General picture of the disease
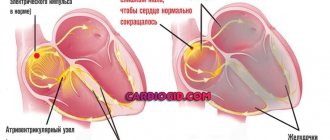
The structure of the His bundle involves the presence of two anterior legs and a posterior one. The branch on the right has a wide bundle that penetrates the muscle layers of the right ventricle. To understand what right heart branch block is, it is necessary to consider the features of the changes observed in this case:
- Throughout the cardiac system, the conduction of impulses slows down.
- The right parts of the organ are excited, affecting the septum present between the ventricles.
- The unblocked left ventricle is involved in the process, after which the right one is also excited.
Impaired conduction along the right bundle branch can negatively affect the functioning of the ventricles, as a result of which the time of their excitation changes. As a result, loss of normal performance of the right departments is possible.
Against the background of the development of this pathology, impulses can reach the left bundle of His without changes, without spreading to the right leg. Due to this disconnection in the functioning of the parts of the heart, the development of serious pathologies of the organ is possible.
Detection of conduction disorders using Holter monitoring.
Akselrod A.S., Head of the Department of Functional Diagnostics,
Cardiology Clinic of the MMA named after.
THEM. Sechenov Conduction disturbances are less common in cardiologist practice than cardiac arrhythmias. However, a significant proportion of syncope of unknown origin is represented by conduction disorders. If they are transient (which happens quite often), it is extremely difficult to detect them when recording a standard ECG. In such a situation, consistent use of a 24-hour recorder over 3 days or a single use of a 72-hour recorder is absolutely recommended.
As is known, patients with various conduction disorders may not present any complaints for a long time. In such situations, the appearance of syncope is often the first indication for Holter ECG monitoring.
During 24-hour ECG recording, it is possible to detect conduction disturbances that occur only at night. Of course, daily ECG monitoring also reveals the connection between conduction disorders and medication use, physical activity, etc. Transient sinoatrial and atrioventricular blockades, transient frequency-dependent blockades of intraventricular conduction, changes in the degree of previously diagnosed blockade - this is an incomplete list of the most common conduction disorders, which can only be identified with long-term ECG monitoring.
When purchasing software, you should pay attention to the mandatory presence of three features:
1. changing the tape drive speed: this feature allows you to more clearly set the boundaries of the PQ interval and PP distance;
2. changing the overall voltage: this feature allows you to increase the amplitude of the P wave and, thus, visualize it more clearly in doubtful cases;
3. the presence of a ruler with colored stretchable jaws: when you set these jaws to the interval you need, its duration in ms automatically appears on the fragment.
Sinoatrial blocks
associated with a slowdown (grade 1) or disruption (grades 2 and 3) of the generation or conduction of sinus node impulses to the atrial myocardium and, accordingly, the atrioventricular node. Sinoatrial block can be transient or permanent, occur at any heart rate and be combined with other conduction and heart rhythm disorders.
Sinoatrial block 1st degree
can be suspected by fragments of a sudden slowdown in rhythm followed by its acceleration (difficult to differentiate with sinus arrhythmia) during Holter monitoring.
With 2nd degree SA blockade
Some of the impulses arising in the sinus node do not reach the atria. In this case, a pause (more than 2 seconds) without atrial activity is recorded on the ECG: unlike AV block, during a pause with SA block there are no P waves.
With 2nd degree block of type I (partial sinoauricular block with Samoilov-Wenckebach periods)
There is a progressive shortening of the RR intervals before a long pause - Samoilov-Wenckebach periodics. In this case, the degree of conduction disturbance can be characterized by the ratio of the number of sinus impulses, for example, 3:2, etc. (in the numerator the number of sinus signals is set
impulses, including the expected and failed impulses; the denominator is the number of actually conducted impulses). The detected pause is not a multiple of the distance PP of the main rhythm.
For sinoatrial block of the 2nd degree, type II (Mobitz type)
no such periodicals are found. This type of blockade is diagnosed more often. The identified pause is a multiple of or equal to one distance PP of the main rhythm. Often, with this type of blockade with a 2:1 or greater degree of blockade, it becomes necessary to differentiate monitoring fragments from sinus bradycardia. Often, during the same Holter registration, it is possible to register both types of SA blockade.
Pay attention to the ability of your software to display in each of the printed fragments both the duration of the pause and the heart rate value against the background of this pause. This marking makes the fragment very visual and once again emphasizes its diagnostic significance (Fig. 1).
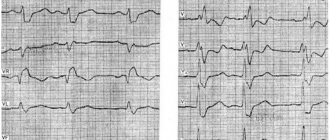
Rice.
1. Patient S., 64 years old, variants of sinoatrial block of the second degree: A - C A block of the 2nd degree, type I with Samoilov-Wenckebach periodicity; B – SA blockade 2nd degree type II with 3:2.
A
B
About the third degree of sinoatrial block (complete sinoatrial block or sinus node failure, “sinus arrest”)
they speak in the absence of atrial waves and the presence of replacement contractions from the distal centers of automaticity - the AV connection or the ventricular conduction system (Fig. 2).
Often during Holter monitoring one can see fragments of conduction disturbances that occur against the background of respiratory arrhythmia. In such a situation, it can be quite difficult to qualify the identified pauses. For example, in patient Zh., 45 years old, at night (from 2:00 to 5:00) episodes of SA conduction disturbance were recorded without multiplicity and clear Samoilov-Wenckebach periodicity, 9 pauses of more than 4 seconds, including 2 episode of sinus node arrest.
Fig.2. Patient Zh., 45 years old: A - episodes of slowing of SA conduction without a clear multiplicity and Samoilov-Wenckebach periodicity, B - arrest of the sinus node with the formation of a pause of 4.048 sec.
A
B
For novice doctors, I would like to note three important points:
1. often the degree and type of blockade may vary depending on the time of day;
2. the lack of multiplicity of the PP interval and the duration of pauses may be due to concomitant sinus arrhythmia, often respiratory;
3. when qualifying a pause as an SA blockade, you must be absolutely sure that this fragment is not artificial: the pause is duplicated in both leads. In doubtful cases, monitoring will have to be repeated.
Atrioventricular blockade.
Atrioventricular (AV) blocks are caused by damage to the conduction system at the 2nd and 3rd levels - the conduction of the sinus impulse to the atrioventricular node, as well as pathology of the atrioventricular node itself. In this case, both a delay in the conduction of the impulse from the atria through the AV node, and a complete cessation of its conduction are possible.
Prolongation of the PQ interval by more than 200 ms in adults and more than 170 ms in children indicates 1 degree of AV block (slowing of AV conduction)
. Incidental detection of this type of blockade at night in patients taking beta-blockers and not showing any complaints is one of the most common favorable conduction disorders in practical cardiology and can be qualified in conclusion as “slowing of AV conduction” if PQ does not exceed 300 msec (Fig. 3).
Rice. 3. Patient R., 57 years old: slowing of AV conduction was detected during night sleep (PQ interval reached 240 ms). A – PQ 146 ms (15:10), B – PQ 240 ms (4:33).
A
B
A much greater danger is posed by a significant (more than 300 ms) slowdown in AV conduction, which must be qualified in the conclusion as “1st degree AV block” (Fig. 4). When a PQ interval of more than 300 ms is recorded on the resting ECG, the patient is advised to have 24-hour ECG monitoring to decide on the need for therapy correction. Such severe conduction disturbances often progress over the course of a day.
Fig.4. Patient G, 64 years old: 1st degree AV block
“Loss” of the ventricular complex (pause, a multiple of the duration of the RR interval) with registration of an unchanged P wave (as opposed to sinoatrial block) is a sign of 2nd degree AV block
.
With an increasing lengthening of the PQ interval before the pause, they speak of type I partial AV block of the 2nd degree with Samoilov Wenckebach periods (Mobitz type I)
.
In the absence of such periodicals, type II AV block of the 2nd degree (Mobitz type II)
. It is convenient to indicate the degree of conduction using the ratio 5:2, 3:2, etc. (the first digit indicates the number of P waves, the second - the number of ventricular QRS complexes). It can be extremely useful to use graphs (or tables) of the distribution of pauses by hour. At the same time, having distribution graphs in your program is much more convenient: they are more visual and allow you to quickly and correctly assess the prevalence of pauses by hour (Fig. 5).
Fig.5
.
Patient B, 76 years old: 2nd degree AV block, type II.
A – stereotypical fragment of blockade with the formation of a pause of 2.288 sec; B – graph of the distribution of pauses by hour (predominance at night is expressed) A
B
Complete atrioventricular block (3rd degree AV block, complete transverse block)
is detected as a loss of connection between atrial (P wave) and ventricular contractions (QRS complex), while the atrial rhythm is more frequent than the ventricular one (Fig. 6). In such fragments one can see the layering of P waves on the ventricular QRS complexes, so the possibility of increasing the total voltage (and, accordingly, the amplitude of the P wave) is simply necessary.
Fig.6. 3rd degree AV block in patient Zh., 69 years old.
Often, against the background of 3rd degree AV block, replacement contractions or rhythms are recorded (Fig. 7).
Fig.7.
Patient G, 64 years old: replacement idioventricular rhythm against the background of 3rd degree AV block.
Quite often in patients, AV block occurs sporadically or its degree varies depending on the time of day. Rare episodes of 2nd degree AV block may also occur at night (usually in the early morning hours) with a normal PQ interval for the rest of the monitoring time. In addition, during follow-up of a patient with AV block, one can often see a progressive deterioration of AV conduction over several years (Fig. 8).
Fig.8.
Progressive deterioration of AV conduction in patient L., 45 years old: A – slowing of AV conduction was first detected at the age of 45 years; B – 2nd degree AV block type II at 46 years old; C and D – 2 consecutive episodes of 3rd degree AV block 3:2 and 5:2 with the formation of pauses of 2.31 and 5.34 seconds, respectively.
A
B
IN
G
Every novice doctor is faced with the difficulty of differential diagnosis between 2nd degree AV block type II and 3rd degree AV block. Only with a detailed comparison of the fragments and the use of the “ECG review” option can we conclude that there is a complete transverse blockade on the controversial fragment.
Blockades of the branches of the His bundle
A standard 12-channel resting ECG allows you to clearly diagnose variants of conduction disorders along the His system. During daily ECG monitoring, it is possible to identify transient blockades of the branches of the His bundle, which are recorded at night or, conversely, during intense physical activity. They are often an incidental diagnostic finding. However, such intraventricular conduction disturbances (for example, transient complete block of the left bundle branch) can mimic paroxysmal ventricular arrhythmias and lead to overdiagnosis of life-threatening arrhythmias (Fig. 9).
Fig.9.
Patient K., 72 years old: transient complete blockade of the left bundle branch. A – beginning of the blockade, B – end of the blockade.
A
B
As a rule, it is not difficult to differentiate conduction aberration along the His system from paroxysmal ventricular rhythm disturbances: the block is characterized by a regular regular rhythm, smooth regular cycles, the absence of a compensatory pause (or lengthening of the RR interval) at the end of a rhythm fragment from extended complexes and a smooth restoration of normal sinus rhythm .
None of the listed signs can be seen in Fig. 10, which allows us to qualify this fragment as ventricular tachycardia. Rice. 10. Patient K., 79 years old: paroxysm of unsustained ventricular tachycardia
In conclusion, I would like to note: for a clear diagnosis of conduction disorders, a single Holter recording is often not enough. If there are dubious changes suspicious for conduction disorders (especially at night), the study must be repeated with a total monitoring duration of up to 72 hours.
Moscow, 04/16/2009
Causes
Such changes most often occur due to structural changes in the heart muscle. This may be caused by one of the following diseases:
- various types of heart defects;
- ischemia;
- hemochromatosis;
- heart attack, cardiosclerosis and other heart ailments;
- pulmonary heart;
- thromboemolia of the pulmonary arteries;
- amyloidosis;
- poisoning with medications or exceeding recommended doses;
- hypertension.
In some cases, the cause of conduction disturbance may be one of the extracardiac factors:
- systemic connective tissue diseases;
- problems of water and electrolyte nature;
- congenital pathologies associated with the conductive function of the heart.
We should not forget about the characteristics of the body. According to statistics, every twentieth patient has a congenital conduction disorder in the right leg, which is the norm.
Symptoms
Complications in diagnosing the disease arise because the conduction disorder of the right bundle branch does not have any significant manifestations. The patient simply cannot detect this deviation on his own.
Most often, the disease is detected randomly during a routine ECG. However, the patient may have complaints such as pain in the heart, shortness of breath, interruptions in heart rhythm, and severe fatigue, which appear due to the progression of the underlying disease that caused the blockade.
If other sectors are affected, the following symptoms are possible:
- Signs of hemiblockade of the posterior or anterior left branch depend on the underlying disease. They are usually mild and involve heart pain, shortness of breath, and fatigue.
- Complete blockade of the left leg of the heart is manifested by dizziness, heart pain, and palpitations. The appearance of these symptoms can be caused by extensive changes in the left ventricle, including acute infarction.
- Three-fascicle blockade can be characterized by a complete absence of impulse conduction. Patients experience frequent dizziness, interruptions in heart function, and fainting. If adequate treatment is not carried out, various complications are possible, including a heart attack.
Bundle branch block
Bundle branch blocks do not have independent clinical manifestations; in most cases they are manifested by symptoms of the underlying disease and specific ECG changes. In some cases, with a decrease in cardiac output, bundle branch block may be accompanied by frequent dizziness, severe bradycardia, and sometimes attacks of loss of consciousness.
Let's consider the main clinical options for bundle branch block.
Right bundle branch block
In the case of complete blockade of the right bundle branch, impulse conduction and excitation of the myocardium of the right ventricle and the right half of the IVS occurs along contractile muscle fibers from the left ventricle and the left half of the IVS. With incomplete blockade, there is a slowdown in the conduction of the electrical impulse along the right bundle branch. Sometimes incomplete blockade of the right bundle branch is detected in practically healthy young people; in this case, it is regarded as a variant of the physiological norm.
ECG signs of complete blockade of the right bundle branch are the expansion of the S wave, an increase in amplitude and expansion of the R wave, the QRS complex has the form qRS with an expansion of up to 0.12 seconds. and more.
Left bundle branch block
With a complete block of the left bundle branch, the excitation wave is not conducted along the trunk of the leg until it branches or does not spread simultaneously to both branches of the left bundle (two-bundle block). The excitation wave is transmitted to the myocardium of the left ventricle with a delay from the right half of the IVS and the right ventricle along the Purkinje fibers. The ECG shows a deviation of the EOS to the left, widening of the QRS complex to 0.12 seconds. or more.
The blockade of the anterior branch of the left bundle branch is based on a violation of impulse conduction to the anterolateral wall of the left ventricular myocardium. In this case, after excitation of the IVS and the lower parts of the posterior wall along the anastomoses of the Purkinje fibers, the excitation wave propagates to the anterolateral wall of the left ventricle from bottom to top.
When the posterior branch of the left bundle branch is blocked, the conduction of impulses to the posteroinferior parts of the myocardium of the left ventricle is impaired. The activation wave spreads from the anterior and anterolateral wall of the left ventricle along the Purkinje fibers to the posteroinferior parts of the left ventricle, i.e., from top to bottom.
Incomplete blockade of the left bundle branch is characterized by a slowdown in impulse conduction along the main left trunk or along both branches of the left bundle. In this case, part of the myocardium of the left ventricle is excited by impulses propagating along the right leg.
Double bundle blockades
When a blockade of the right bundle branch is combined with a blockade of the left anterior branch, the electrical impulse propagates along the posterior branch of the left bundle branch, causing excitation first of the posteroinferior sections of the myocardium of the left ventricle, then of its anterolateral sections. Following this, the impulse slowly spreads along the contractile fibers to the myocardium of the right ventricle.
Delayed excitation of the anterolateral wall of the left ventricle and right ventricle is reflected on the ECG in the form of an expansion of the QRS complex to 0.12 seconds, jagged ascending limb of the S wave, a negative T wave, and deviation of the EOS to the left.
With a combined block of the right bundle branch with blockade of the posterior left branch, the impulse is carried out through the anterior left branch, the anterolateral sections of the myocardium of the left ventricle through anastomoses to the posteroinferior sections of the left ventricle, and then along the contractile fibers to the right ventricle. The ECG reflects signs of blockade of the left posterior branch and right bundle branch, deviation of the EOS to the right. This combination indicates widespread and profound changes in the myocardium.
Three-bundle blockade
Incomplete three-fascicular block is accompanied by the propagation of the excitation impulse to the ventricles along the least affected branch of the bundle branches. In this case, atrioventricular block of the first or second degree is noted.
In the case of a complete three-fascicular block, the conduction of impulses from the atria to the ventricles becomes impossible (III degree AV block), which leads to the separation of the atrial and ventricular rhythms. In this case, the ventricles contract in their own idioventricular rhythm, characterized by low frequency and arrhythmia, which can lead to the appearance of atrial fibrillation and asystole of varying duration.
The ECG picture with complete block of the bundle branches corresponds to signs of AV block of varying degrees.
Diagnostic features
Any conduction abnormality can be detected during electrocardiography. Based on the results of this procedure, the specialist determines further actions:
- If incomplete right blockade was detected in the absence of other cardiological diseases, then this can be attributed to the characteristics of the body. Additional research in this case is not prescribed.
- A detected two-fascicle blockade will require in-depth diagnostics. If this deviation has not previously been observed in the patient, then he needs urgent hospitalization, even if there are no complaints. If a complete left blockade exists for a long time, then hospital treatment is not required.
- If a three-fascicular block is detected in a patient, urgent hospitalization is necessary. Here, a full examination will be carried out in a short time to determine the further course of treatment.
Treatment methods
This pathology needs to be eliminated only if the patient has a disease that provoked the development of the blockade. In its absence, therapy is not carried out.
For patients suffering from single- or double-fascicular nonconduction, drug therapy is chosen, which involves taking the following drugs:
- antioxidants;
- vitamins;
- sedative herbal preparations;
- means for eliminating arterial hypertension;
- antibiotics;
- cardiac glycosides and diuretics.
The course of treatment is selected depending on the underlying disease and the stage of its development. In advanced cases, the blockage can be treated surgically. It involves installing a pacemaker for the patient.
AV block (atrioventricular block) - symptoms and treatment
Treatment of AV block depends on its degree and the presence of concomitant diseases.
In the case of 1st degree AV block, treatment of the underlying pathology that provoked the development of the block is indicated. All patients with this degree of conduction impairment should be monitored to ensure its progression. If intoxication with digitalis preparations (digoxin, strophanthin, corglycon) is detected, they should be discontinued. With increased tone of the parasympathetic nervous system, atropine must be prescribed. Ajmaline, quinidine, procainamide, beta-blockers and potassium should be avoided due to the risk of increasing the degree of AV block [2].
Second degree AV block (primarily type I) in the absence of symptoms and signs of acute cardiac pathology usually does not require active treatment, since there are no objective signs of circulatory disorders.
Special drug treatment is necessary for second degree AV block with slow heart function, causing circulatory disorders and various symptoms. Pharmacotherapy is also indicated in all cases of acute myocardial infarction. Treatment begins with the administration of atropine and isoprenaline, which increase the conduction of impulses in the His bundle. The exception is cases when, due to a very rare rhythm and impaired blood supply, urgent placement of an artificial pacemaker is necessary. Treatment with these drugs is carried out only by a doctor.
To determine treatment tactics, complete AV block can be divided into three groups:
1. Complete AV block without symptoms . No treatment required. This form occurs in a small group of people with congenital or acquired at a young age AV block with a ventricular contraction rate of 50-60 beats per minute. These patients should be monitored, visit a cardiologist and have an ECG done once every 6 months. If your condition worsens and complaints appear, you should definitely consult a doctor. If the ventricles contract less than 40 times per minute and the QRS complexes become wider, a permanent pacemaker should be installed, even in the absence of symptoms. This will help prevent sudden cardiac death.
2. Complete AV block with impaired circulation in the brain or heart . When cerebral circulation is impaired, fainting occurs. The main method of treatment is the installation of a pacemaker. Most doctors consider even a single faint to be an indication for its installation, since each attack may be the last and lead to the death of the patient. Drug therapy is carried out if the pacemaker is ineffective or during preparation for its use. The most suitable drugs are sympathomimetics - orciprenaline (alupent), isoprenaline (isoproterenol, proternol, saventrin). They cannot eliminate complete AV block, but they can increase the automaticity of the replacement ventricular center and maintain the ventricular contraction rate within 50-60 beats per minute. The dosage of the drug is selected individually for different periods of treatment.
Impaired cardiac circulation is associated with heart failure. If fainting is not observed, complete AV block is treated with digitalis and saluretics. To increase the frequency of ventricular contractions and minute volume, long-term therapy with isoprenaline, orciprenaline or ephedrine is indicated. If drug treatment does not improve heart failure, a pacemaker may be necessary.
3. Complete AV block of acute, transient form in case of fresh myocardial infarction, intoxication with cardiac glycosides, myocarditis, after heart surgery. Corticosteroids are an effective treatment for such blockade. They accelerate the resorption of edema and stop the process of inflammation in the area of the AV system. Hydrocortisone is administered intravenously, or prednisolone in tablet form is used.
The role of saluretics in the treatment of complete AV block is still being clarified. By influencing the excretion of salt from the body, they reduce the level of potassium in the serum by 1 mEq/L. This may improve AV conduction, increase the number of ventricular contractions, and stop or reduce the frequency of syncope. It is necessary to take saluretics for a long time, be sure to monitor the level of potassium in the blood.
The patient’s lifestyle and disease prognosis
If the patient does not have any heart disease, and the blockade of the right leg of the heart occurs in his body without complications, then he can lead a normal life with moderate physical activity. If the pathology is caused by another illness, the patient should limit stressful situations and loads, eliminate bad habits, and monitor nutrition.
If a pacemaker was installed during the operation, the patient should observe the following precautions:
- have with you the identification card of the owner of the pacemaker;
- protect the implantation area from the influence of a mobile phone or electrical appliances;
- undergo an ECG once a year (or more often if there is a special doctor’s order).
Since His bundle block is not an independent disease, but is a consequence of other ailments, the prognosis directly depends on the disease that provoked this pathology. Single-fascicle right blockade without significant heart damage does not pose a danger to human health.
If, as a result of a heart attack, the impulse of the left branch was blocked, then the prognosis is less favorable (mortality is up to 50% with exacerbation of the disease). Three-bundle pathology also has serious consequences, since against its background the likelihood of asystole increases.
The blockade of the His bundle itself is a feature of the body and cannot affect the patient’s quality of life. But with the development of concomitant diseases, the consequences of this pathology can be very dire. To avoid trouble, it is necessary to undergo systematic ECG examinations.
Diagnosis of cardiac conduction disorders (part 2)
intraventricular conduction Disorders of intraventricular conduction can be divided according to the level of damage into two groups - proximal and distal. The group of proximal disorders includes blockades resulting from conduction disturbances in the His bundle. The group of distal conduction disorders includes disorders that occur at the level of the left or right bundle branch and two branches of the left bundle (Fig. 14). 1. Right bundle branch block (RBBB). 2. Left bundle branch block (LBBB). 3. Block of the anterior branch of the left bundle branch (ALBBB). 4. Block of the posterior branch of the left bundle branch (LPBL). 5. Block of the right bundle branch in combination with blockade of the anterior branch of the left leg (double-bundle block: RBBB and RBBB). 6. Block of the right bundle branch in combination with a block of the posterior branch of the left bundle (two-bundle block: RBBB and BZVLBP). 7. Block of the left bundle branch in combination with blockade of the anterior branch of the left leg (double-bundle block: LBBB and LBBB). 8. Bilateral bundle branch block (LBBB and RBBB). 9. Three-bundle block (RBBB + BPVLNPG + BZVLNPG, RBBB + BPVLNPG + AV block I–II stages, RBBB + BPVLNPG + AV block I–II stages). 10. Arborization blockade. 3.4.1. Right bundle branch block (RBBB) is a conduction disorder along the right bundle branch, as a result of which excitation spreads in the usual way to the left ventricle and in a roundabout way, with a delay, to the right ventricle (Fig. 15). The ECG shows a widened, deformed QRS complex (more than 0.1 s), which in leads V1–V2, III, aVF has the form rsR', RSR', RsR', rR' (the R wave predominates in combination with the QRS). Depending on the width of the QRS complex, right bundle branch block can be complete or incomplete. 3.4.2. Left bundle branch block (LBBB) is a conduction disorder in the main trunk of the left bundle branch before it divides into two branches or simultaneous damage to two branches of the left bundle branch. Excitation spreads in the usual way to the right ventricle and in a roundabout way, with a delay, to the left ventricle (Fig. 16). The ECG shows a widened, deformed QRS complex (more than 0.1 s), which in leads V5–V6, I, aVL looks like rsR', RSR', RsR', rR' (the R wave predominates in the QRS complex). Depending on the width of the QRS complex, right bundle branch block can be complete or incomplete 3.4.3. Block of the anterior branch of the left bundle branch (LABLB, left anterior hemiblock, anterior left block, anterolateral block, left ventricular focal block, parietal block, atypical left bundle branch block, pronounced deviation of the EOS to the left, upper left intraventricular block, qRI–rSII–rSIII syndrome, syndrome S2–S3, abnormal left axis deviation, left anterior fascicular block) is a conduction disorder that occurs along the anterior branch of the left bundle branch (Fig. 17, 18). Blockade of the anterior branch of the left leg is identified by the deviation of the electrical axis of the heart: to the left (EOS from 0 to -30˚) - incomplete LPVP, or sharply to the left (EOS more than -30˚) - complete BPLP. 3.4.4. Block of the posterior branch of the left bundle branch (LPBL, left posterior hemiblock, left posterior focal block, peri-infarction diaphragmatic block, pronounced deviation of the EOS to the right, block of the left lower branch, abnormal right axis deviation, left posterior fascicular block) is a conduction disorder that occurs on along the posterior branch (Fig. 19, 20). Blockade of the posterior branch of the left leg is detected by the deviation of the electrical axis of the heart: to the right (EOS from +90 to +120˚) - incomplete LVLP, or sharply to the right (EOS more than +120˚) - complete BLBP. 3.4.5. Block of the septal branch of the left bundle branch. The septal branch is formed by part of the fibers of both branches of the LBP and provides impulses to the interventricular septum. ECG signs: absence of Q wave in leads V5–V6. Differential diagnosis 1. Intraventricular blocks (bundle branches, three-bundle). 3.4.6. Block of the right bundle branch in combination with a block of the anterior branch of the left leg (block of the right leg with left anterior hemiblock, block of the right leg with a strong deviation of the EOS to the left, block of the right leg of the Bailey type) is a two-bundle block with simultaneous damage to the right leg and the anterior branch of the left bundle branches (Fig. 21, 22). The ECG shows signs of RBBB (QRS complex more than 0.1 s, with a predominant R wave in leads V1–V2, III, aVF) in combination with signs of RBBB (deviation of the EOS to the left or sharply to the left). 3.4.7. Right bundle branch block in combination with left posterior branch block (right bundle block with left posterior hemiblock, classic right bundle branch block, rare type of right bundle branch block) is a two-bundle block with simultaneous damage to the right bundle and the posterior branch of the left bundle branch. The ECG shows signs of RBBB (QRS complex more than 0.1 s, with a predominant R wave in leads V1–V2, III, aVF) in combination with signs of RBBB (deviation of the EOS to the right or sharply to the right) (Fig. 23, 24). 3.4.8. Block of the left bundle branch in combination with block of the anterior branch of the left leg is a two-bundle block with simultaneous damage to the main trunk of the left leg and its anterior branch. A similar ECG picture occurs when incomplete blockade of the posterior branch is combined with complete blockade of the anterior branch of the left leg (Fig. 25). The ECG shows signs of LBBB (QRS complex more than 0.1 s, with a predominant R wave in leads V5–V6, I, aVL) in combination with signs of LBBB (deviation of the EOS to the left or sharply to the left). 3.4.9. Block of the left bundle branch in combination with a block of the posterior branch of the left leg is a two-bundle block with simultaneous damage to the main trunk of the left leg and its posterior branch. A similar ECG picture occurs when incomplete blockade of the anterior branch is combined with complete blockade of the posterior branch of the left leg (Fig. 26). The ECG shows signs of LBBB (QRS complex more than 0.1 s, with a predominant R wave in leads V5–V6, I, aVL) in combination with signs of LBBB (deviation of the EOS to the right or sharply to the right).
* Part 1, see RMJ. 2013, no. 4. pp. 237–240.