoms of an overdose are increased heart rate, increased blood pressure, emotional swings, and aggression.
QUESTION ON THE TOPIC
How soon is it safe to take medications after drinking alcohol?
- I can tell you the exact figure for the drugs metronidazole and tinidazole - after 72 hours. For other medications there is such a way to navigate. The instructions for the drug always indicate the so-called half-life of the drug. This figure (for example, 2 hours) needs to be multiplied by 5. And you will get the time (say, 10 hours) during which most of the drug will be eliminated from the body. But this is a very conditional rule, I advise you to consult a doctor,” says Yuri Kiselev.
— If it does happen that a person mixed drugs and alcohol, how to act correctly? Should I drink more water? Some people recommend activated carbon...
— Yes, activated carbon or other sorbents, and more water. It is also important to monitor the person, not leave him alone, and if his condition worsens, call a doctor.
Antidepressants
It is known that ethyl alcohol, some time after administration, especially when the dose is increased, inhibits the activity of the central nervous system. It leads to an increase in the action of its own serotonin against the background of more active synthesis of dopamine - the main hormones of pleasure. Thus, we can consider that alcohol is an independent antidepressant. The simultaneous use of alcohol and antidepressants can cause an unpredictable effect on serotonin receptors and provoke an excessive release of adrenaline. This situation is especially dangerous in the case of taking monoamine oxidase inhibitors (MAO) - iproniazid, nialamide, pyrazidol, selegiline. Another dangerous combination is MAO inhibitors with beer, since this popular drink contains one biologically active substance - tyramine, which affects all body systems like adrenaline. The processing and excretion of this biogenic amine occurs due to the enzyme monoamine oxidase; accordingly, MAO inhibitor drugs interfere with this natural process.
All antidepressants are quite hepatotoxic, and their combination with alcohol has an additional negative effect on the liver.
Alcohol is strictly contraindicated:
— During treatment with metronidazole and tinidazole. These are antimicrobial drugs that are included, in particular, in widespread treatment regimens for peptic ulcers and trichomoniasis (genitourinary infection). “The consequences of combination with alcohol can be very serious, even fatal,” the expert warns.
— During treatment with antibiotics, linezolid and doxycycline are also fraught with dangerous complications.
- When treated with drugs acting on the central nervous system. These include: sleeping pills, sedatives (including the most popular Valocordin and Corvalol), anticonvulsants, antidepressants, antipsychotics, narcotic painkillers, cough suppressants. “If a number of factors fail to coincide, the consequences of combining such drugs with alcohol can be fatal - for example, breathing may stop,” explains Yuri Kiselev. “For the monoamoxidase inhibitor drugs used to treat depression and Parkinson’s disease, alcohol can cause a sharp and dangerous increase in blood pressure.”
At the same time, a large number of people constantly or for very long courses take, say, anticonvulsants or antidepressants. So, they can’t have a drop of champagne either on their birthday or on New Year’s?! “For many of them, one glass of wine once a week will not cause much harm, but it is still better to abstain. As they say, God protects the careful,” notes the doctor. “The same applies to drugs that reduce blood clotting, which are prescribed against thrombosis.”
Medicines and alcohol
Photo: Nail VALIULIN
Tranquilizers
Psychotropic drugs for relieving anxiety and fear are a group of anxiolytics, most of which belong to the class of benzodiazepines. Drugs in this group have hypnotic, relaxing, sedative and anticonvulsant effects. The result of the simultaneous use of drugs along with alcoholic beverages is a sharp depression of the nervous system, which is manifested by severe intoxication, impaired coordination, and thought processes. Unexpected motor disturbances and respiratory arrest may occur.
Alcohol and its effect on blood pressure
Ethanol, entering the blood, triggers a series of biochemical reactions. Their effects on the body vary depending on:
- volume of alcohol consumed, type of drink;
- individual characteristics of the body, health status;
- presence of alcohol dependence;
- age.
Initially, the first dose of alcohol lowers vascular tone. They expand and become more elastic. Blood pressure decreases slightly. The heart rate increases, but the blood does not speed up. This factor affects the fall in blood pressure. This continues until the opposite happens - the vessels sharply narrow. The reason for this change is the concentration of ethanol in the blood: the nervous system “strains”, begins to work actively, and the production of adrenaline increases significantly.
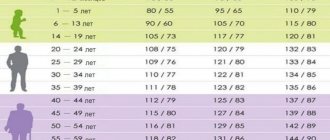
To prevent the negative impact of alcoholic beverages on human health, it is necessary to strictly adhere to the norm of alcohol consumption. It is individual for everyone. There are specific numbers recommended by the medical community. Medical doctors remind that they are valid for a healthy body.
Preparations for general anesthesia
Surgeons often have to perform urgent surgical interventions without special preoperative preparation. In this case, the patient may be intoxicated. This situation is only possible in cases where the consequences of not having surgery are worse than the risk of drug interactions with alcohol. It is important to remember that depression of the central nervous system when administering ether or intravenous anesthesia with diethyl ether, ketamine, sodium hydroxybutyrate, thiopental and other drugs can lead to depression of brain function, including respiratory arrest.
STAY IN TOUCH
Who needs special care
Alcohol has a stronger effect on older and very thin women and men, the expert notes. They have less water in their bodies and, accordingly, the concentration of alcohol and its breakdown products will be higher. Therefore, you need to be especially careful; the risk of adverse effects of combining alcohol with medications in such people increases.
In general, from a medical point of view, there are three important components that we must take into account, says Yuri Kiselev.
1. The effect of alcohol itself on the body.
2. The effect of alcohol directly on the drug - for example, accelerated or delayed processing of the drug in the liver.
3. The combination of the effects of alcohol and drugs on the body - say, sleeping pills and alcohol independently suppress the central nervous system.
Antiallergic
Most often, patients with various types of allergies are prescribed antihistamines. They block certain receptors and prevent the development of symptoms of hypersensitivity reactions. However, the first generations of this group of drugs are characterized by a pronounced sedative effect, causing drowsiness, and the combination of these active substances with alcohol causes the same reactions as tranquilizers. Ethanol blocks the main effect of antihistamines, so patients may experience allergic reactions with serious complications.
A great danger is the inhibition of the enzyme aldehyde dehydrogenase under the influence of histamine receptor blockers, which significantly disrupts the functioning of the systems for neutralizing alcohol metabolites.
Antihypertensive drugs and alcohol - compatibility of substances, consequences of use
Currently, hypertension is a very common disease. And treatment of hypertension involves long-term use of antihypertensive drugs. Of course, taking pills coincides with holidays and celebrations. And therefore, people have a natural question: is it possible to take antihypertensive drugs with alcohol?
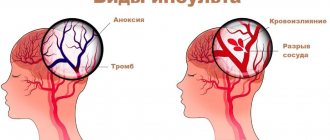
Classification of antihypertensive drugs
The development of arterial hypertension is indicated when systolic blood pressure rises above 140 mmHg. High blood pressure leads to impaired blood supply to internal organs, especially the brain and heart. And this, in turn, is fraught with the development of such dangerous conditions as stroke and subarachnoid hemorrhage.
Antihypertensive drugs are prescribed to treat hypertension. These are different groups of drugs that lower blood pressure through various mechanisms of action. Thus, the following groups of antihypertensive drugs are distinguished:
- ACE inhibitors (Enalapril, Captopril);
- Diuretics (Hydrochlorothiazide, Furosemide);
- Angiotensin II receptor blockers (Losartan, Valsartan);
- Beta-blockers (Atenolol, Labetalol);
- Calcium antagonists (Verapamil, Amlodipine);
- Combination drugs (Captopres, Liprazide).
If arterial hypertension is detected, treatment begins with the administration of one drug in a minimum dosage; if necessary, the dose is gradually increased. When such a treatment regimen does not have the desired effect, then a combination of several antihypertensive drugs from different groups is prescribed.
Compatibility of blood pressure pills with alcohol
When prescribing antihypertensive drugs, doctors warn their patients against drinking alcoholic beverages. This limitation is due to the fact that alcohol enhances the hypotensive effect of the drug. It would seem that lowering blood pressure is a good thing? However, the use of antihypertensive drugs with alcohol leads to a sharp and severe decrease in blood pressure, and this is another undesirable extreme.
It is important to understand that a critical drop in pressure leads to disruption of the blood supply to internal organs, which means oxygen starvation of tissues develops. The brain is the first to suffer from a lack of oxygen.
Signs indicating the development of acute arterial hypotension are:
- Severe weakness;
- Cold extremities;
- Pale skin;
- Headache;
- Dizziness;
- Fainting.
The use of antihypertensive drugs with alcoholic beverages is especially dangerous for people suffering from coronary heart disease or vascular diseases of the brain . In such patients, a sudden and excessive decrease in blood pressure can lead to myocardial infarction or stroke.
What happens if you take alcohol with blood pressure pills?
So, alcohol enhances the hypotensive effect of antihypertensive drugs, which is fraught with serious consequences. Therefore, antihypertensive drugs should not be taken with alcoholic beverages. What to do in such a situation if an important celebration is coming up? First of all, you should never stop taking medications completely, as this can ultimately lead to a hypertensive crisis. It is worth consulting with your doctor on this issue; sometimes, as an exception, when treating arterial hypertension, drinking alcohol in small quantities is allowed.
Separately, it is worth mentioning the use of antihypertensive drugs for hangovers. Often, after a wild party, people wake up the next morning with high blood pressure. This is an extremely dangerous condition that can lead to hypertensive crisis or stroke. In such situations, it is imperative to reduce blood pressure with the help of antihypertensive drugs, despite the fact that a small amount of alcohol still remains in the blood.
Valeria Grigorova, doctor, medical columnist
2, total, today
Cardiac products
One of the groups of antiarrhythmic drugs and drugs that lower blood pressure are adrenergic blockers, such as timolol, atenolol, propranolol and other representatives of the class. A large percentage of people constantly take nitrates - drugs against angina pectoris, which dilate the blood vessels of the heart and improve its blood flow.
Their interaction with alcohol can be unpredictable - it enhances the vasodilatory effect, dilating peripheral and central vessels, therefore, with a sharp transition from a lying position to a standing position, a sudden drop in blood pressure may occur. Symptoms of this condition are clouding of consciousness, severe weakness, flashing “spots” before the eyes, nausea, and coordination problems.
Accordingly, for the same reasons, you cannot combine the intake of alcoholic beverages and antihypertensive drugs. The decrease in blood pressure can be so rapid that an emergency situation arises - a hypotensive crisis.
Indirect anticoagulants such as phenindione, omefin or neodicoumarin are indicated as treatment or prevention of blood clots. Taking these medications on a regular basis can prevent the development of serious conditions such as heart attack or stroke. However, there is a main risk of their long-term use - the risk of bleeding. Also, in people who are not prone to drinking alcohol, a single dose of large doses of alcohol enhances the effect of indirect anticoagulants. This may pose a greater risk of developing internal hemorrhages. The opposite situation occurs among those who systematically allow themselves a glass or two of strong drinks. Their tolerance to the action of these drugs increases, and there is an additional risk of thrombosis.
Thesis No. 1: Alcohol is incompatible with any antibiotics
Status: Myth
Indeed, a number of antimicrobial agents block acetaldehydrogenase, delaying the enzymatic biotransformation of ethanol at the stage of extremely toxic acetaldehyde. Its accumulation in the body contributes to the development of intoxication, which is accompanied by severe sensations. In fact, these drugs work in the same way as the famous disulfiram, used to treat alcohol addiction, which simply causes poisoning of the body. Its typical symptoms are difficulty breathing, tachycardia, nausea and vomiting, low blood pressure, fever or chills.
However, only a few antimicrobial drugs act in this way, in particular: cefamandole, cefoperazone, chloramphenicol, griseofulvin, isoniazid, metronidazole, ornidazole, nitrofurantoin and sulfamethoxazole.
All other antimicrobials do not have strict restrictions when combined with ethanol, but this does not mean that their combination helps to effectively fight infection.
Drugs for the treatment of gastrointestinal diseases
Histamine H2 receptor blockers, such as cimetidine, ranitidine or famotidine, reduce the acidity of the gastrointestinal tract. This leads to rapid absorption of alcohol and increased effects. It is important to remember that if you have gastritis or peptic ulcers, drinking alcohol is absolutely contraindicated. Violation of the ban can lead to the formation of ulcerative defects in the gastric mucosa.
Another group of medications that are prescribed to improve gastrointestinal motility, bile secretion and other processes for digesting food are antispasmodics. The well-known “No-shpa” and its analogues relax the muscles of the internal organs. Ethanol potentiates the effect of the drug, causing stronger muscle relaxation effects, which makes it difficult to choose a safe dose of the antispasmodic.
Get a free consultation
+7 (495) 266-59-76
or make an appointment
Arterial hypertension and alcohol
Arterial hypertension is one of the most socially significant pathological conditions. It is detected in 20-30% of the adult population of industrialized countries and is one of the leading causes of disability and mortality in the population, often in working age. The heterogeneous group of arterial hypertension includes conditions caused by potentially reversible causes. Among them are ethanol-induced increases in blood pressure (BP). Chronic or acute alcohol consumption causes 5-25% of all hypertensive conditions.
The results of epidemiological studies conducted in Russia in recent years indicate a direct connection between alcohol consumption and mortality from pathologies of the circulatory system, especially in working age. Among the main causes of premature death are progressive heart failure and vascular accidents in the cerebral artery basins. Risk factors for this include chronic alcohol intoxication and dysregulation of blood pressure.
The first reports on the connection between alcohol and blood pressure (BP) have been known since the beginning of the 20th century. A study of French army officers revealed a persistent increase in blood pressure in those who consumed more than 2.5 liters of wine per day. To date, more than 70 epidemiological studies have been conducted to study the relationship between blood pressure and alcohol consumption. Their result is the emergence of several models of the relationship between alcohol consumption and hypertension: threshold - a convincing connection between alcohol and hypertension begins with a certain dose; linear, in which the degree of increase in blood pressure is directly related to the amount of alcohol consumed; J-shaped - abstainers have higher blood pressure numbers than those who consume alcohol in moderate quantities.
The range of threshold doses is very high, but its minimum value in studies was 24 g of conventional 100% ethanol per day. A linear relationship exists regardless of salt and coffee consumption, smoking, obesity, ethnicity, and level of education. Higher blood pressure levels were found in men who consumed alcohol. The so-called “J-shaped” dependence is largely due to the fact that among abstainers there are more often people with a lower health index and initially higher blood pressure values than among people who are able to drink alcohol at least occasionally.
The effect of the predominantly consumed drink (beer, wine, vodka) on arterial hypertension is insignificant. The “French paradox”, which consists in a decrease in the incidence of coronary artery disease with high consumption of red wines, is not observed in relation to blood pressure. Threshold doses are calculated in terms of pure alcohol and are approximately the same for Mediterranean countries (wine) and northern countries (spirits). A study conducted in the Czech Republic on men consuming almost exclusively beer found a low dose threshold of 24 g per day in terms of ethanol.
Alcoholic hypertension is heterogeneous in its clinical course. Factors that predominantly affect systolic or diastolic blood pressure are shown above. In patients with stages I and II of alcoholism after alcoholic excesses, more often on days 1-5, there is an increase in blood pressure to 180/100 - 160/90 mm Hg. Ophthalmoscopy reveals dilation of the veins and sometimes a slight narrowing of the arteries. Repeated excesses with a subsequent increase in blood pressure can lead to the formation of persistent arterial hypertension with characteristic clinical manifestations. In alcoholic hypertension combined with coronary artery disease, the most common course is a crisis, especially in women. In patients with alcoholism and arterial hypertension, left ventricular function is reduced compared to hypertensive patients without ethanol dependence. In alcohol withdrawal syndrome, transient hypertension is an obligate symptom. Detoxification leads to normalization of blood pressure.
To date, there is no convincing data on the special pathogenetic mechanisms of the formation of alcoholic hypertension. Hypotheses about the activation of the sympathetic nervous system and an increase in the content of catecholamines in the blood, an increase in the activity of the renin-angiotensin system, disruption of the transport of calcium ions into vascular cells, a decrease in the synthesis of nitric oxide (NO), which is a natural vasodilator, the influence of nephropathy, and others are considered.
Long-term alcohol consumption is a chronic stress for the body, increasing the activity of catecholamines. Hypertension that develops during alcohol withdrawal syndrome is almost entirely of catecholamine origin, at least in the first 72 hours of the full clinical picture of withdrawal.
Data were obtained on the direct effect of ethanol on blood vessels, mainly on the resistance in the medial layer of the vascular wall and the absence of an effect on the mass of circulating blood. Chronic consumption of ethanol is accompanied by a decrease in the concentration of Mg ions in the blood, which leads to a decrease in the activity of Na-K-ATPase and Ca-ATPase, a decrease in the concentration of Na and Ca ions in the cell and, finally, to vasospasm. The central effect of alcohol is manifested by activation of the sympathetic nervous system, which leads to an increase in blood pressure due to vasoconstriction and an increase in heart rate. At the same time, the baroreflex deteriorates due to interaction with brain stem receptors. Systematic formation of excess amounts of acetaldehyde during systematic alcohol abuse leads to oxidative stress (peripheral mechanism of hypertension). The main metabolite of ethanol, acetaldehyde, causes a sympathomimetic effect associated with catecholamine release and manifested by increased cardiac output, increased oxygen consumption, pulmonary and systemic pressure. For the treatment of arterial hypertension during post-alcohol withdrawal syndrome, centrally acting drugs (clonidine) and (-adrenergic blockers) are considered the most effective drugs.
A sharp increase in renin activity has been described during chronic alcohol intoxication. Some authors believe that this factor is more important than the catecholamine mechanism in the formation of alcoholic hypertension. Activation of the cascade of reactions of the renin-angiotensin system caused by acetaldehyde is known.
The attention of specialists is drawn to the relationship between ethanol and the mechanisms of NO synthesis, which has a vasodilating effect (inhibition of interleukin-1(-induced oxide synthase). It has been shown that alcohol can increase the production of superoxide and other vasoconstrictor free radicals due to dysregulation and changes in the functioning of the NO synthesis system in the vascular endothelium. Ethanol , in addition, causes dislocation of bacterial intestinal systems, the endotoxins of which also reduce the formation of NO. Low levels of intracellular arginine resulting from insufficient nutrition or the direct effect of alcohol deprive the NO synthesis system of raw materials and inhibit the formation of both NO and tyrosine kinase, which plays an important role in vascular relaxation.
Nephropathy with damage to the glomerular apparatus, detected in patients who abuse alcohol, can also serve as a factor in the formation of arterial hypertension. Among the possible causes of nephropathy are hyperuricemia, the toxic nature of nephropathy, and Na+ reabsorption disorders.
Treatment of alcoholic hypertension is associated with certain difficulties. There are reports of the ineffectiveness of ACE inhibitors, in particular lisinopril; a lesser effect of indapamide and chlorthalidone has been shown.
The main way to prevent alcoholic arterial hypertension in people is to avoid drinking alcohol. Randomized controlled studies of large cohorts of alcohol consumers found regression of hypertension after abstaining from alcohol after 2 months. Reducing alcohol consumption is recommended as the most effective way to reduce the consequences of alcoholic hypertension and prevent it. Complete abstinence from alcohol leads not only to better stabilization of blood pressure under the influence of treatment, but also to its reduction to normal levels. Let us recall that currently systolic blood pressure is considered optimal <120 mm Hg, diastolic blood pressure is <80 mm Hg, and normal is <130 and <85 mm Hg, respectively. In practical terms, most likely, there are no convincing differences in diagnostic and therapeutic algorithms that fundamentally distinguish alcoholic hypertension from other types of arterial hypertension.
Severe alcoholic excesses and especially post-intoxication syndrome are accompanied in some cases by an individually significant increase in blood pressure, which can lead to damage to target organs (hypertensive encephalopathy, intracranial hemorrhage, unstable angina and myocardial infarction, pulmonary edema, dissecting aortic aneurysm, eclampsia). This condition is an absolute reason for an emergency reduction in blood pressure. It should be emphasized once again that the blood pressure values at which these lesions are possible are individually variable and can fluctuate even in one person. In this regard, the previously practiced practice of diagnosing a “hypertensive crisis” based on blood pressure figures does not seem entirely correct (although many authors believe that diastolic blood pressure should be > 120 mm Hg).
Emergency care for a hypertensive crisis should be limited to a rapid decrease in blood pressure (not always to normal values), and therefore the most preferable is the administration of drugs in parenteral form.
Enalaprilat is a fairly safe means for smoothly lowering blood pressure. The drug is administered intravenously as a bolus in a dose of 0.5-1 ml of solution for injection over 3-5 minutes under blood pressure monitoring. When a crisis develops against the background of post-intoxication syndrome, it is advisable to administer intravenous (-blockers) (propranolol 1 mg for 1 min to a total dose of 5 mg or metoprolol 10 ml of injection solution under careful monitoring of hemodynamic parameters).
If the crisis is complicated by an attack of ischemic heart disease or acute left ventricular failure, it is necessary to start an intravenous infusion of nitrates - nitroglycerin 6.0-10.0 in 400 ml 0.9 percent. solution of sodium chloride or isosorbide dinitrate 10.0 intravenously in a stream, then 10.0-20.0 dropwise per 400 ml 0.9 percent. sodium chloride solution.
The phenomena of cardiac asthma and pulmonary edema require the administration of diuretics, preferably loop diuretics due to the speed of onset of action and clinical effectiveness - furosemide (Lasix) 60-100 mg intravenously or intramuscularly.
In the absence of parenteral forms of drugs, sublingual administration of 10 mg of nifedipine or 25 mg of captopril is successfully used. Taking clonidine has no advantages over nifedipine, but is associated with a greater risk of side effects.
In all cases of the development of a hypertensive crisis, a 12-lead ECG should be taken, and consultation with a neurologist is advisable. A hypertensive crisis in a patient who abuses alcohol most often indicates the acute phase of alcohol withdrawal syndrome. In general medical practice, such patients should be considered as a group at increased risk of alcoholic delirium (toxic cerebral edema), which is fraught with fatal complications. To prevent alcoholic psychosis, it is advisable to prescribe phenazepam 5-10 mg orally every 4-6 hours for 3-4 days. If hallucinations occur, an urgent consultation with a psychiatrist-narcologist is necessary.
Pavel OGURTSOV,
Head of the Department of Somatic Rehabilitation of the National Scientific Center for Narcology of the Ministry of Health of the Russian Federation, Doctor of Medical Sciences.