Heart block is an abnormal heart rhythm in which the heart beats too slowly. Why is this happening and what to do? Let's find out together with the experts. Each heartbeat occurs in the heart's upper right chamber (atrium) in the sinus node, a bundle of specialized cells that act as the heart's natural pacemaker. When it beats, an electrical signal from the upper chambers goes to the lower chambers, which causes the heart to contract and pump blood. Heart block disrupts this normal rhythm.
Degrees of heart block in adults
Heart block can be first, second, or third degree, depending on the electrical signal abnormality.
First degree heart block. In this case, the electrical impulse still reaches the ventricles, but travels through the AV node more slowly than usual.
Second degree heart block. It is divided into two categories:
- Type I, also called Mobitz block I or Wenckebach AV block, is a less severe form of second-degree heart block in which the electrical signal on its way to the ventricles becomes slower and slower;
- type II, also known as Mobitz block II - in this case, some electrical signals do not reach the ventricles at all, and the heartbeat may be slower than usual.
Third degree heart block. In this embodiment, the electrical signal from the atria to the ventricles is completely blocked. To compensate, part of the ventricles acts as a pacemaker, creating electrical signals. These signals cause the heart to pump blood, but much more slowly than normal.
Prevention
Prevention of atrioventricular (AV) heart block involves treating the underlying disease. Additionally, the patient is prescribed a cardiological diet, moderate physical and emotional stress, and cessation of smoking and alcohol consumption. It is important to follow the doctor's prescriptions and recommendations for successful therapy.
To prevent the development of the disease, it is necessary to undergo a timely examination by a cardiologist. At the cardiology center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency, specialists will select an examination program for you and prescribe adequate treatment.
Take care of yourself and your heart!
Causes of heart block in adults
The most common cause of heart block is a heart attack.
Other causes include heart disease, problems with the structure of the heart (due to defects) and rheumatism. The blockage can also be caused by damage during open heart surgery, as a side effect of certain medications or exposure to toxins. Heart block can be congenital, but it is a rare pathology. The risk of heart block increases with age and the presence of heart disease.
First-degree heart block is common in well-trained athletes, teenagers, young adults, and people with a highly active vagus nerve.
Diet food
After diagnosing a patient with a transient 1st degree blockade, cardiologists recommend changing the diet.
To improve conductivity in the AV node, it is necessary that the foods consumed have enough potassium, magnesium and calcium.
Products that improve AV node conduction:
- seeds;
- honey;
- dried fruits;
- bananas;
- baked potatoes with skins;
- dairy products;
- seafood;
- cottage cheese, sour cream, cheese;
- fresh fruits;
- vegetables;
- sea fish.
Salted and smoked foods, confectionery sweets, and artificial fats are excluded from the diet. If you are obese, you need to lose those extra pounds that put a strain on the heart.
Transient AV block: what not to eat:
- lard, meat with fat;
- animal fats, butter;
- strong broths;
- canned food and marinades;
- sour cabbage;
- seasonings and sauces with hot pepper;
- chocolate;
- coffee;
- cocoa;
- Black tea;
- alcoholic drinks;
- sparkling waters.
On the table of a patient with cardiac disease there should be vegetables, preferably fresh or stewed in olive oil, porridge, boiled, lean meat, and dairy products.
If you have high cholesterol, the number of eggs is limited; it is advisable not to serve them whole, but to add them to dishes according to the recipe. Fresh bread made from white flour is replaced by bread made from wholemeal flour, baked yesterday.
Diagnostics
First, the cardiologist will review the patient's medical history and ask questions about your general health, diet and activity level, and family medical history.
In addition, he will ask about the medications the patient is taking, as well as about bad habits. The doctor will then listen to your heart and check your pulse for signs of heart failure, such as fluid retention in your legs and feet.
In addition, to diagnose heart block, use:
- ECG – this will show the heart rate and rhythm, as well as the timing of electrical signals as they pass through the heart;
- A Holter monitor is a portable ECG that is attached to the patient’s body and records heart activity from 24 to 48 hours;
- An event monitor is another type of portable ECG that is worn over an extended period, where the device records heart activity at specific times rather than continuously;
- Electrophysiology test - This test uses thin flexible wires (catheters) that are placed on the surface of the heart to record its electrical activity.
Providing first aid during an attack
An attack of blockade requires immediate action. It is necessary to call an ambulance, but even before the doctors arrive, the patient is given first aid.
The person is placed on his back with a pillow placed under his head. To alleviate the condition, you can give isadrin, one tablet under the tongue. If the patient has lost consciousness, artificial respiration and chest compressions will help revive him.
The ambulance team will take the following measures:
- Administration of adrenaline and norepinephrine intravenously.
- Atropine is injected subcutaneously.
- The cardio-aortic plexus is blocked with novocaine.
- A defibrillator is used.
The patient is urgently hospitalized in the intensive care unit.
Popular questions and answers
Cardiologist Stanislav Snikhovsky answered our questions about heart block.
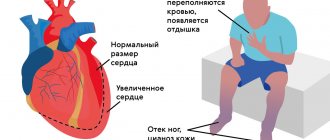
What complications can occur with heart block?
Clinically, all heart blocks are manifested by slowing of the pulse.
When the pulse rate decreases, fainting conditions associated with a lack of blood circulation to the brain may develop. Patients may complain of irregular heartbeat, headache and shortness of breath. With complete heart block (pulse about 40 beats per minute or less), Morgagni-Edams-Stokes syndrome develops, which is manifested by convulsions and loss of consciousness. Complete heart block causes rapid development of heart failure and can be fatal.
When to call a doctor at home if you have a heart block?
If there is sudden general weakness or fainting, a rare (less than 50 beats per minute) or very weak pulse, a feeling of irregular heartbeat, sudden shortness of breath and a feeling of lack of air, you should immediately call an ambulance.
Classification
There are several types of heart block. They are divided based on the location of the area where the conduction function of the heart is difficult or completely blocked. Due to the development of the disease in different parts of the heart, each blockade has its own characteristic features.
Photo: psodaz / freepik.com
Sinoatrial blockade
Sinoatrial block or sick sinus syndrome (SSNS) develops as a result of complete or partial dysfunction of the sinus node. This can occur both as a result of physiological disorders and due to other factors not related to the state of the body (extracardiac factors).
The main cause of SSSS can be considered fibrosis (development of connective tissue and its scarring) of the sinus node tissue. This pathology can be caused by inflammatory processes, increased tone of the vagal nerve, or taking medications.
SSSU can manifest itself:
- shortness of breath;
- general weakness of the body;
- pain in the heart;
- dizziness and loss of consciousness;
- low blood pressure;
- arrhythmia.
Interatrial block
Interatrial block develops when the propagation of electrical impulses is disrupted, both within and between the atria. The propagation of excitation occurs along special conduction pathways, which are circular and longitudinal muscle bundles, usually not described as part of the specialized conduction system of the heart.
One of the mechanisms of changes in the electrophysiological properties of the atrial myocardium, leading to a slowdown in conduction, is the development of fibrosis. There is a violation of the integrity of myocardial cells with the deposition of collagen in the intercellular space, which prevents the movement of impulses throughout the heart.
Accompanied by general weakness, pain in the chest and abnormal heart rate.
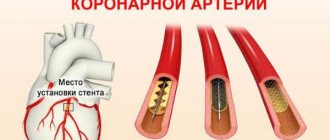
Atrioventricular block
Atrioventricular (AV) block is a partial or complete interruption of the transmission of impulses from the atria to the ventricles, leading to disturbances in heart rate and blood flow rate.
There are 3 types of atrioventricular block:
- 1st degree - due to a slow transition of impulses from the atria to the ventricles;
- 2nd degree - characterized by blocking of some impulses;
- 3rd degree - (complete atrioventricular block), associated with blocking of all impulses coming from the atria to the ventricles.
It occurs due to damage to the most sensitive area of the conduction system of the heart - the atrioventricular junction.
Intraventricular block
Intraventricular block occurs when the His bundle, the conducting region of the heart located in the region of the ventricles, is disrupted. The bundle of His consists of 3 branches: the left and right anterior branches and the posterior branch. The posterior branch is also divided into right and left.
Figure 1. Differences in ECG readings with normal rhythm and with blockades.
Intraventricular block is classified based on damage to 1 of 3 branches:
- Blocking of the anterior right branch - the innervation of the right ventricle is disrupted;
- Blocking of the anterior left branch - in case of disruption of the innervation of the left ventricle;
- Blocking of the posterior branch - the work of the His bundle is disrupted to the greatest extent, since along this branch impulses go from the atria to the ventricles, and are subsequently divided into right and left;
- Three-bundle block is associated with disruption of the conduction of the entire His bundle.
Mobitz Option 1
In a number of cases, atrioventricular conduction seems to gradually deteriorate with each subsequent conduction of the next sinus impulse, reaching such a deterioration at a certain point that conduction of the impulse becomes impossible.
Let's assume that four impulses come out of the sinus node. The first of them will pass the atrioventricular connection without a significant delay (travel time - P-Q interval is 0.12″). The second impulse will also pass through the atrioventricular junction, but will take more time to do so than the first (travel time - P-Q interval is 0.14″). The third impulse will also pass through the atrioventricular connection: with great difficulty, with a long delay - but it will pass (travel time - P-Q interval is 0.16″). But the fourth impulse was unlucky: atrioventricular conduction by this moment had deteriorated so much that its implementation became impossible.
Incomplete atrioventricular block 2nd degree, Mobitz 1, 4:3
This option of blocking the conduction of the sinus impulse along the atrioventricular connection is called the Mobitz 1 variant. In this case, the periodicity of the passage of sinus impulses is 4:3, i.e. Of the four sinus impulses, only three passed through the atrioventricular connection.
Naturally, with the Mobitz 1 option, other periodics can also be observed, for example 5:4, 6:5, etc. There may also be different rates of gradual obstruction of the conduction of each subsequent sinus impulse, and as a result, the transit time of the atrioventricular connection will be different from our case, for example, a change in the P-Q interval within the range of 0.16″-0.19″-0.22″ .
The gradual lengthening of the P-Q interval was described independently by Wenckebach and Samoilov. In their honor, this type of periodicals is called the Wenckebach-Samoilov periodicals.