Of all birth defects, heart defects are the most common. This may be due to the earliest and most intense development of the cardiovascular system in the first weeks of pregnancy. Be that as it may, it is newborns and their parents who may subsequently need to undergo often life-saving surgical interventions.
Congenital heart defects (CHD) are organic disorders of the structures of the heart or adjacent vessels that are present from birth. The danger of defects lies in the fact that the blood circulation system can be seriously disrupted, both within the organ itself and throughout the pulmonary or systemic circulation.
Childhood mortality associated with congenital heart disease fell nearly 60% from 1987 to 2005, according to a study published in the September 2010 issue of the American College of Cardiology.
Most heart defects have no known cause. Despite this, today, thanks to successful modern prenatal care and cardiac surgery, many children with congenital heart disease can fully develop and move into adulthood. Still, the question of how long people live with congenital heart disease can be considered open. The answer to this most often depends on the severity and size of the defect itself.
Video: Congenital heart defect
What is heart disease
To understand what a heart defect is, you need to understand the basic anatomy of this organ and the principles of its operation.
The human heart consists of 4 chambers - 2 atria and 2 ventricles. Blood moves from one chamber to another through openings that have valves. From the left ventricle, blood is released into the systemic circulation (aorta), saturates all organs and tissues of our body with oxygen, and returns to the left atrium through the vena cava. From there it goes to the right ventricle, then to the pulmonary artery in order to be enriched with oxygen in the lungs, and through the pulmonary veins returns to the right atrium, then to the left ventricle. Then the cycle repeats.
To prevent mixing of arterial and venous blood inside the heart, the left and right sections are separated by partitions - interatrial and interventricular. To prevent blood from flowing back (from the ventricles to the atria or from the aorta to the left ventricle), there are valves that open and close at certain times.
All heart defects are divided into 2 types - congenital and acquired.
As the name implies, congenital defects appear in a person from his very birth, and acquired defects arise in the course of later life.
The incidence of congenital heart defects (CHD) is approximately 5-8 cases per 1000 children. Acquired heart defects (AHD) occur in 100-150 people per 100,000 population.
To make it easier to understand the differences between CHD and PPS, I note that with the former, an anomaly develops, deformation of the main vessels (aorta and pulmonary trunk) or a septal defect, and with acquired ones, the valves are affected. But such a division can be considered conditional, since the valves can be damaged even with congenital defects.
All this leads to disruption of hemodynamics (normal blood flow) inside the heart, predominance of blood supply to some chambers and depletion of others. As a result, arterial blood mixes with venous blood, certain chambers become filled with blood, stretch, and their walls thicken. The filling of other parts of the heart, on the contrary, decreases compared to normal.
Most people with heart disease receive a disability rating. They cannot live a full life, like all healthy people, they need to constantly observe some restrictions. Even purely psychologically it is difficult.
On the issue of the army - people with heart defects are classified as “unfit” or “limitedly fit” for military service.
Is it possible to die from pathology?
Unfortunately, death from heart disease is quite possible. The statistics of deaths from congenital heart disease are quite sad. Without timely medical intervention, it occurs in 70-80% of cases.
People with PPS die approximately 15-20% of the time. The main cause of death with heart defects is heart failure, i.e. deterioration of the main function of the “pump” - pumping blood.
Other causes of death include heart rhythm disturbances, such as paroxysmal ventricular tachycardia, atrial fibrillation, and atrioventricular block. Due to atrial fibrillation, thromboembolism often occurs in the brain, leading to stroke.
Answers to frequently asked questions
Is there accurate data on how many years people with congenital heart defects live?
As medical care and treatment for infants expands, patients with congenital heart disease live longer and healthier lives. Many children with congenital heart disease were able to transition into adulthood. It is estimated that more than two million people in the United States live with congenital heart disease.
Survival statistics:
- The survival of infants with congenital heart disease depends on how severe the defect is, when it is diagnosed, and how it is treated.
- About 97% of children born with non-critical congenital heart disease survive to one year of age, while 95% of children born with non-critical congenital heart disease survive to 18 years of age.
- About 75% of infants born with critical congenital heart disease survive to one year of age, while 69% of infants born with critical congenital heart disease survive to age 18. Thus, the population of people with congenital heart disease is increasing.
- Survival and medical care for children with critical congenital heart disease are improving. Between 1979 and 1993, about 67% of infants with critical congenital heart disease survived to one year. About 83% of children with critical congenital heart defects in the period from 1994 to 2005 were able to survive to the same age. [3 - Matthew E. Oster, Kyung A. Lee. Temporal Trends in Survival Among Infants With Critical Congenital Heart Defects. Pediatrics, May 2013.]
There are the following options for the development of congenital heart disease:
- Many people with uncomplicated forms of defects live without any problems.
- In other cases, the disease may develop over time.
- Some patients with congenital heart disease have genetic disorders or other health changes that increase the risk of disability or even death.
Even with improved treatment, many people with congenital heart disease are not completely cured, even if their heart defect has been repaired. With congenital heart disease, other health problems may develop over time. It all depends on the specific cardiac defect of the patient, the magnitude of the disorder and the severity of the pathology.
Against the background of congenital heart disease, even after treatment, various health problems may arise:
- irregular heart rhythm (arrhythmias);
- increased risk of infection of the heart muscle (infective endocarditis);
- weakening of the heart due to the development of cardiomyopathy.
The presence of congenital heart disease forces you to undergo regular examinations with a cardiologist, which allows you to maintain your health at an acceptable level. Repeat surgery may also be required at an older age, even after primary childhood surgery.
Possible causes
Among the causes of acquired defects, the most common are:
- Rheumatism, or more precisely, chronic rheumatic heart disease is an inflammation of its inner lining (including the valve apparatus), which develops after suffering (mainly in childhood) a streptococcal infection (tonsillitis).
- Infectious endocarditis is the gradual destruction of the heart valves due to the proliferation of bacteria on them. Infection can occur during the removal of a carious tooth, poor antiseptic treatment of the skin during an injection, or the use of unsterile syringes.
- Atherosclerosis and degenerative changes in valves are typical for older people.
More rare causes include syphilis and systemic pathologies - rheumatoid arthritis, lupus erythematosus, scleroderma.
The specific etiological factor of birth defects is difficult to determine. It can be:
- hereditary mutations – Down syndrome, Patau;
- maternal diseases - diabetes mellitus, thrombophilia, systemic vasculitis;
- intrauterine viral infections - rubella, cytomegalovirus, chickenpox;
- bad habits - smoking, drinking alcohol during pregnancy;
- exposure to ionizing radiation;
- the use of drugs that adversely affect fetal development - antitumor agents, sulfonamides, tetracyclines.
How to determine the presence of a heart defect
To find out whether a person has a heart defect, I focus on the following data:
- symptoms and complaints bothering the patient;
- physical status – the appearance of the patient;
- electrocardiography;
- echocardiography (ultrasound of the heart);
- X-ray of the chest organs.
Symptoms, signs and typical appearance of the patient
People with heart defects mainly suffer from symptoms of heart failure. They experience difficulty breathing, especially at night, which is associated with a horizontal position of the body and increased pressure in the vessels of the lungs. For the same reasons, they may be bothered by paroxysmal cough.
Patients (especially with congenital heart disease) get tired very quickly, even after very little physical activity, they constantly want to sleep, they feel dizzy, and they may even faint.
Due to the enlarged liver, the patient feels heaviness or nagging/aching pain in the right hypochondrium. By evening my legs swell very much. Often bothered by aching pain in the left side of the chest, palpitations, and discomfort in the chest. Patients with certain congenital heart diseases regularly experience lower respiratory tract infections.
I often notice the so-called “drumstick symptom” in people with heart defects. This is a thickening of the terminal phalanges of the fingers. This sign indicates a long-term circulatory disorder throughout the body.
Newborns and infants with congenital heart disease are stunted and have reduced body weight. Often their lips, nose, and fingertips become bluish (cyanosis).
There are specific symptoms of heart disease. For example, with coarctation of the aorta, due to its pronounced narrowing, the blood circulation of the head, arms and upper body remains at the proper level, while the lower parts of the body and legs are depleted of blood. This leads to the fact that the muscles of the upper shoulder girdle stand out against the background of the underdeveloped muscles of the lower extremities. And a false impression of an “athletic physique” is created.
Another example is mitral stenosis. In the later stages of this PPS, against the background of general pallor of the face, a bright bluish-pink blush appears on the cheeks, while the lips and nose have a blue tint. This is called "facies mitralis", or "mitral face".
I would like to note that a person with PPS can feel quite healthy for a long time and not experience any pain or difficulty breathing. This is due to the fact that the heart tries to compensate for hemodynamic disturbances and at first copes well with this. However, sooner or later these mechanisms are not enough, and the disease begins to manifest itself clinically.
When I examine such patients, I am able to identify some pathological signs, for example, an increased cardiac impulse of the left or right ventricle, trembling of the chest. During auscultation of patients with heart disease, I often hear murmurs at the projection points of the valves, septa and carotid arteries; strengthening, weakening or splitting tones.
Instrumental diagnostics
Basic instrumental research methods for diagnosing heart defects:
- Electrocardiography. On the ECG, I can see signs of hypertrophy of different parts of the heart by changes in the height, width and shape of the teeth. Arrhythmias are often detected (atrial fibrillation is especially common).
- Echocardiography is perhaps the main diagnostic method that allows one to reliably establish a heart defect. Echo-CG clearly identifies the condition of the valves, septa, wall thickness and chamber volume. In Doppler mode, you can see the direction of blood flow between sections (regurgitation) and measure the pressure in the pulmonary artery. If a defect is suspected, I prescribe a transesophageal echocardiogram (a sensor is installed in the esophagus directly behind the heart) to obtain a more detailed image.
- X-ray of the chest organs - the image clearly shows the bulging of the pulmonary artery trunk, increased pulmonary pattern due to increased pressure in the vessels of the lungs, changes in the shape of the heart shadow, usuration of the ribs (uneven contour due to compression of them by the intercostal arteries).
Types of defects and their differences
As already mentioned, all heart defects are divided into congenital and acquired. They differ from each other in pathophysiology, severity, and human life expectancy.
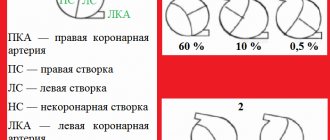
There are many classifications of congenital heart disease, but most often clinicians use the Marder classification, which divides all congenital heart disease into defects with cyanosis and without cyanosis (i.e., “blue” and “white”).
Table 1. Characteristics of congenital heart disease
| Type | Name | Highlighting feature | Mechanism of hemodynamic disturbance |
| CHD without cyanosis (pale type) | Defects of the interventricular and interatrial septa | “Cardiac hump” (protrusion of the anterior chest wall) due to severe enlargement of the pancreas. Intense systolic murmur in the III-IV intercostal space to the left of the sternum | Discharge of blood from left to right. Overload of the left ventricle, then the right parts of the heart. Rapid development of pulmonary hypertension due to reflex spasm of the pulmonary arteries |
| Patent ductus arteriosus | Systole-diastolic murmur in the II-III intercostal space to the left of the sternum | Discharge of blood from the aorta into the pulmonary artery, increased blood flow in the pulmonary circle, overload of the left parts of the heart | |
| Isolated pulmonary stenosis | Weakening of the second tone and rough systolic murmur over the pulmonary valve | Sharp overload of the pancreas, depletion of pulmonary blood flow | |
| Coarctation of the aorta | High blood pressure, “athletic physique”, “chillness of the legs”, weakening or pulsation in the arteries of the lower extremities, Usuration of the ribs on the radiograph, systolic murmur along the entire left sternal border | Obstruction of blood flow through a narrowed section of the aorta, LV overload | |
| CHD with cyanosis (blue type) | Transposition of the great vessels | Severe general hypoxia (cyanosis, “drumsticks”), cardiac hump, loud first sound at the apex | Lack of oxygen in the organs through which the large circulation passes. |
| The only ventricle of the heart | Signs of hypoxia, systolic murmur at the apex | Mixing of arterial and venous blood, increased pulmonary blood flow, rapid overload of the ventricle | |
| Tetralogy of Fallot | Sharp weakening of the second tone over the pulmonary artery | Discharge of blood from right to left |
Acquired heart defects are divided into 2 types - stenosis, i.e. narrowing of the opening between the chambers, and insufficiency, i.e. incomplete valve closure. All PPS come down to the overflow of blood in some chambers of the heart and depletion of others, with all the ensuing consequences.
The most common PPS in adults is aortic stenosis (about 80%).
Combined defects can occur - when a person simultaneously has both insufficiency and valve stenosis. I also quite often see people who have multiple valves affected. This is called a combined heart defect.
Table 2. Characteristics of teaching staff
| Type | Name | Highlighting feature | Mechanism of hemodynamic disturbance |
| Mitral valve defects (MV) | MK deficiency | Weakening of the first tone, systolic murmur at the apex | Reverse discharge of blood into the left atrium |
| Mitral stenosis | Loud first sound, diastolic murmur at the apex. Facies mitralis. | Severe overload of the left atrium, its hypertrophy and expansion. Increased pressure in the pulmonary vessels due to reflex spasm | |
| Aortic valve defects (AV) | AC deficiency | Increased pulse blood pressure, visible pulsation of the carotid arteries, protodiastolic murmur on the AC | Distension of the left ventricle by reverse flow of blood from the aorta |
| Aortic stenosis | Pain resembling angina pectoris, constant fainting. Rough systolic murmur on the AC, extending to the carotid arteries | Deterioration of blood ejection into the aorta, left ventricular overload | |
| Pulmonary valve defects (PA) | LA insufficiency | Weakening of the second sound on the pulmonary valve, protodiastolic murmur in the second intercostal space to the left of the sternum | Backflow of blood into the right ventricle |
| PA stenosis | Strengthening and splitting the second tone. Pronounced pulsation of the right ventricle | Obstruction of blood ejection into the PA, overload of the RV | |
| Tricuspid valve defects (TC) | TC deficiency | Systolic murmur on TC | Reverse discharge of blood into the right atrium |
| TC stenosis | Strengthening the first tone on TC | Overload of the right atrium, its expansion and hypertrophy |
Department of surgical treatment of congenital heart defects (CHD)
Congenital heart defects (CHD) are a large group of anomalies of the intrauterine development of the heart and large vessels flowing into or leaving its cavities, varied in formation and anatomy.
CHD incidence statistics
According to various sources, the incidence of congenital heart disease varies from 2 to 15 cases for every 1000 newborns. In 2021, among more than 1.3 million newborns, about 12 thousand children with congenital heart disease were registered.
Compared to statistics 10 years ago, the frequency of detection of congenital heart disease in newborns has increased from 6 to 9 cases per every 1000 infants born, which is apparently due to improved means of early diagnosis of this serious and often life-threatening group of diseases in childhood.
Despite the fact that modern methods and technical capabilities of ultrasound examination (echocardiography) will make it possible to detect congenital heart disease in the fetus starting from 12-14 weeks of pregnancy with a high degree of probability (up to 96%), nevertheless, cases of late detection of this pathology are recorded both among children, as well as among adults.
At the end of 2021, more than 573 thousand patients (children and adults) with an established diagnosis of congenital heart disease were registered in Russia (population of about 147 million people). However, there is a high probability that the actual number of such patients may be higher, and the number of annually registered cases of this diagnosis will increase.
Survival prognosis
Undoubtedly, the natural (without medical intervention) course of the vast majority of various congenital heart diseases, as a rule, has an unfavorable prognosis and leads to a reduction in the duration and quality of life of the patient, often quite significantly. Up to 90% of newborns with so-called “critical congenital heart disease” do not survive beyond 1 year. Many of them die within the first weeks of their lives. According to statistics, congenital heart defects account for about 10% of the causes of infant mortality in Russia.
Causes of congenital heart disease
Among the most likely causes of the formation of congenital heart disease are genetic and chromosomal aberrations, viral infections of the mother during pregnancy, chronic endocrine and metabolic diseases, bad habits (smoking, drinking alcohol, etc.), teratogenic and mutagenic adverse environmental factors.
There are a great many congenital anomalies of the development of the heart and great vessels. Conventionally, the entire set of congenital heart disease can be subdivided depending on the age at which clinical manifestations (symptoms and consequences) are most pronounced and prognostically significant.
| Types of congenital heart disease | Age at which surgical treatment is usually necessary |
| Newborn period |
| First year of life |
| Over a year old |
Some congenital heart diseases are characterized by severe disturbances of central hemodynamics soon after birth, forcing surgical treatment to begin already in the neonatal period (for example, simple transposition of the great arteries or obstructive forms of total anomalous drainage of the pulmonary veins).
Transposition of the great arteries
Total anomalous pulmonary venous drainage
Other congenital heart defects occur with clinical compensation in the first few weeks or months of life, manifesting closer to the second half of life (ventricular or aortic-pulmonary septal defect, atrioventricular canal, SBUG).
Common atrioventricular canal
Ventricular septal defect
Common truncus arteriosus
There are congenital anomalies that do not appear clinically for a long time and are benign, which makes it possible to delay their surgical treatment until the second year of life and even later (atrial septal defect, partial anomalous drainage of the pulmonary veins).
Atrial septal defect
Moreover, there are a number of congenital heart defects, the correction of which is advisable to delay within the duration of the clinical compensation period in order to achieve better treatment results (corrected transposition of the great arteries, compensated forms of Ebstein's anomaly, moderate coarctation of the aorta).
Coarctation of the aorta
It should also be noted that the same nosological form of congenital heart disease, depending on the specific anatomy, can become a reason for surgery at different age periods. For example, a simple transposition of the great arteries forces an arterial switch operation to be performed in the first two weeks of life, whereas in combination with a large ventricular septal defect, the same anomaly can be operated on at the age of two months or older. Extreme forms of Ebstein's anomaly with hemodynamic atresia of the pulmonary artery and ductus-dependent pulmonary blood flow are “critical congenital heart disease of the newborn period.”
“Critical defects of the newborn period” account for about 30% of identified congenital heart defects and require immediate surgical care in the first weeks, or even days, of a child’s life.
Previously, this group of diseases was identified with a pathology incompatible with life. However, the capabilities of modern medicine have made it possible to achieve impressive early and long-term results in the treatment of many of this group of congenital heart diseases.
Critical UPS
Hypoplastic left heart syndrome
Pulmonary valve atresia
Tricuspid valve atresia
It is important to remember that a number of congenital heart abnormalities cannot be eliminated immediately, within the framework of one surgical operation. In such cases, to achieve optimal treatment results, it is divided into several stages, or phases, each of which is performed at different ages, starting from infancy. Also, it is almost never possible to exclude the possible need to perform additional surgical intervention even after a previously performed radical (that is, definitive) correction of a heart defect.
All operations for congenital heart disease can be divided into 4 categories:
| Radical operations (corrections) | When complete and final elimination of congenital heart disease is achieved and the child’s heart acquires an anatomical structure corresponding to a healthy heart or close to normal anatomy. Intracardiac circulation after such operations naturally becomes physiological (that is, normal). After treatment, the patient’s rate of development, quality and life expectancy does not differ from healthy peers and usually only needs preventive outpatient monitoring. As a rule, disability is removed. |
| Hemodynamic corrections | When the intracardiac circulation, as well as the anatomical structure of the heart, upon completion of treatment cannot be called “corresponding to a healthy heart.” However, such a correction ensures hemodynamics close to physiological, allowing the child to live, develop, and in the future, successfully adapt to society and create his own family. A person’s physical capabilities may be somewhat limited, but the disability is not completely removed. |
| Preparatory (intermediate) palliative operations | They are interventions that aim to prepare the heart and the body as a whole for subsequent radical or hemodynamic correction. There may be several such operations. Patients after such operations can be temporarily discharged from the hospital, but require systematic outpatient monitoring in order to monitor the clinical condition, correct drug therapy and determine the timing of the next hospitalization for diagnosis and continuation of surgical treatment |
| Definitive palliative (life-prolonging) operations | Currently, they are very rare and are performed on patients with incurable (inoperable) complex forms of cardiac anomalies or their incurable complications. Such operations are sometimes called a “bridge” to heart transplantation. |
From a prognostic point of view, all congenital heart defects can be divided into anomalies with a favorable prognosis and defects with an unfavorable prognosis.
. The latter most often represent a combination of multiple congenital heart defects (often combined with malformations of other organs, multiple manifestations of dysembryogenesis and syndromic forms of genetic anomalies), which are not subject to radical correction and predetermine, even if hemodynamic or palliative surgery is performed, a low quality of the patient’s future life, limitation of its duration, deep disability and limited social adaptation. Patients with such anomalies are potentially considered candidates for heart or heart-lung transplantation. In cases of early prenatal (intrauterine) diagnosis of congenital heart disease with an unfavorable prognosis, the possibility of terminating the pregnancy for medical reasons should be considered in connection with the detection of a congenital heart defect incompatible with life in the fetus.
Classification of congenital heart disease
CHD can also be classified into simple (the patient has a single anomaly) and complex (a combination of several anomalies). In the WHO International Classification of Diseases, some frequently combined anomalies of heart formation are often combined into one nosological unit with appropriate coding, for example, “hypoplastic left heart syndrome” or “tetralogy of Fallot.”
Tetralogy of Fallot
Clinical manifestations (symptoms) of congenital heart disease
are not only very diverse, but also have a characteristic spectrum inherent in a specific age period of their natural course. For example, a large ventricular septal defect usually does not cause symptoms in the first few months of life due to the physiology of the lungs in newborns and infants. By six months of life, the child develops symptoms of heart failure (frequent colds, poor appetite, decreased exercise tolerance, shortness of breath, underweight, anemia, sleep disturbances) caused by excess blood flow in the lungs and overload of the left chambers of the heart. However, later, by 2-3 years of age and older, as irreversible dangerous sclerotic changes develop in the small vessels of the lungs, these symptoms spontaneously regress - a period of imaginary well-being begins. During this period, the patient is either conditionally operable or not operable at all. Subsequently, the clinical picture is characterized by symptoms of right ventricular circulatory failure and secondary deficiency of pulmonary blood flow against the background of sclerosis and obstruction of small vessels of the lungs.
Division of defects into “pale” and “blue” (cyanotic)
, widespread in popular scientific literature and online resources, is very conditional in nature, since it does not have a clear correlation with the hemodynamic patterns of the natural course of congenital heart disease and does not carry any prognostic value. Thus, two anomalies “simple transposition of the great arteries” and hypoplastic right heart syndrome are cyanotic congenital heart disease, but in the first case the possibility of radical correction predetermines a favorable prognosis, in contrast to the second of these congenital heart disease.
Congenital heart disease in adult patients is included in a special group
— corrected or uncorrected congenital heart disease in persons 18 years of age and older.
They are usually divided into primary and secondary. Primary
- a set of anomalies with a relatively favorable natural course, allowing one to survive childhood, first identified at the age of over 18 years or identified in childhood, but recognized as incurable (incurable).
This is a smaller cohort of patients. Secondary
– in the so-called “GUCH-patients” (the larger of the two cohorts). They are represented by a wide range of congenital heart anomalies previously operated on in childhood.
On the basis of the clinical departments of our Center, specialized in the treatment of patients with congenital heart disease, all types of open surgical, minimally invasive surgical (thoracoscopic) and X-ray endovascular interventions (including hybrid) are performed for a wide variety of congenital anomalies and tumor diseases of the heart and great vessels .
The center is equipped with all the necessary modern equipment for timely and complete diagnosis of congenital heart disease, including prenatal (intrauterine) diagnostics. Every year, about 3,500 patients with congenital heart disease receive the necessary surgical care at our Center. More than 900 X-ray endovascular procedures are performed for congenital anomalies of the heart and great vessels.
How are heart defects treated?
Unfortunately, there is no medicine that can cure a person from heart disease. And all congenital heart disease can only be treated surgically. An exception is the patent ductus arteriosus, a congenital defect that can be completely eliminated pharmacologically. But this is effective only in the first day of a person’s life. To do this, I prescribe intravenous administration of a non-steroidal anti-inflammatory drug (Ibuprofen, Indomethacin) for 3 days.
If cyanosis and signs of severe heart failure are present, surgery is performed immediately. Often, surgeons even have to operate on infants and one-year-old children. If the defect was discovered by instrumental examination methods, and the patient is not worried about anything, or there are minor symptoms, the operation can be postponed.
Traditionally, surgical interventions to eliminate congenital heart disease are performed under general anesthesia, on an open heart, with connection to a heart-lung machine. The defect is either sutured or covered with a patch of pericardium or synthetic tissue. The open duct is ligated or divided.
Recently, in specialized cardiology centers with appropriate equipment, it has been possible to perform minimally invasive endovascular interventions. In such operations, under ultrasound and X-ray guidance, a catheter is inserted through the femoral vein and reaches the right atrium. An occluder is inserted through the catheter, which consists of connected disks of nickel-titanium wire. This occluder closes the defect.
The main contraindication to such operations is advanced pulmonary hypertension with severe vascular sclerosis. In these cases, so-called palliative interventions are performed, which eliminate not the defect itself, but its consequences. Communications (anastomoses) are artificially created between large vessels so that blood flows bypassing the overloaded parts of the heart.
Now let's look at the treatment of acquired defects. Things are a little different with them.
If PPS developed against the background of rheumatism, then, according to the protocol, I always use antibacterial therapy with penicillin antibiotics. This point is very important, since the presence of streptococcal bacteria in the body can cause the development of new heart defects.
I also always prescribe drug therapy that will help stabilize the patient’s condition.
First of all, medications are used to slow the progression of heart failure:
- ACE inhibitors – Perindopril, Ramipril;
- beta blockers – Bisoprolol, Metoprolol;
- diuretics - Torasemide;
- aldosterone antagonists – Spironolactone, Eplerenone;
In case of heart rhythm disturbances, I use antiarrhythmic drugs - Sotalol, Amiodarone.
It is important to carry out anticoagulant therapy, since some of the PPS, especially mitral stenosis, are often accompanied by atrial fibrillation, in which blood clots form in the cavity of the left atrium, leading to cardioembolic stroke. To prevent this, I prescribe Warfarin or low molecular weight heparins.
When the patient’s condition is serious, when medications no longer help, I refer patients for surgical treatment.
There are 2 main types of operations for PPP:
- valve replacement;
- reconstructive operations - valve repair, commissurotomy, balloon valvotomy.
Valve prostheses can be mechanical (artificial) or biological. Their key difference is as follows. When installing a biological valve, the patient must receive anticoagulant therapy for the first 3 months after surgery, and when implanting a mechanical valve, for life. The question of choosing the type of valve is decided on an individual basis each time.
The only anticoagulant approved for long-term use with an artificial heart valve is Warfarin.
Mechanical valves are more durable, but their cost is much higher compared to biological ones.
Treatment of acquired heart defects can be conservative or surgical
Conservative treatment is effective only in the early stages of the development of heart disease and requires mandatory follow-up by a cardiologist.
PPS should be treated surgically when:
- Heart failure progresses.
- Pathological changes in the valve significantly affect hemodynamics.
- The ongoing conservative therapy does not have the desired effect.
- And there are fears of serious complications.
Types of operations for heart defects
Open heart surgery is performed under artificial circulation through a median sternotomy. Median sternotomy creates optimal conditions for the cardiac surgeon to perform the necessary surgical interventions for various pathologies and to connect the heart-lung machine. The soft tissue incision is approximately equal in length to the length of the sternum (about 20 cm), and the sternum is dissected along its entire length.
The main two types of operations that are currently used for PPS are reconstruction of the affected valves (plastic) or their prosthetics.
Valve-sparing surgery
Performed to eliminate the cause of valve dysfunction.
If the valves do not close (valve insufficiency), then the cardiac surgeon during the operation achieves normalization of the closure of the valve leaflets, performing resection of the valve leaflets, annuloplasty, commissural plastic surgery, and chord replacement. If there is valve stenosis, then the sections of the valves that have fused due to a pathological process are separated and an open commissurotomy is performed.
Valve replacement surgery
If it is impossible to perform plastic surgery, when there are no conditions for this, valve replacement operations for prosthetic heart valves are performed. In case of intervention on the mitral valve, replacement is performed with full or partial preservation of the anterior or posterior valve leaflets, and if impossible, without their preservation.
In valve replacement surgeries, prostheses are used.
- Prosthetics can be made from animal or human tissue. Such prostheses are called biological. Its main advantage is that the patient does not need to take anticoagulant drugs during subsequent years of life, and their main disadvantage is their limited service life (10-15 years).
- Prostheses consisting entirely of mechanical elements (titanium and pyrolytic carbon) are called mechanical. They are very reliable and can serve without failure for many years, without replacement, but after such an operation the patient must always take anticoagulants for life, this is a negative aspect of using a mechanical prosthesis.
Minimally invasive surgeries
Modern surgery, thanks to the creation of new instruments, has the opportunity to modify surgical approaches to the heart, which leads to operations becoming minimally traumatic for the patient.
The point of such operations is that access to the heart is carried out through small incisions in the skin. During minimally invasive operations on the mitral valve, a right-sided lateral minithoracotomy is performed, with a skin incision of no more than 5 cm, this allows one to completely avoid dissecting the sternum and provides convenient access to the heart. To improve visualization, endoscopic video support with multiple magnification is used. With minimally invasive access to the aortic valve, the skin incision is approximately half as large (incision length 8 cm), and the sternum is incised lengthwise in its upper part. The advantage of this method is that the uncut portion of the sternum provides greater stability after surgery, as well as a better cosmetic effect by reducing the size of the suture.
Endovascular operations - transcatheter aortic valve replacement (TAVI).
Methods of transcatheter aortic valve implantation:
- The entire operation is carried out through a blood vessel (femoral or subclavian artery). The meaning of the procedure is to puncture the femoral or subclavian artery with a guide catheter and deliver the stent valve against the blood flow to the site of its implantation (aortic root).
- Through the aorta. The essence of the method is to dissect the sternum over a short distance (ministernotomy) and puncture the aortic wall in the ascending section and implantation of a stent valve into the aortic root. The method is used when it is impossible to deliver the valve through the femoral and subclavian arteries, as well as when there is a pronounced bend in the arterial arch.
- Through the apex of the heart. The meaning of the procedure is to make a small incision in the fifth intercostal space on the left (minithoracotomy), puncture the apex of the heart with a guide catheter and install a stent valve. Once the new valve is implanted, the catheter is removed. The new valve starts working immediately.
There are two types of stent valves:
- Self-expanding stent-valve expands to the desired size after removing the restrictive sleeve sleeve from it.
- A balloon-dilatable stent valve that expands to the desired size when the balloon is inflated; After final installation of the stent valve, the balloon is deflated and removed.
To determine whether TAVI surgery is appropriate, the patient must undergo a series of tests, including an ECG, echocardiography, computed tomography (CT) scan, and angiography.
Currently, the TAVI procedure is increasingly used not only for aortic stenosis, but also for aortic insufficiency, as well as their combination. In addition, TAVI surgery is used for dysfunction of the biological prosthetic aortic valve.
TAVI surgery is performed under general anesthesia and requires a multidisciplinary approach. The procedure is performed by a specialized team, which includes an interventional cardiologist, cardiac surgeon, anesthesiologist, and radiologist.
The presence of a stent valve is not an indication for the patient to take the indirect anticoagulant Warfarin (in the absence of other indications).
What does the prognosis depend on: how long do patients live?
I am often asked: “How long do people live with heart disease?”
This depends on many factors such as:
- type of defect;
- its heaviness;
- degree of heart failure;
- presence of complications;
- timeliness of diagnosis and treatment;
- following the doctor’s recommendations (correctly taking medications in compliance with all dosages, etc.);
- the quality of the operation performed.
Without surgical intervention, patients with many congenital heart diseases die in early childhood (up to 2-5 years). CHDs in which a person can live to adulthood without surgery include coarctation of the aorta and atrial septal defect.
The most favorable PPS in terms of prognosis are mitral and tricuspid regurgitation. Serious complications develop rarely and over a long period of time. With other PPS (mitral, aortic stenosis), patients die approximately 5-10 years after the first onset of symptoms.
Modern treatment options, both pharmacological and cardiac surgery, make it possible to extend the life of such people to 60-70 years.
Symptoms of heart failure
In the clinical picture of the disease, there are general symptoms and specific ones, determined by the anatomical location of the defect. Common symptoms include:
- weakness and decreased ability to work;
- dizziness and fainting;
- shortness of breath and cyanosis (blue discoloration) of the skin;
- feeling of heartbeat;
- increase or decrease in blood pressure.
All these signs are the first signals and can only indirectly indicate the presence of heart disease.
Consequences of pathology
A patient with a heart defect, both congenital and acquired, has a high risk of developing acute heart failure (pulmonary edema, cardiogenic shock), which without prompt medical intervention leads to death.
Also, people with heart defects develop coronary disease much earlier, which means they are several times more likely to have a myocardial infarction.
Almost any heart defect is accompanied by rhythm disturbances. The most dangerous of them are ventricular tachyarrhythmias and atrioventricular block.
With some defects, due to severe overload of the pulmonary circulation and reflex narrowing of the pulmonary vessels, pulmonary hypertension occurs - a very serious condition, difficult to respond to drug therapy, requiring surgical intervention.
Due to prolonged severe oxygen starvation (hypoxia) of the whole body, the immune system suffers, which is why patients with heart defects constantly suffer from infectious diseases, especially bronchitis and pneumonia.
With any heart defect, as well as the presence of prosthetic valves, the risk of infectious (bacterial) endocarditis increases several times - a dangerous disease that affects the heart valves, often ending in death.
Classification
There are combined, complex and simple structural cardiac disorders. According to the level of oxygen starvation - white (pale) and blue. According to the classification information of the Association of New York Cardiac Surgeons, there are 4 classes of complexity:
- First . There are no serious anatomical changes in the myocardium; surgical intervention is not recommended.
- Second . The pathology is not advanced, the processes are reversible. Thanks to surgery, 100% recovery is possible. The systems and organs (except the heart muscle) are not damaged against the background of the defect.
- Third . Irreversible cardiac defects are observed. Pathological changes in the body caused by deformities are reversible.
- Fourth . The most dangerous class, often leading to death. All violations are irreversible.
Is surgery necessary for heart defects? What medications should I take and what should I not do? Only the attending physician can give answers to all these questions. There is no point in looking for an answer on the Internet. To cope with the problem and find an exceptionally error-free solution, make an appointment with a qualified cardiologist.
Case study: a teenager with coarctation of the aorta
Let me give you one interesting case from my practice.
A mother came to see me with her 15-year-old son, who has been troubled by headaches, chilliness and strange weakness in his legs since early childhood. At the age of 7 years, the boy was in the hospital in the pediatric department, where he was diagnosed with high blood pressure up to 150/90 mm Hg. A diagnosis was made: “Hypertension”, medications were prescribed. The patient took medications irregularly. The young age of the patient, as well as the absence of hypertension in the mother and father, made me doubt the diagnosis and suspect the “secondary nature” of high blood pressure. During a general examination of the patient, in addition to elevated blood pressure (155/90 mm Hg), I was able to detect weakened pulsation in the arteries of the legs and a systolic murmur at the back at the level of the lower angle of the scapula. I ordered an echocardiogram, which showed thickening of the left ventricle and an area of narrowing in the thoracic aorta. The radiograph clearly showed another sign of coarctation of the aorta – rib usuration (uneven contour). The patient underwent surgery - plastic surgery of a narrowed section of the aorta. The boy's condition improved, blood pressure returned to normal, and the need to take medications to correct blood pressure disappeared.
Expert advice: living with heart disease
I would like to give a few recommendations that will help avoid most of the negative consequences and increase the effectiveness of treatment:
- sports – professional training will have to be stopped. Minor physical activity is allowed;
- Regular examination - it doesn’t matter whether you were successfully operated on as a child or have only recently been diagnosed with mild mitral regurgitation. In case of heart disease, it is necessary to visit a cardiologist at least once every six months to a year, do an ECG and Echo-CG to check the state of heart function, as well as to monitor the occurrence of possible complications;
- table salt - if you have been diagnosed with signs of chronic heart failure and you have been prescribed medications for its treatment, for greater effectiveness you need to limit the use of table salt with food to 2-3 grams per day;
- Warfarin – This drug is often prescribed to patients with heart defects to prevent blood clots. In order for its use to be effective and at the same time safe, you need to regularly do a blood test (coagulogram). The INR in this study should be greater than 2 but less than 3;
- a visit to an otolaryngologist - if you have been diagnosed with PPS of rheumatic origin, be sure to go for a consultation with an ENT doctor, since the main cause of rheumatism is tonsillitis (tonsillitis). In the presence of chronic tonsillitis, treatment of the tonsils (washing, antibiotics) is necessary, and possibly their removal. This is necessary to prevent relapse of rheumatism and the appearance of a new heart defect.
- prevention of infective endocarditis - all people with heart defects and prosthetic valves have an increased risk of developing infective endocarditis. Therefore, to prevent it, they must take penicillin antibiotics (Amoxicillin, Ampicillin) once, approximately 30 minutes/1 hour before medical procedures (tooth extraction, bronchoscopy, cystoscopy, etc.).
Prevention
A healthy lifestyle is the main option for preventing rheumatic heart disease and other types of cardiac defects. Thanks to proper nutrition, an even distribution of physical activity, and the absence of stress, you can strengthen the immune system and increase the regenerative capabilities of the body, especially in the case of traumatic injuries. Cardiologists advise:
- Eat only healthy food, do not forget about vitamins, important microelements, add more fresh fruits, vegetables, low-fat fish and herbs (dill, cilantro, parsley, onions, lettuce) to your diet.
- Monitor your blood pressure, constantly use a tonometer, and if your condition worsens, take medications prescribed by your cardiologist.
- Avoid depressive disorders and stressful situations. It is important to create coziness and comfort around you from a psychological point of view, not to get nervous about little things, to devote more time to hobbies, to communicate with pleasant people and friends.
- Monitor your health and well-being, monitor the activity of organs and systems of the body, monitor the behavior of the thyroid gland, liver, and symptoms characteristic of these organs.
Prevention of the development of major heart defects, which are considered congenital, depends on the future parents. During the planning period, during conception, in the first trimester of pregnancy, it is important that the expectant mother:
- I gave up bad habits, smoking, drinking alcohol, and taking drugs.
- She was examined for infections, or more precisely for herpes and cytomegalovirus.
- I did not get vaccinated during pregnancy, but took care of the prevention of rubella, chicken pox, measles, polio and mumps in advance.
It is strictly forbidden to take medications that can harm the fetus. If you use tablets, drops, syrups, sprays, check whether you can continue to do this when planning a child or becoming pregnant.