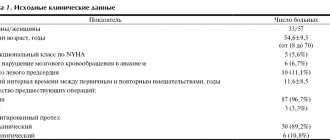
Patient Information
- CELL TRANSPLANTATION: real achievements and opportunities for clinical application
- Choosing a prosthesis in Russian conditions
- Coronary artery bypass surgery without artificial circulation - what should be considered when choosing a clinic to perform it?
- “With a whip of a butt... you’ll kill it!”, or the truth about coronary artery bypass grafting and stenting
- Delays in issuing clopidogrel prescriptions to patients after stenting are a common and deadly problem.
The traditional type of surgical treatment of damaged heart valves in our country and abroad is their replacement with various prostheses.
At the early stage of the development of cardiac surgery, doctors tried to use valve devices based on biological tissues of xenogeneic (i.e., borrowed from animals) or allogeneic (homogeneous) (i.e., borrowed from humans) origin as replacement material. The main disadvantage of these devices is the limited service life of the valve due to the gradual destructive effect on biological tissues from the recipient's body. Since in those years (60-70) any heart surgery was perceived as a difficult test for the patient (and also for the surgeon), the primary task was to develop a type of prosthesis, the implantation of which would be final in the surgical treatment of valve disease. Bioprostheses clearly did not meet this condition. The search began for materials and models for creating synthetic, mechanical prostheses. More than several dozen models have been created, of which only two design types have modern worldwide recognition and distribution: a prosthesis with one folding round disk (Fig. 1) and a prosthesis with two wings in the shape of a semicircle (Fig. 2-1, Fig. 2-2 ).
| Fig. 1 Domestic single-disk prosthesis “LIKS-2” | Fig. 2-1 Domestic double-leaf prosthesis “Carbonics-1” | Fig. 2-2 Bicuspid prosthesis from Sulzer Carbomedics (USA) |
Implantation of mechanical prostheses from a very early stage was accompanied by frequent cases of the development of cerebral circulatory disorders with deep disability of patients or their death, and therefore the main condition for the life of a patient with a mechanical prosthesis was developed - taking drugs that disrupt the blood coagulation process by reducing the production of coagulation proteins in liver. Targeted selective suppression of liver function for this purpose was achieved by prescribing specific substances to the patient - coumarin derivatives. Treatment with coumarin derivatives refers to the so-called anticoagulant therapy, and the substances themselves are called indirect anticoagulants. Several decades of use of mechanical prostheses have not produced as satisfactory results as expected, regardless of the model of the prosthesis. The main problem after their implantation remains the high incidence of circulatory disorders in organs, including the brain, due to the separation of small blood clots from the synthetic moving parts of the prosthesis, the possibility of the formation of which exists even with diligent and excessive anticoagulant therapy. On the other hand, drug-induced aggravation of blood coagulation disorders increases the risk of bleeding of various locations, often fatal. Therefore, in patients with stomach and duodenal ulcers, severe hypertension with the risk of cerebral hemorrhages, etc., the use of anticoagulants is very dangerous.
At present, we can say with confidence that attempts to modify the mechanisms of fastening the valves of mechanical prostheses, giving them mobility, creating a prosthesis from flexible synthetic structures, etc. have completely exhausted their capabilities in reducing the incidence of thromboembolic circulatory disorders, and the use of anticoagulant therapy with all its possible complications is mandatory for any mechanical prosthesis.
Having exhausted the reserves for changing the models of mechanical prostheses in relation to reducing circulatory disorders, researchers and clinicians are trying to find ways to precisely control the action of indirect anticoagulants in the hope of being able to deepen anticoagulant therapy while minimizing the complications of the latter. Since the mid-80s, in the countries of Western Europe and North America, there has been a laboratory testing system for all reagents to perform an analysis of the depth of anticoagulant therapy (reagents for determining the so-called prothrombin index, time, ratio) in comparison with the World Health Organization standard ( WHO). Reagents whose sensitivity differs from the WHO standard by more than 20% are considered unsuitable for use. The remaining reagents are used with a correction factor to determine the modern form of expression for prothrombin time - the International Normalized Ratio (INR).
Finally, manufacturers of mechanical prostheses have created personal coagulometers based on the determination of INR using strips with dry reagents. The patient himself or with the help of relatives takes blood by piercing the fingertip, applies a drop of blood to a certain place on the strip with reagents, and then inserts the strip into the device, on the screen of which after 30-60 seconds. The INR value is given.
In the cardiac surgical literature, the impact of new methods of monitoring therapy with indirect anticoagulants on the incidence of cerebrovascular accidents and the life expectancy of patients with mechanical prostheses in general is now being assessed with hope.
From the above, we can conclude that despite all the measures taken, thrombus formation on a mechanical prosthesis remains highly probable, and anticoagulant therapy, which is unsafe in itself, is mandatory for a patient with any mechanical prosthesis.
Now let’s evaluate the Russian living conditions of a patient with mechanical prostheses.
Domestic single-disk prostheses are quite reliable and have shown a low frequency of breakdowns in the human body during long-term operation, which cannot be said about double-leaf domestic models, the dysfunction of which is of a purely technical nature (loss or fragmentation of the valves) is associated with a series of scandalous lawsuits in the mid-90s . Such breakdowns are clinically extremely difficult, and if the patient is far from a specialized cardiac surgery center, death is likely in almost 100% of cases. In fairness, it should be noted that all the world's major manufacturers of mechanical prostheses did not avoid cases of technical breakdowns of their models, although the frequency of their occurrence was low.
As for the problems of blood clotting on a prosthesis, all of the above points can be completely transferred to our Russian prostheses, but with some national characteristics, which are outlined below.
Firstly, in Russia there are real difficulties in accurately determining the prothrombin test in one form or another due to the purchase by hospitals of a wide variety of reagents, often very far from WHO standards. There is a vicious practice of long-term storage of the prepared reagent in order to save money, as a result of which the digital expression of the prothrombin test completely misinforms both the patient and the attending physician. The definition of the modern form of expression for prothrombin time, i.e. INR is performed in even fewer laboratories in the country. As a result, reliable analysis can be obtained only in hospitals where heart operations are performed and great attention is paid to verification of the technique. The second feature follows from this.
Secondly, if we consider that there are only a few dozen such hospitals and centers in Russia, then one can imagine the obstacles in obtaining analysis, which are of a territorial nature.
Thirdly, indirect anticoagulants are not produced in Russia. Among the inexpensive drugs, there is the drug phenylin produced by the Kharkov Chemical Pharmaceutical Plant (KCP) and the Tallinn CPZ. Despite the same dosage, the effect of the drugs is noticeably different. Moreover, we noticed differences between different series of the drug from the same plant. All this again requires bringing the patient closer to a laboratory that can assess the effect of taking the drug. Fortunately, the highly standardized indirect anticoagulant warfarin from Nycomed is now on sale in Russia, and individual coagulometers from Sulzer are also imported into Russia, but the cost of these products is incomparable with the above-mentioned drugs, and they are inaccessible to most Russians.
Fourthly, the awareness of provincial Russian doctors about the principles of therapy with indirect anticoagulants is completely insufficient. Our practice provides many examples of a doctor’s complete misunderstanding of how the results of the analysis and the dosage of the drug relate, what tactics to choose when performing surgical procedures in a patient taking indirect anticoagulants, etc. As a result, the patient himself must have a deep understanding of this subject, i.e. The principle that works is “saving drowning people is the work of the drowning people themselves.”
Over the years of mechanical prosthetic fascination, years of hope and disappointment, cardiac surgery has advanced, reducing and reducing the mortality associated with the operation, with the result that repeated cardiac surgery has become commonplace, performed with risks no different from the initial operation.
In the new conditions, it is necessary to reassess our views on valve prosthesis, which consists in the fact that the quality of life of a patient with a prosthesis should be more significant for us than the fear of a second operation, that the apparent reliability and durability of a mechanical prosthesis results in the replacement of one disease with another, sometimes more more dangerous than the first. That is why we offer patients to return to implantation of prostheses made from biological tissues. These prostheses do not require therapy with indirect anticoagulants, modern methods of processing biological tissue make it possible to ensure normal operation of the prosthesis for up to 10-12, and sometimes up to 20 years, the biological degradation of the prosthesis occurs gradually, without the occurrence of critical situations, like a natural human valve affected by a pathological process. Let's look at the instructions for the biological prosthesis Sulzer Mitroflow Synergy in the “Indications” section: “... the valve is proposed for use in those patients who do not want long-term anticoagulant therapy for various reasons, such as living in remote areas, the presence of diseases of the gastrointestinal tract or other potential sources of bleeding in whom surgery in other areas is expected, in elderly patients, and in other situations where difficulties in anticoagulant therapy are expected for social or medical reasons.” Are there any patients who are candidates for implantation of a mechanical prosthesis? Who can know what awaits a patient with a mechanical prosthesis in the future, whether he will develop a stomach ulcer, whether he will need surgery, whether a young woman will want to give birth to a child? Life with a mechanical prosthesis is full of dangers and limitations.
That is why we have in our arsenal and offer patients a large selection of valve replacements created from biotissues. Among them are xenoarterial (Fig. 3) and xenopericardial (Fig. 4) prostheses from the Brazilian company BRAILE, biological prostheses from Sulzer (Fig. 5-1), (Fig. 5-2), and domestic bioprostheses "KemKor" (Kemerovo) (Fig. 6) and, finally, donor homografts of the original production (Fig. 7).
| Rice. 3 Biological xenoaortic prosthesis BRAILE (Brazil) | Fig.4 Biological xenopericardial prosthesis BRAILE (Brazil) | Rice. 5-1 Biological xenopericardial prosthesis Mitraflow Synergy (USA) |
| Rice. 5-2 Biological xenoaortic prosthesis “LABCOR” (USA) | Fig.6. Domestic biological xenoaortic prosthesis “KemKor” | Fig.7 Homoaortic graft (homograft, allograft) |
2.Stages of operation
At the first stage
the patient is connected to cardiac monitors, the chest is processed, breathing tubes are inserted from an artificial respiration apparatus, which is connected only after the anesthesia begins to take effect (i.e., the only discomfort for the patient may be some soreness and soreness in the throat after the operation).
The anesthesiologist puts the patient under general anesthesia. From this moment on, the patient does not feel anything.
An ultrasound device is placed through the esophagus into the heart area, transmitting an image of the heart to a monitor throughout the operation.
Second phase
- This is the opening of the chest. After marking, the heart surgeon makes an incision on the chest from the top of the rib cage to the navel. With the minimally invasive method, the incision length is two-thirds shorter.
The purpose of the third stage
is connection to a machine that provides artificial blood circulation. During the operation, the blood is enriched with oxygen outside the lungs, then it returns to the aorta and moves through the systemic circulation.
At this stage, the surgeon stops the heart, washes it and places it in a special solution that maintains its viability outside the circulation.
Fourth and fifth stages
- This is actually replacing the valve. The aorta is cut and the diseased valve is removed. If part of the aorta is also affected, it is also removed and a graft is placed. The valve hole is measured to select a new valve of the required size. The new valve is sewn on, then it is necessary to check that there are no leaks through it.
Sixth stage
- this is a disconnection from the artificial blood circulation machine. The aorta is sutured, and the trapped air is removed from the heart cavity. The heart begins to beat under the current of its own blood. If an uneven rhythm is observed, an electric shock is applied, which restores an even pulse.
Seventh stage
- chest closure. The bones and tissues are stitched together, and the sternum is closed with a suture that remains visible for life.
The entire operation usually lasts from 2 to 5 hours.
is important for the outcome of treatment .
It starts in the intensive care ward. Discharge from the hospital occurs 5-9 days after surgery. Postoperative rehabilitation continues on an outpatient basis.
Visit our Cardiology page
Consequences and rehabilitation in the postoperative period
After the operation, the patient is in the intensive care unit. Doctors monitor the patient’s condition, as negative consequences are possible and he will need rehabilitation . On the first day, there may be complications such as internal bleeding, thromboembolism, cardiac arrhythmias, infective endocarditis, and heart attack (in less than 5% of cases). After two days, the patient is allowed to get up and walk. At this time, he may complain of chest pain and increased fatigue. The patient is discharged home within 4 to 10 days, where he is under the supervision of a doctor.
The postoperative period lasts 3 weeks, during which temporary disturbances in sleep, vision, appetite, and swelling of the legs are possible. A month later the patient undergoes a full examination. The cardiologist calculates adequate physical activity, diet, and prescribes supportive treatment. It is important to perform physical therapy to strengthen the heart muscle.
Causes of heart valve defects
Heart valve defects in adults are diseases that are based on disorders of the valve apparatus (valve leaflets, annulus fibrosus, chordae, papillary muscles), congenital or developed as a result of diseases and injuries, disrupting proper blood flow through the valves and leading to serious complications, such such as severe heart failure, syncope, arrhythmias, sudden cardiac death, etc.
Stenosis is a narrowing of the valve opening for various reasons, as a result of which the heart has to work excessively to overcome this obstacle.
Valve insufficiency is a malfunction of the valve leaflets, leading to their incomplete closure and the return of blood back into the heart chamber, which leads to the heart working with excess blood volume.